Ask an expert self diagnose atopic dermatitis. This comprehensive guide delves into the intricacies of atopic dermatitis (AD), providing a crucial understanding of its symptoms, triggers, and the limitations of self-diagnosis. We’ll explore the crucial difference between self-assessment and a professional diagnosis, equipping you with the knowledge to make informed decisions about your health.
From understanding the various presentations of AD across different age groups to exploring potential misconceptions, this resource is your one-stop shop for navigating the complexities of this common skin condition. We’ll also discuss the emotional impact of AD and offer strategies for coping with the associated challenges. Learn about the diagnostic process, self-assessment tools, and even basic management strategies.
This is not a substitute for professional medical advice, but rather a supportive resource to enhance your understanding.
Introduction to Atopic Dermatitis

Atopic dermatitis (AD), often called eczema, is a chronic inflammatory skin condition characterized by itchy, dry, and inflamed skin. It’s a prevalent condition affecting individuals of all ages, though its presentation and triggers can vary significantly across different life stages. Understanding the nuances of AD, including its symptoms, triggers, and severity levels, is crucial for effective management and treatment.This chronic skin condition is frequently associated with a predisposition to other allergic conditions like asthma and hay fever, highlighting the interconnectedness of the immune system and skin health.
Its impact extends beyond the physical discomfort, often affecting a person’s emotional well-being and quality of life.
Common Symptoms of Atopic Dermatitis
AD manifests in various ways, with presentations differing significantly depending on the age group. The characteristic symptoms often include dry, itchy skin, which can range from mild dryness to intense, persistent itching. Inflammation can result in redness, swelling, and scaling.
- Infants: Infants often exhibit AD as erythematous (reddened) patches, especially on the face, scalp, and extensor surfaces of the extremities. The skin may appear cracked and weepy, leading to potential secondary infections. A characteristic symptom in infants is often a rash on the cheeks and forehead, which is often more severe than in later childhood or adulthood.
- Children: As children grow, the locations of affected areas can shift. The skin may appear scaly, dry, and thickened. In children, AD frequently affects the creases of the elbows and knees, as well as the wrists, ankles, and face. The itching can be particularly intense, disrupting sleep and daily activities.
- Adults: Adults with AD may experience persistent dryness, itching, and inflammation, often concentrating on the hands, feet, and inner elbows. Skin thickening and lichenification (a leathery appearance) are more common in adults compared to children. Scratching can lead to skin discoloration and visible scars.
Triggers and Contributing Factors
Identifying triggers and contributing factors is essential for managing AD. Several factors can exacerbate the condition.
- Environmental Factors: Exposure to irritants like harsh soaps, detergents, and wool fabrics can worsen AD symptoms. Dry air, especially during winter months, can contribute to skin dryness and increased itching.
- Allergies: Allergens like pollen, dust mites, pet dander, and certain foods can trigger or worsen AD in susceptible individuals. Identifying and avoiding these triggers is critical for managing the condition.
- Stress: Stress can have a significant impact on the immune system, potentially exacerbating skin inflammation and itching in individuals with AD. Stress management techniques can be beneficial.
Comparing Mild, Moderate, and Severe Cases of Atopic Dermatitis
| Severity | Symptom Description | Severity Level |
|---|---|---|
| Mild | Occasional, localized itching and redness; minimal skin dryness; infrequent flares. | Low |
| Moderate | More frequent itching and redness; noticeable skin dryness; flares lasting several days to weeks; involvement of larger areas of the body. | Medium |
| Severe | Intense itching and inflammation; widespread skin involvement; severe skin dryness; frequent and prolonged flares; significant impact on daily activities; potential for secondary skin infections. | High |
Differentiating Atopic Dermatitis from Other Skin Conditions
| Condition | Key Differences |
|---|---|
| Atopic Dermatitis (AD) | Chronic, itchy, dry skin; often associated with allergies and asthma; typically presents with erythematous, scaly, and/or weepy skin lesions. Symptoms can fluctuate. |
| Eczema | General term for inflammatory skin conditions; can share some characteristics with AD but can also have different presentations; not always associated with allergies or asthma; symptom presentation can vary widely. |
| Psoriasis | Chronic autoimmune skin condition; characterized by silvery-white plaques; typically not as itchy as AD; lesions tend to be well-defined and thicker. Lesions tend to be more stable and less variable. |
Self-Diagnosis Considerations
Self-diagnosing atopic dermatitis (AD) can be tempting, especially when dealing with persistent skin irritation. However, understanding the limitations of self-diagnosis is crucial for proper management and avoiding potentially harmful delays in seeking professional care. Accurate diagnosis requires a comprehensive evaluation by a healthcare professional.A thorough understanding of the nuances of AD, including its various presentations and potential triggers, is essential to differentiate it from other skin conditions.
