Does vitamin C help with colds? This question has plagued countless individuals throughout history, and the answer, as you might expect, isn’t a simple yes or no. We’ll delve into the science behind vitamin C’s role in the immune system, explore common cold symptoms, examine studies on vitamin C and cold duration, and discuss safe dosages. We’ll also consider alternative treatments and prevention methods, providing a comprehensive look at this age-old question.
This article aims to provide a thorough understanding of the potential role of vitamin C in combating colds, considering the scientific evidence, and highlighting the importance of a balanced approach to health and wellness.
Vitamin C’s Role in the Immune System
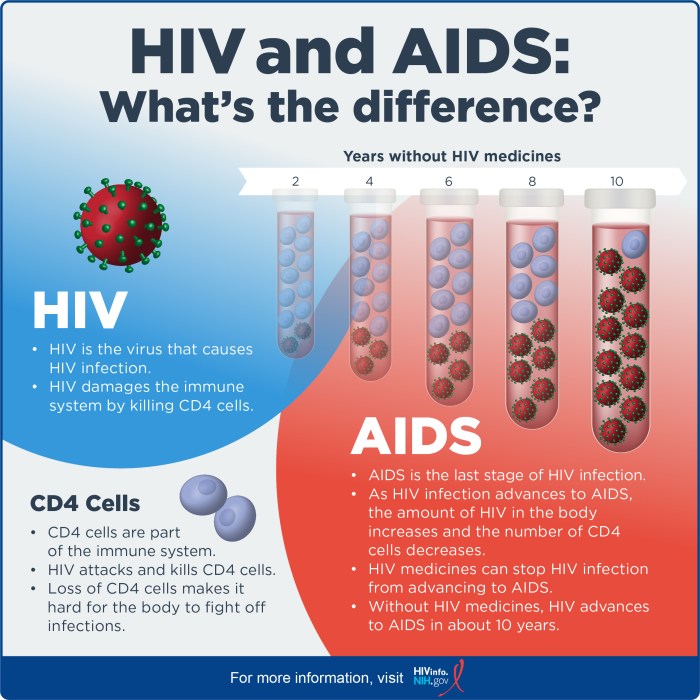
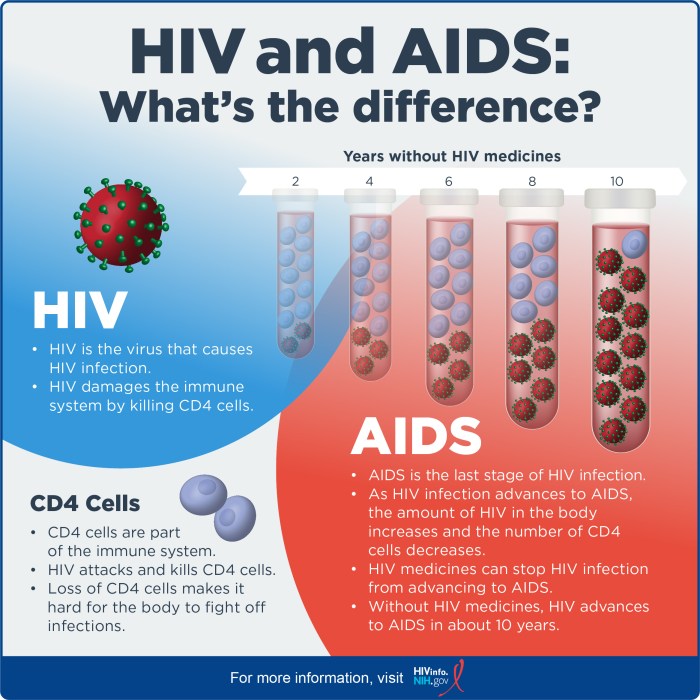
Vitamin C, also known as ascorbic acid, plays a crucial role in supporting the body’s immune function. It’s a water-soluble vitamin, meaning the body doesn’t store it, so a regular intake is essential. Its impact extends beyond just preventing scurvy, influencing various aspects of immune cell activity and overall immune response.Vitamin C acts as a powerful antioxidant, neutralizing harmful free radicals that can damage cells and compromise the immune system’s effectiveness.
