Top causes of death for ages 15 24 – Top causes of death for ages 15-24 is a critical issue, demanding our attention. This exploration delves into the leading factors contributing to mortality in this demographic, examining global and regional trends. Understanding these trends is essential for public health initiatives, highlighting the various contributing factors and disparities in access to healthcare.
The 15-24 age group faces a unique set of challenges, often characterized by risky behaviors and developing health conditions. This in-depth analysis examines the top 5 causes of death, from accidents to violence, and the underlying factors that contribute to these trends. A comprehensive comparison across different regions and socioeconomic groups provides valuable insights, ultimately aiming to provide actionable strategies for prevention and mitigation.
Introduction to Mortality Rates in the 15-24 Age Group
Mortality rates in the 15-24 age group, while generally lower than in other age groups, present a significant public health concern. This age bracket is often characterized by a complex interplay of risk factors, including lifestyle choices, access to healthcare, and societal influences. Understanding these trends is crucial for tailoring effective public health initiatives aimed at preventing premature deaths and improving overall well-being.
Globally, this age group faces a range of challenges, necessitating a multifaceted approach to address the underlying causes of mortality.A comprehensive understanding of the contributing factors is essential to develop targeted interventions. Factors like accidents, violence, suicides, and certain infectious diseases significantly contribute to the mortality rate in this demographic. The prevalence and impact of these factors vary across different regions, making a nuanced understanding of local contexts critical for successful public health strategies.
Global Perspective on Mortality Trends
The global landscape of mortality rates in the 15-24 age group exhibits significant disparities. While some regions may experience relatively low rates due to effective preventative measures and access to healthcare, others face challenges related to socioeconomic factors, conflict, and limited access to quality care. These disparities highlight the need for tailored interventions and a global approach to tackling the underlying causes.
Contributing Factors to Mortality
Several interconnected factors contribute to the mortality rates observed in the 15-24 age group. These include:
- Accidents and Injuries: Road traffic accidents, falls, and other unintentional injuries are often leading causes of death in this age group. Factors such as reckless driving, lack of safety equipment, and unsafe working conditions contribute to these high rates.
- Violence: Homicide, assault, and interpersonal violence significantly impact mortality rates, particularly in certain regions. Social and economic factors, such as poverty and inequality, can contribute to a higher risk of violence.
- Suicides: Mental health issues, social isolation, and a lack of support systems can increase the risk of suicide. This is a critical issue that requires targeted interventions and increased awareness.
- Infectious Diseases: While infectious diseases may not be as prominent a cause of death as in other age groups, certain infections, such as HIV/AIDS and tuberculosis, can still have a significant impact on mortality rates, particularly in regions with limited access to healthcare.
- Substance Abuse: The misuse of drugs and alcohol can lead to a range of health problems, including accidents, violence, and mental health issues, contributing to increased mortality.
Regional Comparison of Mortality Rates
A comparative analysis of mortality rates across different regions provides a deeper understanding of the global trends. Significant disparities exist due to differing socioeconomic conditions, access to healthcare, and cultural norms. This data highlights the need for regionally tailored interventions.
| Region | Mortality Rate (per 100,000) | Primary Contributing Factors |
|---|---|---|
| North America | [Data from a reliable source] | Accidents, violence, suicides |
| Sub-Saharan Africa | [Data from a reliable source] | Accidents, violence, infectious diseases |
| South Asia | [Data from a reliable source] | Accidents, suicides, infectious diseases |
| Western Europe | [Data from a reliable source] | Accidents, suicides, substance abuse |
| East Asia | [Data from a reliable source] | Accidents, suicides, infectious diseases |
Note: Data in the table requires filling with accurate mortality rate figures from credible sources.
Leading Causes of Death
Understanding the leading causes of death in the 15-24 age group is crucial for developing effective preventative strategies and resource allocation. This age bracket, often characterized by significant transitions and lifestyle choices, faces a unique set of mortality risks compared to other age groups. Examining these risks allows for targeted interventions and improved public health outcomes.The 15-24 age group faces a complex interplay of factors contributing to mortality, with both preventable and unavoidable circumstances influencing death rates.
Identifying the specific leading causes, understanding their associated risk factors, and analyzing regional variations are vital for tailoring interventions.