The skin manifestations of AD can mimic those of other dermatological issues, highlighting the need for expert assessment to rule out alternative diagnoses. Incorrect self-diagnosis could lead to inappropriate treatments, exacerbating the condition or missing a more serious underlying issue.
Limitations of Self-Diagnosis for AD
Self-diagnosis of AD, while seemingly convenient, often lacks the depth and precision of a professional evaluation. A doctor can consider a patient’s complete medical history, conduct a thorough physical examination, and order necessary tests to confirm the diagnosis and rule out other possibilities. This holistic approach is essential for effective management of AD. Crucially, self-diagnosis cannot account for the interplay of genetic predisposition, environmental factors, and other medical conditions that can influence the development and progression of AD.
Importance of Consulting a Healthcare Professional
Seeking professional medical advice for AD is paramount for accurate diagnosis and appropriate treatment. A healthcare provider can perform a comprehensive evaluation, including a detailed history and physical examination. This evaluation helps to distinguish AD from similar skin conditions, such as psoriasis, eczema, or contact dermatitis. Furthermore, a healthcare professional can identify potential underlying causes or contributing factors that might be overlooked in a self-diagnosis.
Red Flags Indicating Immediate Professional Consultation
Certain symptoms or situations warrant immediate consultation with a dermatologist or allergist. These “red flags” include:
- Rapidly worsening skin condition, with significant increase in itching, inflammation, or spreading of lesions.
- Presence of secondary infections, such as bacterial or fungal infections, evidenced by pus, crusting, or fever.
- Significant pain or discomfort associated with the skin lesions, beyond the typical itching.
- Presence of skin lesions accompanied by fever, chills, or other systemic symptoms.
- Appearance of skin lesions in unusual locations, particularly if accompanied by other concerning symptoms.
Prompt professional attention is crucial in such cases to address potential complications or underlying medical conditions.
Key Differences Between Self-Diagnosis and Professional Diagnosis
| Characteristic | Self-Diagnosis | Professional Diagnosis |
|---|---|---|
| Information Source | Limited to personal observations and potentially inaccurate information from online resources. | Comprehensive medical history, physical examination, and potentially diagnostic tests. |
| Diagnostic Accuracy | Potentially inaccurate and prone to misdiagnosis. | High accuracy based on expert knowledge and evidence-based methods. |
| Treatment Plan | Potentially inappropriate or ineffective treatment based on inaccurate understanding of the condition. | Tailored treatment plan considering individual needs and medical history. |
| Management of Complications | Inability to identify or manage complications or underlying medical conditions. | Ability to identify and manage potential complications and underlying conditions. |
| Ongoing Monitoring | Limited ability to track the progression of the condition or adjust treatment. | Regular monitoring and adjustments to treatment as needed. |
Medical expertise is critical in accurately diagnosing and managing atopic dermatitis.
Potential Misconceptions About AD
Common misconceptions about AD can lead to incorrect self-diagnosis and inappropriate treatment.
Figuring out if you have atopic dermatitis can be tricky, but asking an expert is key. While researching different treatments, you might also stumble across information on inhaler colors – what do they mean? Knowing the specifics of inhaler colors, like those found on inhaler colors what do they mean , can be helpful, but ultimately, seeking professional advice for a proper atopic dermatitis diagnosis is the best approach.
- AD is solely caused by allergens. While allergens can trigger flares, AD is a complex condition with multiple contributing factors, including genetics and environmental triggers.
- AD is easily cured with topical creams. While topical treatments are important, AD often requires a multifaceted approach including lifestyle modifications, and potentially systemic medications.
- AD is only a childhood condition. While it can start in childhood, AD can persist into adulthood and present differently in adults.
- AD is contagious. Atopic dermatitis is not contagious; it’s a chronic skin condition.