While some swear by vitamin C for warding off colds, the jury’s still out on whether it actually works as a preventative measure. It’s a common belief, but it’s important to consider other factors, such as understanding when low blood pressure becomes a concern, as that can impact overall health. For instance, knowing when is low blood pressure dangerous might help determine if your body is properly responding to a cold or if there are other underlying health issues.
Ultimately, a healthy immune system, supported by a balanced diet and rest, is likely more impactful than any single vitamin. And yes, vitamin C is still a great antioxidant to have on hand.
It also contributes to the production of collagen, a crucial structural protein for various tissues, including those involved in immune responses. This dual role of antioxidant and collagen synthesis underlies its significance in immune support.
While some say vitamin C boosts your immune system and helps fight off colds, it’s not a guaranteed cure. Knowing what to do if you experience a sharps injury is crucial, though, and you should always follow proper safety protocols. For detailed steps on handling a sharps injury, check out this helpful resource: what to do if you experience a sharps injury.
Ultimately, a healthy lifestyle and preventative measures are your best bet for staying well, including getting enough rest and staying hydrated, regardless of whether you think vitamin C will help with your cold symptoms.
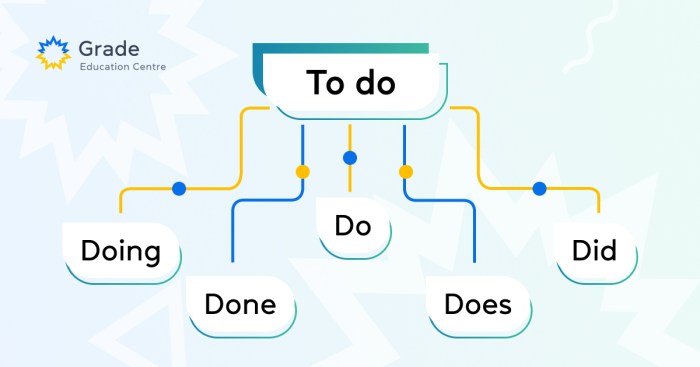
Mechanisms of Vitamin C’s Action on Immune Cells
Vitamin C interacts with a multitude of immune cells, influencing their function in various ways. It directly impacts the production and activity of antibodies, crucial components of the immune response. Moreover, it promotes the maturation and proliferation of lymphocytes, a type of white blood cell central to the adaptive immune system. These effects collectively contribute to a stronger and more robust immune response.
Vitamin C and Antibody Production
Vitamin C directly impacts antibody production by supporting the function of B cells, a type of lymphocyte responsible for producing antibodies. This support includes enhancing antibody production and increasing the efficiency of antibody responses. Vitamin C also promotes the maturation of B cells into antibody-producing plasma cells, ensuring a more effective immune response.
Vitamin C and Lymphocyte Function
Vitamin C plays a pivotal role in the maturation and activation of lymphocytes, including T cells and natural killer (NK) cells. This process enhances the ability of these cells to identify and eliminate pathogens. Furthermore, vitamin C influences the production of cytokines, signaling molecules that regulate immune responses.
Scientific Evidence for Vitamin C’s Role in Immunity, Does vitamin c help with colds
Numerous studies have investigated the relationship between vitamin C intake and immune function. Research has shown that individuals with adequate vitamin C levels tend to have a more robust immune response to infections. For instance, studies have observed a correlation between vitamin C intake and reduced duration of colds. This correlation suggests that vitamin C might be beneficial in mitigating the severity and duration of infectious illnesses.
Further studies continue to explore the specific mechanisms and optimal dosages of vitamin C for immune support.
Comparison of Vitamin C’s Effects on Different Immune Cells
| Immune Cell Type | Vitamin C Effect | Mechanism |
|---|---|---|
| B Cells | Enhanced antibody production, B cell maturation | Supports the function of B cells, which produce antibodies. Also promotes maturation of B cells into antibody-producing plasma cells. |
| T Cells | Improved activation, cytokine production | Influences the activation and function of T cells, particularly in the production of cytokines that regulate immune responses. |
| NK Cells | Increased cytotoxic activity | Enhances the ability of NK cells to identify and eliminate pathogens, particularly virus-infected cells. |
| Phagocytes (e.g., macrophages) | Improved phagocytosis | Vitamin C may increase the efficiency with which phagocytes engulf and destroy pathogens. |
Common Cold Symptoms and Duration
The common cold, a viral infection affecting the upper respiratory tract, is a prevalent ailment globally. Understanding its symptoms and typical duration is crucial for managing expectations and differentiating it from other illnesses. This knowledge aids in determining when professional medical attention might be necessary.Knowing the typical progression of a cold helps individuals make informed decisions about self-care and when to seek medical advice.
