Are nightshades bad for arthritis? This question sparks debate among those seeking ways to manage arthritis symptoms. Nightshades, a diverse family including tomatoes, potatoes, peppers, and eggplants, are staples in many diets. However, some believe their consumption might exacerbate arthritis pain. This exploration delves into the potential link between nightshade consumption and arthritis, examining scientific…
Category: Health & Wellness
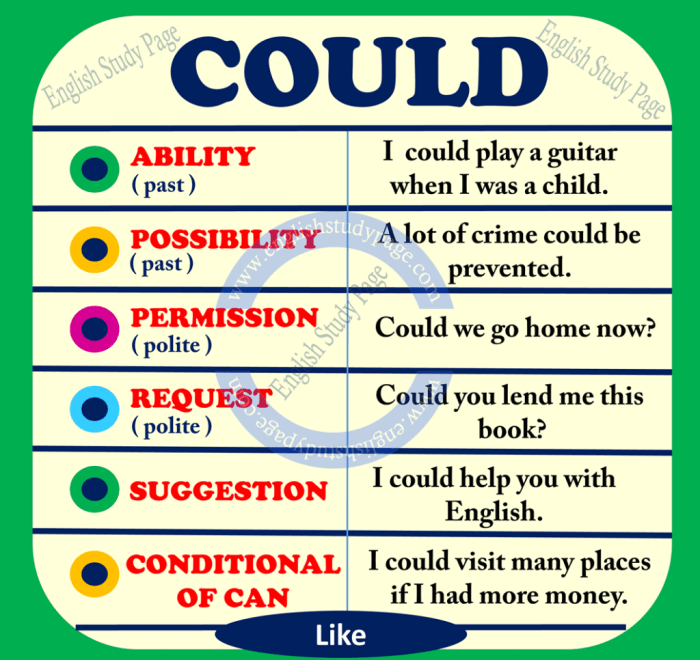
Could Prednisone Cause Mood Swings?
Could prednisone cause mood swings? This question delves into the potential link between the powerful corticosteroid prednisone and fluctuations in mood. Understanding how this medication impacts the body’s neurochemistry is crucial for patients and healthcare providers alike. This exploration investigates the mechanisms behind prednisone’s effect on various neurotransmitters, leading to potential mood changes. Prednisone, often…
Is It Bad to Sleep Right After Eating? A Deep Dive
Is it bad to sleep right after eating? This question is a common concern for many, and the answer isn’t a simple yes or no. Digestion is a complex process, and the timing of sleep after a meal can significantly impact its efficiency and overall health. This exploration delves into the science behind digestion, potential…
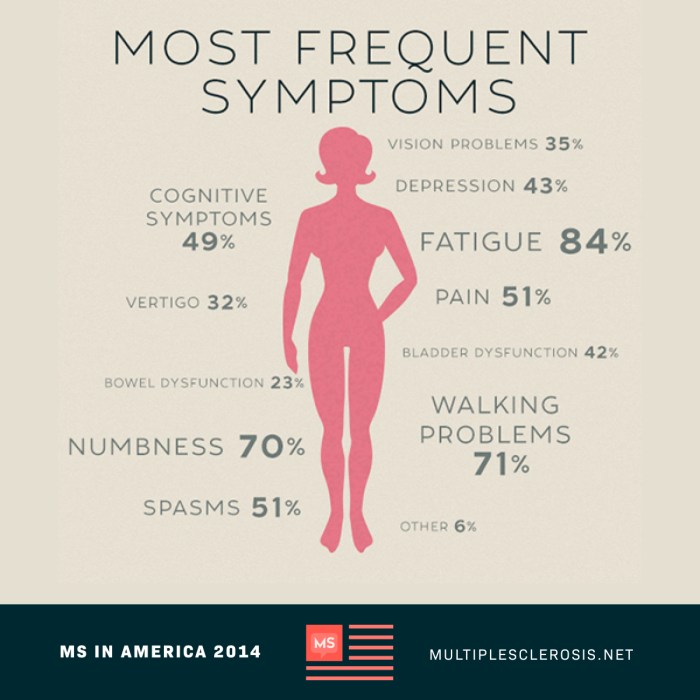
How MS Is Diagnosed A Comprehensive Guide
How MS is diagnosed is a multifaceted process, involving a combination of assessments, examinations, and procedures. This guide delves into the intricate steps healthcare professionals take to identify Multiple Sclerosis (MS), from initial symptom evaluation to advanced diagnostic techniques. Understanding this process is crucial for patients and their families as they navigate the complexities of…
What is the Death Rattle A Comprehensive Guide
What is the death rattle? This article delves into the intricacies of this often-misunderstood phenomenon, exploring its physical manifestations, physiological mechanisms, and the diverse medical conditions that can lead to it. We’ll uncover the common sounds, the role of the respiratory system, and how dehydration and muscle weakness play a part. Further, we’ll examine the…
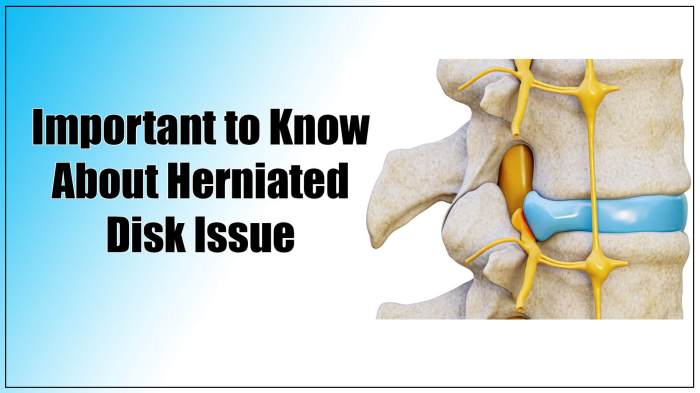
