What are the physical effects of sleep deprivation? This exploration delves into the immediate and long-term consequences of insufficient sleep, from reduced alertness to serious health risks. We’ll examine how sleep loss impacts various organ systems, physical performance, and even dietary habits. Understanding these effects is crucial for prioritizing sleep and maintaining overall well-being.
Sleep deprivation takes a toll on the body, impacting everything from our reflexes to our risk of chronic disease. From the short-term effects of a single sleepless night to the cumulative impact of chronic sleep loss, the consequences are significant and far-reaching. This detailed look at the topic will help readers understand the importance of prioritizing sleep for optimal physical health.
Short-Term Effects

Sleep deprivation’s immediate impact on the body is significant and multifaceted. From sluggishness and impaired judgment to physiological changes, the consequences of insufficient rest become readily apparent within hours of sleep loss. Understanding these short-term effects is crucial for appreciating the importance of adequate sleep in maintaining overall health and well-being.
Reduced Alertness and Impaired Reaction Time
The body’s natural state of alertness is directly correlated with the amount of sleep obtained. A lack of sleep significantly diminishes cognitive function, leading to decreased vigilance and impaired decision-making. Reduced alertness is particularly noticeable in tasks requiring sustained attention, such as driving or operating machinery. This decreased alertness can be directly attributed to the brain’s diminished capacity to process information efficiently.
Impaired reaction time is a further consequence, impacting the body’s ability to respond swiftly to stimuli. For example, a driver deprived of adequate sleep may have a significantly slower reaction time to sudden hazards, increasing the risk of accidents.
Physiological Changes in the Body
Within the first few hours of sleep loss, the body’s physiological processes begin to exhibit noticeable changes. These changes are often subtle but can accumulate and have significant consequences over time. Increased heart rate and blood pressure are common responses to sleep deprivation, reflecting the body’s heightened state of alert. The cardiovascular system works harder to maintain this state of readiness, placing extra strain on the heart and blood vessels.
Furthermore, hormone levels can fluctuate, impacting various bodily functions. This illustrates the interconnectedness of sleep and overall physical health.
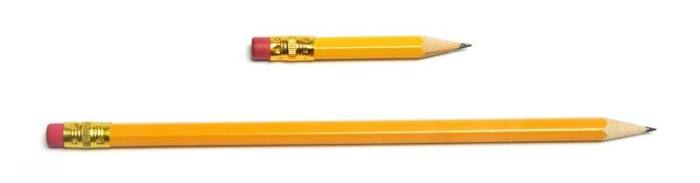
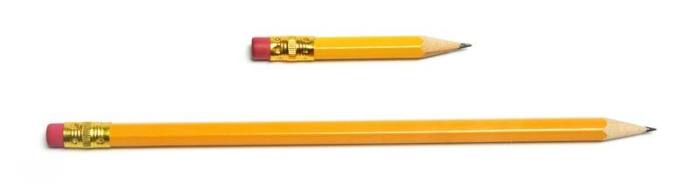
Comparison of Different Sleep Durations
The physical consequences of sleep deprivation vary significantly based on the duration of sleep loss. A person who gets only 4 hours of sleep will experience more pronounced effects compared to someone who gets 6 hours. The difference in performance is more pronounced in activities demanding sustained concentration or quick reflexes. For example, a task like driving a long distance or performing surgery requires significant alertness, and the body’s ability to maintain this alertness is directly related to the amount of sleep received.
Sleep deprivation can wreak havoc on your body, impacting everything from your immune system to your blood sugar levels. This is especially crucial after surgery, where a compromised immune response can lead to complications like infection, and fluctuating glucose levels can complicate recovery. Understanding how sleep affects post-operative health is vital, and factors like after surgery infection and glucose management are key.
Ultimately, prioritizing sleep is essential for overall physical health, regardless of surgery or other factors.
Eight hours of sleep provides the body with the necessary time to recover and replenish, leading to optimal physical performance and cognitive function. This contrast highlights the critical role of sufficient sleep in maintaining peak physical and mental performance.