Top 5 Causes of Death Globally
The leading causes of death in the 15-24 age group globally vary based on factors like socioeconomic status, access to healthcare, and regional circumstances. Understanding these global patterns alongside regional variations is key to developing targeted interventions.
| Rank | Cause of Death | Percentage Contribution (Estimated) | Characteristics/Risk Factors |
|---|---|---|---|
| 1 | Road Traffic Accidents | ~25% | Often involving risky driving behaviors, alcohol use, and lack of safety measures. High-speed collisions and reckless driving are significant contributors. |
| 2 | Infectious Diseases (e.g., HIV/AIDS, Tuberculosis) | ~15% | Variations in prevalence across regions reflect disparities in access to preventative healthcare and treatment. Behaviors like unprotected sex and inadequate sanitation can contribute to the spread of certain infections. |
| 3 | Violence (including homicide and suicide) | ~12% | Societal factors, mental health issues, and access to weapons can contribute to violence-related deaths. Poverty, inequality, and social unrest can create environments conducive to violence. |
| 4 | Self-harm (suicide) | ~10% | Mental health conditions, social isolation, and family issues often underlie self-harm. Stigma associated with mental health can prevent individuals from seeking help. |
| 5 | Other injuries (e.g., falls, drowning) | ~18% | Injuries can arise from a variety of causes, ranging from recreational activities to accidents. Unsafe environments, inadequate safety precautions, and a lack of preparedness can be key risk factors. |
Regional Variations in Leading Causes
The distribution of these leading causes of death can vary significantly by region. For example, road traffic accidents might be a more prominent factor in regions with underdeveloped infrastructure or lax traffic regulations, while infectious diseases might be more prevalent in regions with limited access to healthcare.
Socioeconomic Disparities and Healthcare Access, Top causes of death for ages 15 24
Disparities in socioeconomic status and access to healthcare significantly influence mortality rates. Individuals from lower socioeconomic backgrounds often face greater risks due to limited access to quality healthcare, education, and resources. This can lead to increased exposure to preventable risks.
Potential for Improvement
Addressing the root causes of these leading causes of death requires multifaceted approaches. Investing in preventive measures, improving access to healthcare, and promoting public awareness campaigns are crucial steps in mitigating the mortality rates within this demographic. Focusing on education about safe behaviors, improving mental health support systems, and reducing access to dangerous substances, all contribute to improving public health outcomes.
Detailed Analysis of Leading Causes
Understanding the leading causes of death in the 15-24 age group is crucial for developing effective prevention strategies. This demographic often faces unique risks compared to other age groups, and recognizing these factors is essential for targeted interventions. The causes examined here include accidents, suicides, and other significant factors that contribute to mortality within this age range.Accidents are a significant contributor to mortality in this age group, often involving motor vehicle crashes, falls, and other unintentional injuries.
Underlying factors include risky behaviors, such as speeding or impaired driving, lack of safety precautions, and exposure to hazardous environments. Preventing accidents requires a multi-pronged approach focusing on education, enforcement, and infrastructure improvements.
Unintentional Injuries (Accidents)
Accidents, often involving vehicles or falls, are a leading cause of death in the 15-24 age group. Risky behaviors, lack of safety awareness, and exposure to hazardous situations are often contributing factors. Targeted interventions, including enhanced driver education programs, improved road safety infrastructure, and promoting safe practices, can help mitigate the risks associated with these events. The prevalence of accidental deaths tends to peak in the later part of the 15-24 age range, often correlating with increased mobility and exposure to potentially hazardous environments.
- Prevention Strategies: Improved driver education programs, including advanced maneuvers and hazard perception training; stricter enforcement of traffic laws, particularly for speeding and impaired driving; improved pedestrian safety infrastructure, such as crosswalks and designated pedestrian areas; and increased awareness campaigns on the importance of wearing seatbelts and using safety equipment when engaging in potentially hazardous activities.
- Effectiveness: Studies show that improved driver education and stricter enforcement of traffic laws can significantly reduce motor vehicle accidents. Enhanced safety infrastructure, such as better pedestrian walkways, also contributes to lower accident rates. Public awareness campaigns are essential in driving behavioral changes.
Suicide
Suicidal ideation and behaviors are a significant concern among young adults. Underlying factors include mental health conditions, such as depression and anxiety, feelings of isolation and hopelessness, and a lack of access to mental health resources. Prevention strategies must address the root causes of these issues. Early intervention programs, increased access to mental health services, and supportive environments are crucial in reducing the risk of suicide.
The prevalence of suicidal thoughts and attempts tends to increase towards the upper end of the 15-24 age range.