Careful consideration and clarification of these misconceptions are vital to ensure accurate self-assessment and appropriate medical intervention.
Understanding the Diagnostic Process: Ask An Expert Self Diagnose Atopic Dermatitis
Figuring out if you have atopic dermatitis (AD) involves a careful process where healthcare professionals use various methods to gather information and make an accurate diagnosis. This isn’t a quick guess; it’s a comprehensive evaluation that takes into account your medical history, physical appearance, and sometimes, further tests. A proper diagnosis ensures you receive the right treatment tailored to your specific needs.The diagnostic journey begins with a detailed conversation about your symptoms, medical history, and lifestyle.
This crucial step helps healthcare providers pinpoint potential contributing factors and understand the nuances of your condition. The physical examination, along with a thorough review of your symptoms, helps paint a clearer picture of your AD.
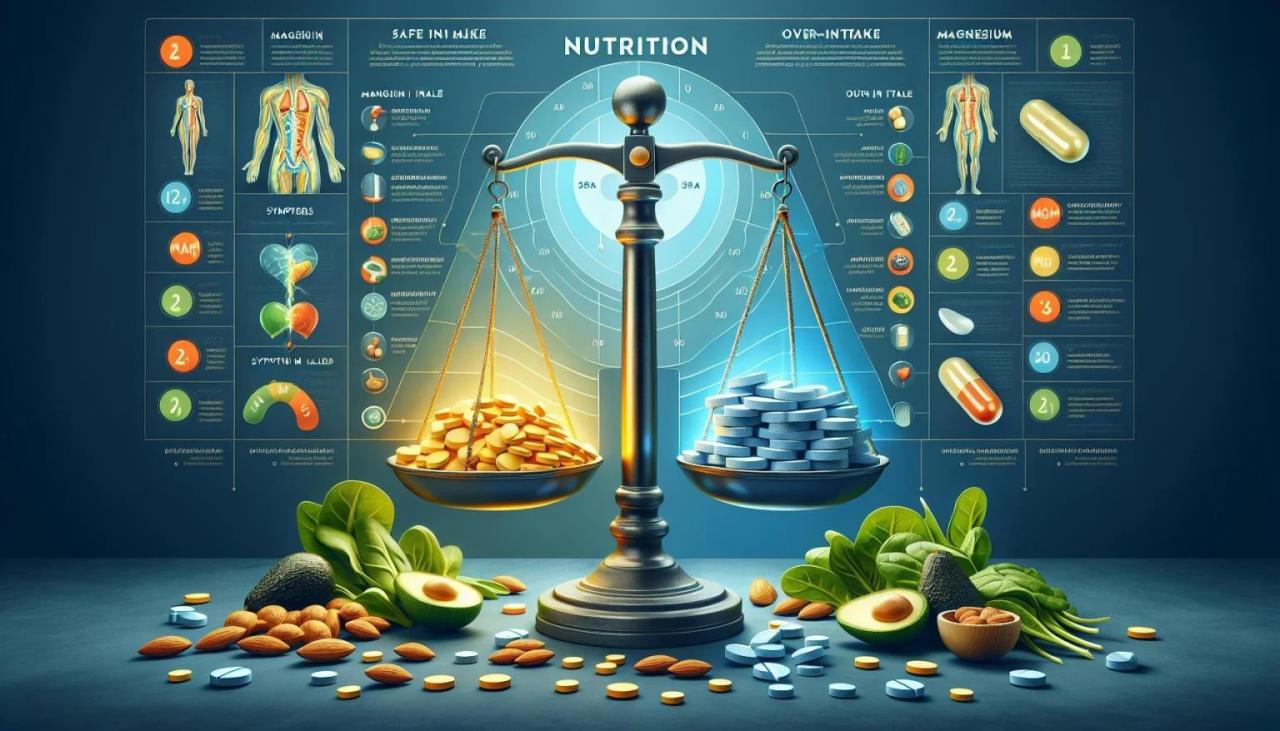
Figuring out if you have atopic dermatitis can be tricky, so asking an expert is key for self-diagnosis. But sometimes, underlying issues like consuming excessive protein might be contributing to the problem. Understanding the potential signs of too much protein could shed light on your skin condition. Ultimately, consulting a dermatologist remains the best course of action for accurate diagnosis and personalized treatment for atopic dermatitis.