Immediate Physical Effects of Sleep Deprivation
| Duration of Sleep Loss | Specific Physical Effect | Brief Description |
|---|---|---|
| 4 hours | Reduced Alertness | Diminished vigilance, impaired judgment, difficulty concentrating |
| 4 hours | Impaired Reaction Time | Slower response to stimuli, increased risk of accidents |
| 4 hours | Increased Heart Rate and Blood Pressure | Elevated cardiovascular strain, potential for cardiovascular complications |
| 6 hours | Reduced Alertness | Decreased attention span, increased susceptibility to errors |
| 6 hours | Impaired Cognitive Function | Difficulty in problem-solving and decision-making |
| 6 hours | Increased Stress Hormones | Potential for heightened stress levels and reduced mood |
| 8 hours | Optimal Alertness | Enhanced cognitive function, improved reaction time, and reduced risk of errors |
| 8 hours | Stable Physiological Processes | Maintenance of balanced hormone levels and cardiovascular health |
Long-Term Effects
Chronic sleep deprivation, the consistent lack of adequate sleep over an extended period, takes a significant toll on the body. The cumulative effects of not getting enough rest can manifest in a variety of ways, impacting overall health and well-being. These long-term consequences are often insidious, developing gradually and sometimes going unnoticed until they become severe.Sleep deprivation disrupts the delicate balance of bodily functions, leading to a cascade of negative impacts on physical health.
This disruption affects everything from immune response to metabolic regulation, potentially escalating the risk of developing chronic illnesses. Understanding these long-term consequences is crucial for promoting healthy sleep habits and preventative health measures.
Cumulative Physical Consequences
Chronic sleep deprivation leads to a build-up of negative effects on the body. This includes a weakened immune system, increased risk of chronic diseases, and significant hormonal imbalances. The body’s ability to repair and rejuvenate tissues is compromised, potentially leading to accelerated aging and a greater susceptibility to illness. The cumulative impact of this constant stress on the body can manifest in physical ailments and long-term health issues.
Impact on the Immune System
Adequate sleep is essential for a robust immune system. When sleep is consistently compromised, the body’s ability to fight off infections is diminished. This means individuals experiencing chronic sleep deprivation are more susceptible to colds, flu, and other illnesses. The body’s production of cytokines, essential proteins that regulate the immune response, is significantly affected by sleep deprivation, leading to a compromised immune defense.
This is particularly important for those facing stressful situations, injuries, or exposure to pathogens. A lack of sleep weakens the body’s natural defenses against illness.
Feeling sluggish and your body aching? Sleep deprivation wreaks havoc on your physical well-being, impacting everything from your mood to your metabolism. It can even affect how much protein you need in your diet to support muscle repair and growth. Understanding how much protein should i eat to lose weight here is crucial, but ultimately, prioritizing enough sleep is key to optimal physical health and recovery.
Without adequate rest, your body struggles to function efficiently, leading to a cascade of negative physical effects.
Link to Chronic Diseases
Research strongly suggests a correlation between chronic sleep deprivation and an increased risk of developing chronic diseases. The disruption of normal metabolic processes can contribute to conditions like type 2 diabetes and cardiovascular disease. For example, individuals who consistently sleep less than 7 hours per night may be at a higher risk of developing high blood pressure, a key factor in cardiovascular issues.
Studies have shown a direct link between insufficient sleep and elevated blood sugar levels, a significant risk factor for diabetes. These conditions can lead to serious health complications if left unaddressed.
Sleep Deprivation and Weight Management
Sleep deprivation can significantly affect weight management, either promoting weight gain or loss, depending on the individual and their lifestyle. The hormonal imbalances associated with insufficient sleep can disrupt the body’s natural appetite regulation, leading to increased cravings and overeating. This is because sleep deprivation affects the production of hormones like leptin and ghrelin, which control feelings of hunger and fullness.
The lack of sleep also reduces physical activity levels, contributing to weight gain. On the other hand, some individuals might experience a loss of appetite due to sleep deprivation, but this is usually temporary and not a healthy way to manage weight.