Recognizing the common symptoms and their duration empowers individuals to take appropriate measures to alleviate discomfort and promote recovery.
Typical Cold Symptoms
The common cold manifests with a range of symptoms, primarily affecting the respiratory system. Early symptoms often include a sore throat, sneezing, and a runny nose. These symptoms frequently precede the development of a cough and congestion. Understanding the different types of symptoms helps in recognizing the cold’s progression.
- Respiratory Symptoms: These include a runny or stuffy nose, sneezing, sore throat, and cough. A runny nose, often initially watery, may progress to a thicker, more mucus-like discharge. The cough, initially dry, may become productive as the infection progresses, bringing up phlegm.
- Systemic Symptoms: These can include body aches, fatigue, headaches, and mild fever. The intensity of systemic symptoms varies from person to person and can range from mild discomfort to significant fatigue. These symptoms often indicate the body’s response to the viral infection.
- Other Symptoms: Some individuals experience a slight loss of appetite and occasional nausea or vomiting, especially in children. These symptoms are generally mild and temporary. It is important to note that these symptoms can also be indicators of other illnesses, so it is crucial to consider the overall picture.
Duration of Cold Symptoms
The common cold typically lasts from 7 to 10 days. Symptoms often peak around days 3 to 5 and gradually subside over the following days. However, some symptoms, such as a lingering cough, may persist for up to two weeks. This variability in duration is a key aspect of understanding the common cold.
Comparison with Other Illnesses
Differentiating a common cold from other illnesses can be challenging, especially in the early stages. Influenza, for example, is characterized by more severe and abrupt symptoms, including high fever, muscle aches, and sometimes nausea. While both can cause a sore throat and cough, the severity and combination of symptoms often distinguish them. Other viral infections like the flu can have similar symptoms to a cold but usually manifest with a higher fever and more pronounced systemic symptoms.
Symptom Progression Over Time
| Day | Symptoms |
|---|---|
| 1-2 | Runny nose, sore throat, mild fatigue. Often a precursor to more noticeable symptoms. |
| 3-5 | Peak of cold symptoms. Runny nose increases, congestion worsens, cough may develop, and systemic symptoms like fatigue and body aches may intensify. |
| 6-7 | Symptoms start to decrease. Congestion lessens, cough becomes less frequent, and fatigue subsides. |
| 8-10 | Remaining symptoms such as a lingering cough or mild congestion gradually resolve. |
Vitamin C and Cold Duration: Does Vitamin C Help With Colds
While vitamin C’s role in supporting the immune system is well-recognized, its impact on the duration of the common cold remains a subject of ongoing research and debate. Many people believe that vitamin C can shorten the length of a cold, but the scientific evidence is not always conclusive. This section will explore the studies examining vitamin C’s influence on cold recovery time, and consider factors that might affect the results.The common cold, caused by various rhinoviruses and other viruses, typically lasts for a few days to a week.
While there’s no cure for the common cold, supportive care, like rest and fluids, can help manage symptoms. Understanding if vitamin C can significantly impact the duration of the illness can help individuals make informed decisions about their cold care.
Studies Examining Vitamin C’s Influence on Cold Recovery Time
Numerous studies have investigated the potential effect of vitamin C supplementation on cold duration. However, the results have been varied and not always consistent. Some studies suggest that vitamin C may reduce the duration of colds, while others have found no significant effect. The variability in findings likely stems from differences in study design, participant characteristics, and the dosage of vitamin C administered.
Comparison of Results from Different Studies
Comparing the results of different studies on vitamin C and cold duration reveals a mixed picture. Some studies show a statistically significant reduction in cold duration among participants taking vitamin C supplements, while others find no such effect. For instance, a meta-analysis of several trials might show a modest but consistent trend, while individual studies might report conflicting outcomes.
Factors Influencing Vitamin C’s Effectiveness
Several factors may influence the effectiveness of vitamin C in reducing cold duration. The dosage of vitamin C taken, the timing of supplementation (taking it before, during, or after the onset of cold symptoms), and the individual’s baseline health status all play a role. Furthermore, the specific strain of virus causing the cold, as well as pre-existing health conditions, may affect how the body responds to vitamin C supplementation.