Common Methods Used by Healthcare Professionals, Ask an expert self diagnose atopic dermatitis
Healthcare professionals employ several methods to arrive at an AD diagnosis. These methods include evaluating a patient’s medical history, performing a physical examination, and potentially ordering additional tests. A thorough understanding of these methods is key to a successful diagnostic journey.
- Patient History Evaluation: This involves a detailed discussion about your symptoms, including their onset, duration, frequency, location, and any triggers. Questions about your family history of allergies or eczema are also crucial. The more information you provide, the better the healthcare professional can understand your specific situation and determine the likelihood of AD.
- Physical Examination: The physical examination focuses on the skin, specifically looking for characteristic features of AD. This includes observing the distribution, intensity, and type of skin lesions. The healthcare professional will also look for signs of other conditions that might mimic AD, such as psoriasis or contact dermatitis. Visual assessment is crucial, as it provides important clues about the nature and severity of the condition.
- Diagnostic Tests: In some cases, further tests may be necessary to confirm the diagnosis or rule out other conditions. These tests can include skin biopsies, which involve taking a small sample of skin tissue for microscopic examination. Another example is patch testing, which helps identify potential allergens that might be triggering the eczema.
Diagnostic Approach for Different Age Groups
The diagnostic approach can vary slightly depending on the age of the patient. For infants and young children, the focus is often on the characteristic skin lesions, family history, and the presence of other allergic conditions. For adults, the diagnostic process might involve a more comprehensive evaluation, including considering potential lifestyle factors and other contributing conditions.
Figuring out atopic dermatitis can be tricky, so seeking expert advice is key. Learning about potential self-diagnosis methods is helpful, but remember that accurate diagnoses often involve professionals. While exploring different treatment options, it’s crucial to be mindful of potential interactions, like how some CBD oil products can sometimes lead to issues with drug tests. For more information on this topic, check out this helpful resource on cbd oil and failing drug tests.
Ultimately, consulting a dermatologist or other qualified healthcare provider is the best way to ensure a proper diagnosis and treatment plan for atopic dermatitis.
- Infants and Children: Diagnosing AD in infants and young children often relies heavily on the characteristic skin lesions, especially in areas like the face, neck, and extensor surfaces. Family history of allergies is also a significant factor. Due to the limited verbal communication of young patients, reliance on observation of skin changes and parental input is essential.
- Adults: The diagnostic process in adults might involve considering a broader range of potential causes for skin conditions, including stress, environmental factors, and other medical conditions. A detailed history about potential triggers and lifestyle factors is essential. In adults, a comprehensive assessment of potential underlying conditions is crucial.
Self-Assessment Tools and Resources
Taking the first step towards understanding your skin condition can be empowering. Self-assessment tools can help you identify potential symptoms and triggers, providing valuable insights to share with a healthcare professional. This process isn’t a replacement for a proper diagnosis, but it can be a helpful starting point for understanding your body and how to manage your atopic dermatitis (AD).
Self-Assessment Questionnaire for Atopic Dermatitis Symptoms
This questionnaire aims to help you identify the patterns of your AD symptoms. Answering honestly will provide a more accurate reflection of your condition.
- Frequency of itching: How often do you experience itching? (e.g., constantly, several times a day, occasionally). The frequency of itching can vary greatly depending on the severity and stage of the condition.
- Location of rash: Where on your body does the rash typically appear? (e.g., face, hands, legs, behind the knees). Identifying specific areas affected can be useful for understanding potential triggers or patterns.
- Rash characteristics: Describe the appearance of the rash. (e.g., dry, red, scaly, inflamed, weepy). These details can aid in distinguishing AD from other skin conditions.
- Severity of rash: How severe is the rash? (e.g., mild, moderate, severe). Severity is often measured by the area affected, the intensity of inflammation, and the presence of secondary infections.
- Time of onset: When did the rash first appear? (e.g., childhood, adulthood, after a specific event). Understanding the onset can help identify potential triggers.
- Triggers: Are there any specific situations, materials, or environmental factors that seem to worsen your symptoms? (e.g., stress, weather changes, certain fabrics). Identifying triggers is essential for managing the condition.