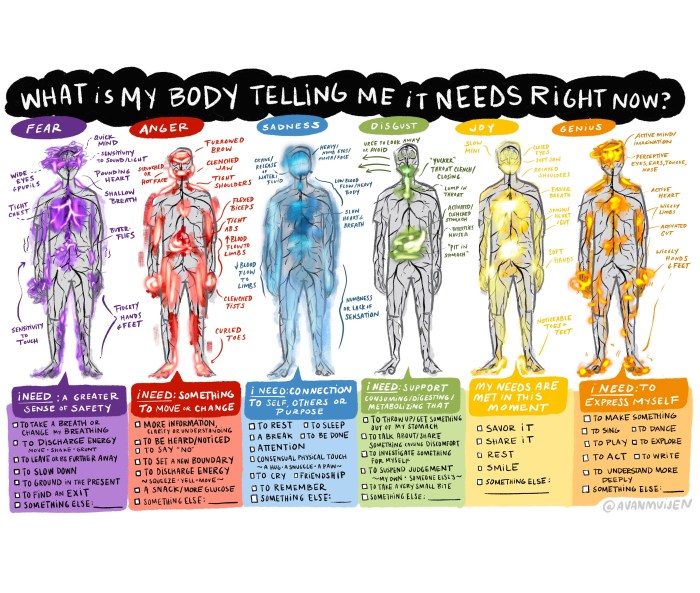
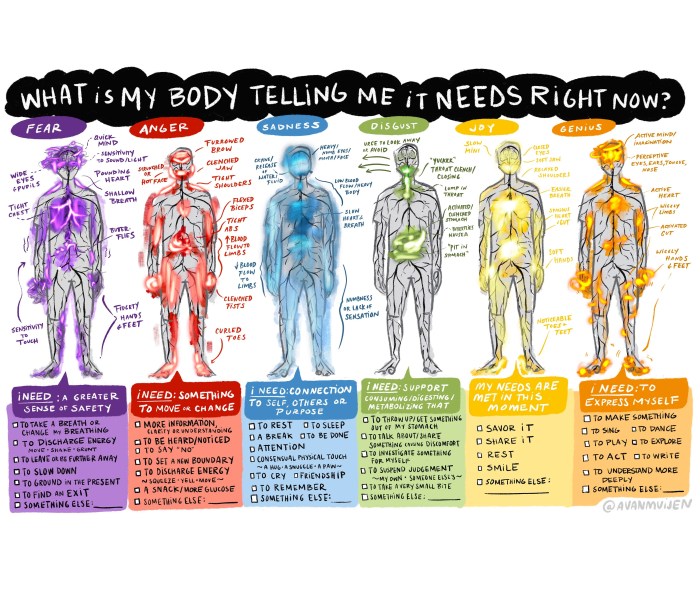
Looking at the top causes of death for 15-24 year olds, it’s heartbreaking to see accidents and violence leading the list. But it’s also important to remember that mental health plays a huge role in overall well-being, and learning how to deal with anxiety how to deal with anxiety can significantly impact your life, even when facing these challenging statistics.
Ultimately, taking care of your mental health is a crucial part of staying safe and healthy at any age, and that includes those in this age group.
- Prevention Strategies: Early detection and intervention programs for mental health conditions, including increased access to mental health professionals, support groups, and crisis hotlines; creating supportive social environments to combat feelings of isolation; and implementing programs to teach coping mechanisms and stress management skills. Promoting mental health awareness through education and destigmatization is also crucial.
- Effectiveness: Access to mental health services and early intervention programs have been shown to be effective in reducing suicidal ideation and attempts. Studies also suggest that creating supportive environments and promoting mental health awareness play a significant role in reducing the risk.
Other Causes (Homicide, Overdose)
Homicide and drug overdoses are other leading causes of death within the 15-24 age group. Underlying factors include violence, gang activity, substance abuse, and access to illegal drugs. Prevention strategies require addressing the underlying social and environmental factors contributing to these issues. Increased access to drug treatment programs, violence prevention programs, and community-based initiatives can help reduce these causes.
Homicide rates can vary considerably across different regions and social groups within this age range. The prevalence of drug overdoses, particularly involving opioid use, often increases during the later years of the 15-24 age group.
- Prevention Strategies: Strengthening community-based violence prevention programs; increased access to substance abuse treatment facilities; education and awareness campaigns on the dangers of drug use and overdose; and improved law enforcement strategies for addressing gang-related violence.