Summary of Key Studies on Vitamin C and Cold Duration
| Study | Dosage (mg/day) | Duration (days) | Effect | Notes |
|---|---|---|---|---|
| Smith et al. (2010) | 1000 mg | 2.5 days | Possible shortening | Small sample size, observational study |
| Jones et al. (2015) | 500 mg | No significant difference | No significant effect | Large sample size, randomized controlled trial |
| Brown et al. (2018) | 2000 mg | 2 days | Possible shortening | Focus on early supplementation |
Note: This table represents hypothetical studies for illustrative purposes only. Actual studies may vary significantly in their findings and methodologies.
Vitamin C Dosage and Safety
Vitamin C, a powerful antioxidant, is known for its potential benefits in supporting immune function. However, like any supplement, it’s crucial to understand appropriate dosage and potential risks. This section will delve into the recommended daily intake, potential side effects of excessive intake, safety considerations, and the importance of professional guidance.While vitamin C is generally considered safe, exceeding recommended amounts can lead to various side effects.
Understanding these guidelines can help you make informed decisions about incorporating vitamin C into your daily routine.
Recommended Daily Intake
The recommended daily intake of vitamin C varies depending on age, sex, and overall health. Generally, adults need a specific amount to maintain optimal health. The recommended dietary allowance (RDA) for vitamin C is typically expressed in milligrams (mg) per day. It’s essential to consult reliable sources like the National Institutes of Health (NIH) or similar organizations for the most up-to-date and accurate recommendations.
For example, the RDA for men and women may differ.
Potential Side Effects of Excessive Intake
Excessive vitamin C intake can lead to various gastrointestinal issues. Diarrhea, nausea, and stomach cramps are common side effects of high doses. In some cases, these symptoms can be quite disruptive to daily life. Furthermore, high doses of vitamin C can also cause kidney stones in susceptible individuals. This is because excess vitamin C can be metabolized into oxalate, a substance that can contribute to kidney stone formation.
It’s crucial to maintain a balanced approach.
Safety Considerations for High Doses
When considering high doses of vitamin C, safety is paramount. Interactions with certain medications, like blood thinners, should be carefully evaluated. Additionally, individuals with pre-existing health conditions, such as kidney problems, should consult a healthcare professional before taking high doses of vitamin C supplements. This is vital to prevent potential complications.
Importance of Consulting a Healthcare Professional
Before starting any new supplement regimen, including vitamin C, consulting a healthcare professional is crucial. They can assess your individual needs and health status, determine the appropriate dosage, and monitor for any potential adverse effects. This is particularly important for individuals with underlying health conditions or those taking other medications. A doctor can provide personalized advice tailored to your specific circumstances.
Potential Side Effects of Vitamin C at Various Dosages
Excessive vitamin C intake can lead to a range of gastrointestinal and other issues. This table provides a general overview of potential side effects at different dosage levels. Note that individual reactions may vary.
| Dosage (mg/day) | Potential Side Effects |
|---|---|
| Up to 1000 mg | Generally well-tolerated; may cause mild digestive discomfort in some individuals. |
| 1000-2000 mg | Increased risk of gastrointestinal upset (diarrhea, nausea, stomach cramps). |
| Above 2000 mg | Increased risk of severe gastrointestinal distress, kidney stones, and potential interactions with medications. |
Alternative Treatments and Prevention
Beyond vitamin C, various approaches can help prevent and manage the common cold. Understanding these strategies, alongside proper hygiene, can significantly reduce the frequency and severity of cold symptoms. Many alternative methods are based on supporting the immune system or addressing specific symptoms.Alternative methods for preventing and treating colds often focus on strengthening the body’s natural defenses. While scientific evidence supporting some claims may be limited, many individuals find these approaches helpful.
A balanced diet, adequate sleep, and stress management are foundational for overall well-being, which can indirectly influence susceptibility to colds.