Checklist for Identifying Potential Atopic Dermatitis Triggers
This checklist helps you identify potential triggers that may be contributing to your AD symptoms.
- Environmental factors: Dry air, extreme temperatures, changes in humidity, pollution, or certain weather conditions.
- Irritants: Soaps, detergents, harsh chemicals, perfumes, dyes, or certain fabrics.
- Foods: Certain foods, such as nuts, dairy, eggs, or soy.
- Allergens: Dust mites, pollen, pet dander, mold, or other allergens.
- Stress: Stressful life events or situations.
- Hygiene products: Certain soaps, shampoos, or lotions.
- Infections: Viral, bacterial, or fungal infections.
Reliable Online Resources for Atopic Dermatitis Information and Support
Reliable online resources can provide helpful information and support for managing AD.
- National Eczema Association (NEA): Provides comprehensive information, support groups, and resources for individuals with AD.
- American Academy of Dermatology (AAD): Offers evidence-based information on AD, including diagnosis, treatment, and management.
- Mayo Clinic: Provides detailed information on AD, including symptoms, causes, and treatment options.
- Johns Hopkins Medicine: Offers a wealth of information on AD, including research updates and expert opinions.
Patient Education in Managing Atopic Dermatitis
Patient education plays a crucial role in managing AD symptoms effectively. Understanding the condition, its triggers, and appropriate management strategies empowers individuals to take control of their health. This includes learning about potential triggers, self-care strategies, and the importance of communication with healthcare professionals.
Key Features of Self-Assessment Tools
| Tool | Strengths | Weaknesses |
|---|---|---|
| Symptom Questionnaire | Identifies patterns, frequency, and location of symptoms. | Not a substitute for professional diagnosis. |
| Trigger Checklist | Helps identify potential irritants and allergens. | May not capture all individual triggers. |
| Online Resources | Provides access to reliable information and support networks. | Information quality can vary; always consult a professional. |
Addressing Common Concerns
Living with atopic dermatitis (AD) can be challenging, impacting not just your physical well-being but also your emotional health. The constant itch, unpredictable flare-ups, and potential social stigma can lead to significant stress and anxiety. Understanding these emotional dimensions of AD is crucial for effective self-management.
The Emotional Toll of Atopic Dermatitis
Atopic dermatitis often affects self-esteem and body image. The persistent itching and visible skin changes can lead to feelings of embarrassment, self-consciousness, and isolation. Individuals with AD may experience frustration, anxiety, and even depression due to the unpredictable nature of the condition and the limitations it can impose. This emotional burden can significantly impact quality of life, making it essential to address these concerns alongside the physical aspects of the condition.
Managing Stress and Anxiety Related to AD
Stress and anxiety are common companions for those with atopic dermatitis. Identifying and managing stress triggers is vital for reducing flare-ups and improving overall well-being. Techniques like mindfulness, deep breathing exercises, and progressive muscle relaxation can help to calm the nervous system and reduce anxiety. Regular physical activity, a balanced diet, and sufficient sleep also play a crucial role in managing stress and supporting emotional health.
Furthermore, seeking professional help from a therapist or counselor specializing in stress management can provide personalized strategies and support.
Coping Strategies for AD Symptoms
Developing effective coping mechanisms is essential for managing the symptoms of atopic dermatitis. These strategies should address both the physical and emotional aspects of the condition. Strategies may include:
- Maintaining a consistent skin care routine, using gentle cleansers and moisturizers, and avoiding harsh soaps or irritants.
- Practicing stress-reduction techniques like meditation, yoga, or spending time in nature.
- Seeking support from friends, family, or support groups.
- Educating oneself about AD to better understand triggers and develop strategies for managing flare-ups.
Implementing these coping strategies can lead to improved emotional regulation and a greater sense of control over the condition.
Support Groups for Individuals with Atopic Dermatitis
Connecting with others who understand the challenges of living with atopic dermatitis can provide invaluable support and a sense of community. Support groups offer a safe space to share experiences, learn coping strategies, and receive encouragement from others facing similar struggles. These groups can also provide access to valuable information and resources. They are crucial for building resilience and fostering a sense of belonging among individuals with AD.