Comparison of Long-Term Effects
| Condition | Risk Factors (Sleep Deprivation) | Preventive Measures |
|---|---|---|
| Healthy Sleep Schedule | Regular sleep schedule, 7-9 hours of sleep per night, conducive sleep environment. | Establish a consistent sleep-wake cycle, create a relaxing bedtime routine, optimize sleep environment (dark, quiet, cool). |
| Chronic Sleep Deprivation | Irregular sleep schedule, less than 7 hours of sleep per night, stress, anxiety, poor sleep hygiene. | Identify and address underlying causes of sleep problems, implement good sleep hygiene practices, consult a healthcare professional for guidance. |
| Type 2 Diabetes | Increased risk of insulin resistance, elevated blood sugar levels. | Maintain a healthy diet, regular exercise, manage stress, consult a healthcare professional for guidance. |
| Cardiovascular Disease | Elevated blood pressure, increased risk of heart disease. | Maintain a healthy diet, regular exercise, manage stress, quit smoking, consult a healthcare professional for guidance. |
Specific Organ Systems
Sleep deprivation’s detrimental effects extend beyond the general malaise and cognitive impairments we’ve already discussed. It significantly impacts various organ systems, disrupting their delicate balance and leading to a cascade of potential health problems. Understanding these specific impacts is crucial for recognizing the long-term consequences of chronic sleep deficiency.
Cardiovascular System
Sleep deprivation disrupts the body’s natural rhythm, negatively impacting the cardiovascular system. This disruption manifests in elevated blood pressure and heart rate. Chronic sleep loss can contribute to hypertension and increase the risk of cardiovascular diseases. The body’s ability to regulate blood pressure is compromised, potentially leading to persistent high blood pressure.
Endocrine System
The endocrine system, responsible for hormone regulation, is profoundly affected by sleep deprivation. Hormonal imbalances can result, impacting various bodily functions. Cortisol, a stress hormone, is often elevated in sleep-deprived individuals, disrupting the delicate balance of hormones like growth hormone and insulin. This imbalance can affect metabolism, stress response, and even mood regulation.
Digestive System
Sleep deprivation can also significantly impact the digestive system, potentially leading to a range of issues. It can affect the production and function of digestive enzymes, resulting in reduced efficiency in breaking down food. This can lead to digestive problems, including indigestion, bloating, and potentially, more serious issues like ulcers. Sleep deprivation’s impact on stress hormones like cortisol also plays a role, as elevated cortisol can hinder the proper functioning of the digestive system.
Organ System Effects Table
| Organ System | Specific Effects | Severity of Impact |
|---|---|---|
| Cardiovascular | Elevated blood pressure, increased heart rate, impaired blood vessel function. | Chronic sleep loss can increase the risk of hypertension and cardiovascular diseases. |
| Endocrine | Elevated cortisol levels, disrupted regulation of growth hormone, insulin, and other hormones. | Chronic imbalances can affect metabolism, stress response, and overall health. |
| Digestive | Reduced digestive enzyme production, impaired digestion, increased risk of indigestion, bloating, and potentially ulcers. | Chronic sleep deprivation can contribute to persistent digestive issues and reduce the body’s ability to absorb nutrients efficiently. |
Impact on Physical Performance
Sleep deprivation significantly impairs physical performance, impacting athletes and everyday individuals alike. This detriment extends beyond just feeling tired; it affects fundamental aspects of physical ability, from strength and endurance to reaction time and motor skills. Understanding these effects is crucial for optimizing physical activity and preventing potential injuries.The human body requires sufficient sleep to effectively repair and rebuild tissues, synthesize hormones, and consolidate memories.
When sleep is compromised, these restorative processes are disrupted, leading to a cascade of negative consequences on physical performance. This includes a reduction in strength, endurance, and speed, along with a decrease in cognitive function, which directly influences motor skills and reaction time.
Effects on Strength Training
Sleep deprivation negatively impacts muscle protein synthesis, a crucial process for muscle growth and repair. When sleep is insufficient, the body’s ability to recover from the stress of strength training is hindered. This leads to a decrease in strength gains and an increased risk of muscle soreness and injury. The reduction in hormone levels like testosterone, crucial for muscle growth, is further exacerbated by insufficient sleep.
Feeling sluggish and irritable? Sleep deprivation wreaks havoc on your body, impacting everything from your immune system to your energy levels. While focusing on a healthy diet is crucial, like incorporating foods packed with nutrients, such as beef liver, which some consider a superfood, it’s important to prioritize adequate sleep for overall well-being. Is beef liver a superfood ?