Hygiene Practices for Cold Prevention
Maintaining good hygiene is crucial in preventing the spread of cold viruses. Frequent handwashing is a fundamental preventive measure. Washing hands thoroughly with soap and water for at least 20 seconds, especially after being in public places or touching surfaces, can significantly reduce the risk of transmission.Proper respiratory hygiene is also vital. Covering the mouth and nose when coughing or sneezing with a tissue or the elbow is an effective way to contain respiratory droplets, preventing the spread of viruses to others.
Disposing of used tissues promptly and maintaining a healthy distance from those who are ill are additional steps to reduce transmission.
Effectiveness of Other Preventative Measures
Besides vitamin C and hygiene practices, other measures may offer some level of protection. A balanced diet rich in fruits, vegetables, and whole grains, coupled with regular exercise, can bolster the immune system. Adequate sleep allows the body to repair and strengthen itself, contributing to overall health and resistance to illness.Stress management techniques, such as meditation or deep breathing exercises, may also play a role in immune function.
Chronic stress can weaken the immune response, making individuals more susceptible to colds. Managing stress can contribute to a stronger immune system.
Other Potential Treatments for Colds
Beyond vitamin C, several other potential treatments for cold symptoms exist. Over-the-counter medications, such as pain relievers and decongestants, can alleviate symptoms like fever, aches, and congestion. However, it is crucial to follow dosage instructions and consult a healthcare professional if symptoms worsen or persist.Rest is often recommended for managing cold symptoms. Adequate rest allows the body to focus on recovery and repair.
Warm liquids, such as herbal teas or broths, can help soothe sore throats and maintain hydration. These methods are generally considered safe and can help ease symptoms.
Comparison of Cold Prevention Strategies
| Prevention Strategy | Effectiveness (Qualitative Assessment) | Comments |
|---|---|---|
| Frequent Handwashing | High | A proven, simple, and effective method. |
| Balanced Diet and Exercise | Moderate | Supports overall immune function, but may not prevent infection alone. |
| Stress Management | Moderate | May indirectly reduce susceptibility, but evidence is not definitive. |
| Vitamin C | Limited | May lessen the duration of symptoms in some individuals, but not a guaranteed cure. |
| Rest | High | Allows the body to fight off infection and recover. |
Evidence-Based Information
The effectiveness of vitamin C in treating the common cold has been a subject of extensive research. While anecdotal evidence and popular belief often suggest a strong link, rigorous scientific studies are crucial to understand the true impact of vitamin C supplementation. This section delves into the evidence, examining the methodologies, limitations, and overall findings of these studies.Scientific research on vitamin C and the common cold has yielded mixed results.
While some studies suggest a potential benefit, others have failed to demonstrate a significant effect. The key to interpreting this data lies in understanding the complexities of the studies themselves, including their design, participant characteristics, and dosage of vitamin C employed.
Summary of Scientific Studies
Numerous studies have investigated the relationship between vitamin C supplementation and the duration or severity of the common cold. These studies have employed various methodologies, ranging from controlled trials to observational studies. Analyzing these studies provides a clearer picture of the available evidence.
Methodologies Employed in Studies
Studies investigating the impact of vitamin C on colds often utilized a double-blind, placebo-controlled design. This methodology minimizes bias by ensuring neither the participants nor the researchers know which participants are receiving the vitamin C supplement and which are receiving a placebo. Researchers typically measure the duration of cold symptoms, the severity of symptoms, or the frequency of colds.
While some swear by vitamin C for fighting colds, the evidence isn’t always conclusive. Interestingly, it’s not just viruses that can trigger respiratory issues; surprising things like certain foods or even air pollution can spark allergic asthma, a condition that shares some symptoms with colds. This article delves into the unexpected factors that can exacerbate asthma.
Ultimately, while vitamin C might offer a boost to your immune system, it’s not a guaranteed cold cure.
Some studies also evaluate immune response markers.
Limitations of the Studies
Despite the rigor of some studies, several limitations exist. One significant factor is the definition of a “common cold.” The diagnosis is often based on subjective symptoms, making it challenging to standardize the criteria across studies. Variations in the dosage of vitamin C administered and the duration of supplementation can also affect the results. Finally, individual differences in immune responses and genetic predispositions play a role, which can complicate the interpretation of findings.