Resources for Emotional Support and Mental Health Services
The following table provides a starting point for accessing resources for emotional support and mental health services related to skin conditions like atopic dermatitis:
| Resource Type | Examples |
|---|---|
| Support Groups | Local AD support groups, online forums, and online support communities |
| Mental Health Professionals | Therapists, counselors, and psychologists specializing in stress management and anxiety disorders |
| Online Mental Health Resources | Websites offering self-help tools, articles, and educational materials on stress management and mental health |
| Community Health Centers | Community health centers offering affordable mental health services |
| National Mental Health Organizations | National Alliance on Mental Illness (NAMI), MentalHealth.gov |
Accessing these resources can provide crucial support in managing the emotional aspects of atopic dermatitis.
Illustrations and Visual Aids
Visual aids play a crucial role in accurately identifying and understanding atopic dermatitis (AD). By visualizing the various presentations of AD, you can gain a better understanding of the condition and improve communication with healthcare professionals. This section will detail how to differentiate AD from other skin conditions, showcase various AD presentations, and explain the importance of visual documentation.Accurate self-assessment and effective communication with dermatologists rely heavily on visual depictions of the skin condition.
This allows for a more comprehensive understanding of the problem and aids in the diagnosis process. Visual aids are crucial tools in this journey.
Appearance of AD Skin Lesions in Different Stages
AD skin lesions manifest in diverse ways across different stages. Early stages often present with dry, flaky skin, particularly on the folds of the skin, like the elbows, knees, or neck. These dry patches may appear slightly red or irritated. As the condition progresses, the skin may become more inflamed, with the development of small, intensely itchy bumps or blisters.
These blisters may ooze fluid, resulting in weeping lesions. In chronic cases, the skin may appear thickened and leathery, with lichenification (thickened, roughened skin). The appearance of these lesions can vary significantly depending on the individual and the specific triggers.
Differentiating AD from Other Skin Conditions Visually
Differentiating AD from other skin conditions visually requires careful observation of the lesions’ characteristics. While eczema and psoriasis may share some overlapping features, key differences exist. For example, psoriasis often presents with silvery-white scales, which are not typical of AD. Eczema can manifest with weeping or crusted lesions, but the distribution and overall appearance may differ from AD.
Additionally, the location of the lesions can offer clues. AD frequently affects the creases of the elbows and knees, as well as the face and neck. The history of the skin condition, including any known triggers, also plays a significant role in the differentiation process. Proper visual documentation helps in accurately communicating the condition to a healthcare professional.
Techniques for Taking Pictures of Skin Lesions
Visual documentation is crucial for accurate diagnosis. Taking clear and informative photographs of your skin lesions can significantly assist healthcare providers in evaluating your condition. When taking pictures, ensure the lighting is natural and even. Avoid using flash, as it can distort the appearance of the lesions. Take pictures from multiple angles, showing the affected area’s extent and the characteristics of the lesions (e.g., redness, scaling, weeping).
Include images of both the affected area and unaffected areas to provide context. The pictures should clearly show the location, shape, size, and color of the lesions. Ensure you capture the texture and any accompanying symptoms.
Examples of AD Presentations
AD presentations can vary considerably. A common presentation involves dry, flaky skin, often appearing as small, white or slightly pink scales, especially on the flexural areas of the body. Another presentation is weeping lesions, characterized by oozing blisters, often accompanied by redness and inflammation. Sometimes, the lesions may appear as red, inflamed patches with small, itchy bumps, which are commonly seen in acute AD flares.
The exact presentation will vary based on individual factors and the severity of the condition.
Significance of Visual Aids in Self-Assessment and Communication
Visual aids, such as photographs, are essential for both self-assessment and communication with healthcare providers. By documenting the appearance of your skin lesions over time, you can track the progression of the condition and identify potential triggers. This detailed documentation aids in understanding the pattern of AD flares. Sharing these images with your dermatologist allows them to accurately assess the severity, type, and location of the lesions, leading to a more precise diagnosis and personalized treatment plan.
This also allows for better communication and understanding between you and your doctor.
Management Strategies (Basic Overview)
Managing atopic dermatitis (AD) is a multifaceted process that involves a combination of strategies. It’s crucial to understand that there’s no one-size-fits-all approach, and the best management plan is tailored to the individual’s specific needs and triggers. The core of effective AD management lies in maintaining skin hydration, preventing flare-ups, and addressing the underlying inflammatory response.