Maybe, but a good night’s sleep will still be your best bet for optimal physical health.
Consequently, athletes and individuals engaged in strength training experience diminished performance and a slower rate of progress.
Effects on Endurance
Adequate sleep is essential for optimal endurance performance. Insufficient sleep reduces the body’s ability to utilize oxygen efficiently during prolonged physical activity. This can result in fatigue, reduced stamina, and a shortened time to exhaustion. Sleep deprivation can also negatively affect glycogen stores, the body’s primary energy source for endurance activities. Consequently, endurance athletes experience decreased performance and an increased risk of injury during training and competition.
Effects on Reaction Time
Sleep deprivation significantly impairs reaction time, which is critical for both athletes and everyday individuals. Reaction time is the time taken to respond to a stimulus, and insufficient sleep slows down this crucial process. This can lead to a higher risk of accidents and injuries, particularly in activities requiring quick responses, such as sports or driving. The reduced alertness and cognitive function associated with sleep deprivation directly contribute to slower reaction times.
Effects on Motor Skills and Coordination
Insufficient sleep directly impacts motor skills and coordination. This manifests in a reduced ability to perform precise movements and maintain balance. Sleep deprivation can impair the smooth execution of complex motor tasks, leading to mistakes and errors in sports or daily activities. Furthermore, the compromised cognitive function associated with sleep deprivation further diminishes the ability to execute and coordinate physical movements effectively.
Comparison of Physical Performance Metrics
| Physical Performance Metric | Adequate Sleep (7-9 hours) | Sleep-Deprived (Less than 5 hours) |
|---|---|---|
| Speed (e.g., sprint time) | Faster | Slower |
| Strength (e.g., bench press max) | Higher | Lower |
| Endurance (e.g., marathon time) | Longer | Shorter |
| Reaction Time (e.g., response to stimulus) | Faster | Slower |
| Motor Skill Precision | Higher | Lower |
Mental Health Implications: What Are The Physical Effects Of Sleep Deprivation
Sleep deprivation isn’t just a nuisance; it significantly impacts our mental well-being. The cumulative effect of insufficient sleep can manifest in a range of mental health issues, sometimes even masquerading as physical symptoms. Understanding this connection is crucial for recognizing the importance of adequate sleep in maintaining overall health and preventing the exacerbation of existing mental health conditions.The brain, during sleep, is engaged in vital restorative processes.
These processes are essential for emotional regulation, cognitive function, and maintaining a balanced mood. When sleep is consistently compromised, the delicate equilibrium of the mind is disturbed, potentially leading to increased susceptibility to mental health problems. Chronic sleep deprivation can impair the brain’s ability to regulate emotions, leading to heightened irritability, anxiety, and difficulty managing stress.
Manifestation of Mental Health Issues as Physical Symptoms
Sleep deprivation can manifest as a variety of physical symptoms that often mimic other medical conditions. For example, persistent headaches, muscle tension, and digestive issues can be related to a lack of sleep, not just a separate ailment. This can make it challenging for individuals to identify the root cause of their discomfort. Misdiagnosis can lead to further frustration and unnecessary medical interventions.
Potential Link Between Sleep Deprivation and Increased Risk of Mental Health Conditions
Studies suggest a strong correlation between sleep deprivation and an increased risk of developing mental health conditions like anxiety and depression. Insufficient sleep can exacerbate existing vulnerabilities and create new ones. This increased risk is not just theoretical; real-life examples show how sleep disruption can trigger or worsen symptoms in individuals predisposed to these conditions.
Impact of Sleep Deprivation on Mood Regulation and Emotional Responses
Sleep plays a critical role in regulating mood and emotional responses. When sleep is inadequate, the brain’s ability to process and manage emotions is compromised. This can lead to heightened irritability, emotional outbursts, difficulty controlling anger, and an overall diminished ability to cope with stress. Consequently, individuals experiencing chronic sleep deprivation might find themselves more prone to emotional reactivity and struggle with maintaining stable emotional well-being.
Examples of How Sleep Deprivation Can Worsen Existing Mental Health Conditions
Individuals with pre-existing mental health conditions, such as anxiety or depression, may experience a significant worsening of symptoms when sleep is consistently compromised. The reduced ability to cope with stress, the heightened emotional reactivity, and the impaired cognitive function associated with sleep deprivation can exacerbate the negative impact of these conditions. For instance, someone with anxiety may find that their anxiety symptoms become more intense and frequent when sleep is consistently disrupted.