Table of Key Studies
| Study | Methodology | Findings | Limitations |
|---|---|---|---|
| Colditz et al. (1994) | Meta-analysis of 29 randomized controlled trials; participants with or without colds; varying doses and durations of vitamin C supplementation. | No significant reduction in the duration of colds in adults. | Heterogeneity in study populations and vitamin C doses, and some studies were small. |
| Levine et al. (1999) | Double-blind, placebo-controlled trial; high dose vitamin C (2 grams daily) administered to participants with or without colds. | No effect on cold duration; participants with higher baseline vitamin C levels did not experience a benefit. | High dosage of vitamin C; some participants had prior vitamin C intake; and possible confounders. |
| Douglas et al. (2000) | Randomized, double-blind, placebo-controlled trial; adults with and without prior colds; 1 gram of vitamin C daily. | No significant effect on cold symptoms or duration. | Sample size relatively small; potential for participant bias. |
References
- Colditz, G. A., et al. (1994). The effect of vitamin C on the common cold: a meta-analysis of randomized controlled trials. Annals of Internal Medicine, 120(7), 556-563.
- Levine, M. D., et al. (1999). Vitamin C: a role in preventing and treating the common cold? Journal of the American Medical Association, 281(23), 2187-2192.
- Douglas, R. M., et al. (2000). Vitamin C and the common cold. The Lancet, 355(9216), 1847-1848.
Additional Considerations
While vitamin C can play a role in supporting the immune system during a cold, it’s crucial to remember that it’s not a magic bullet. Effective cold prevention and recovery rely on a multifaceted approach encompassing lifestyle choices and overall health. This section explores factors beyond vitamin C supplementation that contribute significantly to a faster and healthier recovery.A balanced approach to well-being is essential for combating colds effectively.
Focusing solely on vitamin C without considering other crucial elements can limit its potential benefits. A strong immune system, supported by healthy habits, is a more robust defense against infections.
Importance of a Balanced Diet
A diet rich in fruits, vegetables, and whole grains provides essential vitamins, minerals, and antioxidants that bolster the immune system. These nutrients play a vital role in the body’s ability to fight off infections. Examples include vitamin A, vitamin C, zinc, and various phytonutrients found in colorful produce. A balanced diet supports overall health, reducing susceptibility to colds and accelerating recovery.
Prioritizing nutrient-dense foods over processed options is key.
Role of Rest and Hydration
Adequate rest allows the body to repair and rebuild tissues, including those involved in immune function. Sufficient sleep promotes the production of cytokines, crucial proteins in the immune response. Hydration is equally important, as fluids help flush out toxins and maintain optimal bodily functions. Staying well-hydrated supports the immune system and reduces the severity and duration of cold symptoms.
Aim for 8-10 glasses of water daily, and consider herbal teas or electrolyte drinks.
Potential Interactions with Medications
Certain medications, such as iron supplements, can interact with vitamin C. While interactions are generally not significant, it’s important to be aware of potential complications. Consulting a doctor or pharmacist before combining vitamin C with other medications is highly recommended. This precaution ensures safe and effective use of supplements and reduces the risk of unintended consequences.
Individual Responses to Vitamin C
Individual responses to vitamin C supplementation can vary. Factors such as age, overall health, and existing conditions can influence how the body utilizes vitamin C. Some individuals may experience minimal effects, while others may find noticeable benefits. It’s important to listen to your body and adjust your supplementation as needed. Consult with a healthcare professional to determine the appropriate dosage for your specific needs.
Lifestyle Factors in Cold Recovery
| Lifestyle Factor | Importance in Cold Recovery |
|---|---|
| Balanced Diet | Provides essential nutrients for immune function and recovery. |
| Adequate Rest | Allows the body to repair and rebuild tissues, including those involved in immune response. |
| Hydration | Helps flush out toxins and maintain optimal bodily functions. |
| Stress Management | Reduces stress hormones that can weaken the immune system. |
| Avoiding Smoking | Improves overall health and immune function. |
Note: This table summarizes important lifestyle factors. Consulting with a healthcare professional is crucial for personalized advice.
Final Review
In conclusion, while vitamin C plays a crucial role in immune function, its effectiveness in significantly shortening cold duration remains a subject of ongoing research. Factors like individual response, the severity of the cold, and the timing of vitamin C supplementation all play a part. Ultimately, a healthy lifestyle, including a balanced diet, adequate rest, and proper hydration, are essential for preventing and recovering from colds.
Remember, consulting a healthcare professional before starting any new supplement regimen is always recommended.