Herniated Disc Physical Therapy A Comprehensive Guide
Herniated disc physical therapy is a crucial aspect of managing and recovering from a herniated disc. It’s a personalized approach, focusing on restoring function, relieving pain, and improving overall well-being. This guide delves into the various facets of herniated disc physical therapy, from understanding the condition itself to exploring different treatment methods and patient education….
Prescription Medicine for Diarrhea-Predominant IBS
Prescription medicine for diarrhea predominant IBS offers a range of options for managing this challenging condition. Understanding the various medications, their mechanisms, and potential side effects is crucial for effective treatment. This guide delves into the specifics, providing insights into the role of antidiarrheal medications, and comparing different approaches to treatment. From common over-the-counter remedies…
Infected Belly Button Piercing A Comprehensive Guide
Infected belly button piercing: Understanding the causes, symptoms, and treatments is crucial for a speedy recovery. This guide delves into the complexities of piercing infections, providing a comprehensive overview of the factors that contribute to them and how to manage them effectively. From identifying the initial signs of infection to exploring various treatment options, we’ll…
Dosing Hydrocodone How Much Is Safe?
Dosing hydrocodone how much is safe? This crucial question is often at the forefront of pain management discussions. Understanding the proper dosage of hydrocodone is paramount to ensuring its effective use while minimizing potential risks. Hydrocodone, a commonly prescribed opioid, plays a vital role in pain relief, but its use carries inherent dangers. Proper administration,…
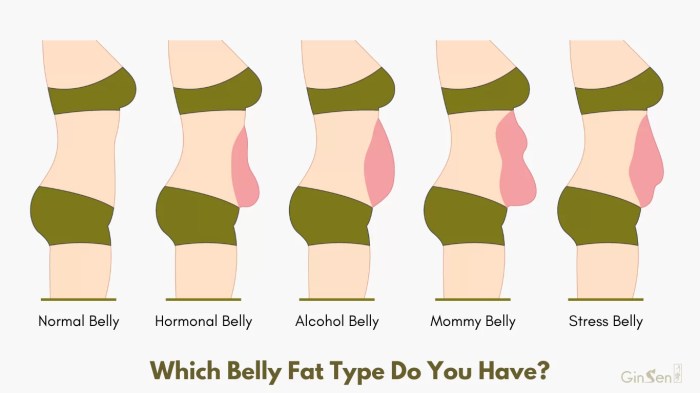
Obesitys Link to Cancer Risk Unveiling the Mechanisms
Why does obesity increase cancer risk? This exploration delves into the complex interplay between excess weight and the development of various cancers. We’ll uncover the physiological pathways, examine specific cancer types, and analyze obesity-related factors to understand how body composition influences cancer risk. From chronic inflammation to hormonal imbalances, we’ll unravel the intricate mechanisms behind…