Skin Hydration and Barrier Repair
Maintaining a healthy skin barrier is paramount in AD management. Dry skin is a common trigger for flares. Regular moisturizing is essential to keep the skin’s protective layer intact. This helps to prevent water loss and keep the skin supple. Moisturizers should be applied frequently, especially after bathing or showering when the skin is most vulnerable.
Choosing the right moisturizer is important. Look for products that are fragrance-free, hypoallergenic, and formulated for sensitive skin. Consider occlusive moisturizers for severe cases.
Topical Treatments in Managing AD Symptoms
Topical treatments play a critical role in controlling AD symptoms. These treatments aim to reduce inflammation, soothe itching, and prevent infection. Common topical treatments include corticosteroids, which help reduce inflammation, and calcineurin inhibitors, which target the inflammatory response. The selection of a topical treatment depends on the severity and location of the AD. A dermatologist can provide personalized recommendations and guidance on appropriate usage and dosage.
Avoiding Triggers in Managing AD
Identifying and avoiding triggers is vital in preventing AD flare-ups. Triggers can vary greatly from person to person. Common triggers include certain fabrics, harsh soaps, strong detergents, allergens, and stress. Keeping a detailed diary of potential triggers and corresponding reactions can be extremely helpful in understanding patterns and developing preventive strategies. This awareness allows individuals to tailor their environment and habits to minimize exposure to these factors.
Summary of Common Topical Treatments
| Treatment Type | Description | Application |
|---|---|---|
| Corticosteroids | Reduce inflammation | Apply a thin layer to affected areas as directed by a healthcare professional. |
| Calcineurin Inhibitors | Target the inflammatory response | Apply a thin layer to affected areas as directed by a healthcare professional. Use with caution, as they can have side effects. |
| Moisturizers (Emollients) | Hydrate and repair the skin barrier | Apply frequently, especially after bathing or showering. |
| Antihistamines | Reduce itching | Taken orally, these can provide relief from severe itching. |
| Antibiotics | Treat secondary infections | Prescribed by a healthcare professional for skin infections. |
Conclusion

In conclusion, while self-assessment can be a helpful starting point, accurate diagnosis and effective management of atopic dermatitis always require expert consultation. This guide has provided a detailed overview of the condition, its various presentations, diagnostic considerations, and potential misconceptions. Remember, seeking professional medical advice is paramount. This resource aims to empower you with knowledge to better communicate with your healthcare provider and ultimately improve your well-being.

















 (Example image: A plate divided into sections, each representing a food group – fruits, vegetables, lean protein, and whole grains – with approximate proportions. The plate image is designed to visually represent the portion sizes required for a balanced meal.)
(Example image: A plate divided into sections, each representing a food group – fruits, vegetables, lean protein, and whole grains – with approximate proportions. The plate image is designed to visually represent the portion sizes required for a balanced meal.) (Example image: A flowchart illustrating the meal planning process. The steps might include identifying dietary needs, creating a shopping list, selecting recipes, and finally, preparing and consuming the meal.)
(Example image: A flowchart illustrating the meal planning process. The steps might include identifying dietary needs, creating a shopping list, selecting recipes, and finally, preparing and consuming the meal.) (Example image: A series of images showcasing healthy cooking methods like steaming, baking, grilling, and stir-frying. Each image could highlight the benefits of the method and show the food being prepared.)
(Example image: A series of images showcasing healthy cooking methods like steaming, baking, grilling, and stir-frying. Each image could highlight the benefits of the method and show the food being prepared.) (Example image: A collage of various healthy meals, including salads, stir-fries, soups, and baked dishes. The images showcase a variety of colors, textures, and food types, representing different cuisines.)
(Example image: A collage of various healthy meals, including salads, stir-fries, soups, and baked dishes. The images showcase a variety of colors, textures, and food types, representing different cuisines.) (Example image: A visual comparison of appropriate portion sizes for different food groups, perhaps using various sized bowls and plates to demonstrate the concept. The image should also include labels indicating the recommended portion sizes.)
(Example image: A visual comparison of appropriate portion sizes for different food groups, perhaps using various sized bowls and plates to demonstrate the concept. The image should also include labels indicating the recommended portion sizes.)