Table: Mental Health Implications of Sleep Deprivation
| Mental Health Condition | Potential Physical Symptom | Severity |
|---|---|---|
| Anxiety | Muscle tension, headaches, gastrointestinal distress | Mild to moderate |
| Depression | Fatigue, loss of appetite, sleep disturbances | Mild to severe |
| Post-traumatic stress disorder (PTSD) | Flashbacks, nightmares, hypervigilance | Moderate to severe |
| Bipolar disorder | Increased irritability, mood swings, sleep disturbances | Moderate to severe |
Sleep deprivation is a significant risk factor in the development and exacerbation of various mental health conditions.
Dietary Considerations
Sleep deprivation significantly impacts our dietary choices and metabolic processes. Our bodies, when sleep-deprived, experience hormonal imbalances that can lead to increased cravings for certain foods, often high in sugar and unhealthy fats. This, coupled with changes in metabolism, can make it challenging to maintain a healthy diet and can lead to a vicious cycle of poor sleep, unhealthy eating, and further sleep disruption.
Effects on Hunger and Satiety Hormones
Sleep deprivation disrupts the delicate balance of hormones that regulate hunger and fullness. Ghrelin, the “hunger hormone,” increases when we are sleep-deprived, stimulating appetite and leading to increased food intake. Conversely, leptin, the “satiety hormone,” decreases, further contributing to the feeling of hunger. This hormonal imbalance can lead to overeating, especially of calorie-dense foods. For example, someone consistently experiencing sleep deprivation might find themselves reaching for sugary snacks or processed foods more often, simply because their bodies are signaling a need for more energy, even if their caloric intake is already high.
Impact on Metabolism and Energy Expenditure, What are the physical effects of sleep deprivation
Sleep deprivation negatively affects metabolic rate and energy expenditure. The body’s ability to burn calories efficiently diminishes, leading to a reduced metabolic rate. Consequently, individuals may struggle to lose weight or maintain a healthy weight, even with a balanced diet. This reduced metabolic rate can be further exacerbated by increased cortisol levels, which also contribute to fat storage and hinder fat burning.
Think of it like this: your body’s furnace is running less efficiently when you’re sleep-deprived, meaning it takes in more fuel (food) but burns less.
Correlation with Unhealthy Eating Habits
The interplay between sleep deprivation and unhealthy eating habits is complex. Sleep-deprived individuals often experience increased cravings for sugary and high-fat foods, leading to overeating. Conversely, some might experience decreased appetite, potentially leading to undernutrition, as their bodies struggle to maintain energy levels. This can result in an irregular and unhealthy eating pattern. For instance, a student pulling all-nighters for exams might experience both intense cravings and exhaustion, leading to unhealthy snacking habits and decreased energy expenditure.
Dietary Adjustments for Mitigation
To mitigate the negative effects of sleep deprivation on appetite and metabolism, dietary adjustments can be helpful. Prioritize whole, unprocessed foods. Increase intake of fruits, vegetables, and lean proteins. Limit processed foods, sugary drinks, and excessive amounts of unhealthy fats. Consider consulting a registered dietitian for personalized dietary recommendations tailored to individual needs and circumstances.
Table: Effects of Sleep Deprivation on Dietary Habits
| Aspect | Sleep-Deprived | Well-Rested |
|---|---|---|
| Appetite | Increased hunger, difficulty feeling full | Balanced hunger and satiety |
| Cravings | Increased cravings for sugary and high-fat foods | Balanced food cravings |
| Food Choices | More likely to choose processed and unhealthy foods | More likely to choose nutritious and whole foods |
Outcome Summary
In conclusion, the physical effects of sleep deprivation are multifaceted and profound. From the immediate impacts on alertness and reaction time to the long-term risks of chronic disease, prioritizing sleep is essential for physical well-being. By understanding how sleep loss affects different organ systems and impacts physical performance, we can take steps to improve our sleep hygiene and overall health.
This knowledge empowers us to make informed choices about our sleep habits, ultimately promoting a healthier and more productive life.