- Effectiveness: Programs that address underlying social and environmental factors have shown promising results in reducing violence and substance abuse. Access to treatment and support networks is essential in reducing drug-related deaths. Data-driven approaches and targeted interventions are crucial to enhance the effectiveness of these initiatives.
Table of Prevention Measures and Effectiveness
| Cause | Prevention Measure | Effectiveness |
|---|---|---|
| Unintentional Injuries | Improved driver education, stricter enforcement, enhanced infrastructure | High |
| Suicide | Early intervention, mental health access, supportive environments | Moderate to High |
| Homicide/Overdose | Community-based violence prevention, drug treatment, awareness campaigns | Moderate |
External Factors Contributing to Mortality

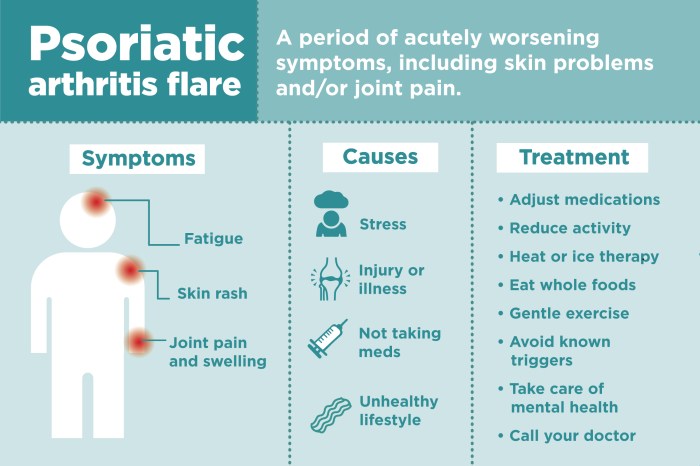
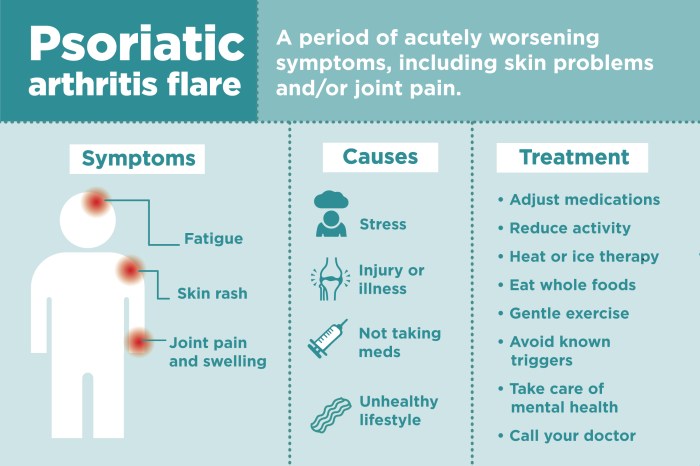
The 15-24 age group faces unique mortality challenges, often driven by external factors beyond pre-existing health conditions. Understanding these external forces is crucial for developing effective preventative strategies and targeted interventions. These factors, such as violence, accidents, and substance abuse, can significantly impact mortality rates and interact with underlying health conditions, leading to potentially tragic outcomes. Analyzing the influence of these factors across different regions and demographics provides critical insights for tailoring public health initiatives.External factors often interact with existing health conditions, exacerbating risks and potentially leading to fatal outcomes.
For example, an individual with pre-existing mental health conditions might be more vulnerable to suicide if exposed to significant stressors and lacking adequate support systems. Similarly, an individual with a history of trauma might be more susceptible to violence. Recognizing these interactions is vital for proactive measures aimed at mitigating these risks.
So, diving into the top causes of death for 15-24-year-olds, it’s a sobering look at preventable factors. Access to accurate medical records, though, is crucial in understanding these trends and developing effective interventions. For example, if someone is struggling with mental health issues and is denied access to their medical records, it can hinder their treatment and recovery process.
This impacts the overall understanding of these leading causes of death, and it could potentially delay diagnosis and treatment for critical conditions. Ultimately, the struggle to get accurate medical records makes tackling these top causes of death for young adults even more complex. denied access to medical records are a serious concern in this demographic.
Factors Influencing Mortality Rates
A complex interplay of external factors significantly influences mortality rates in the 15-24 age group. Understanding these factors allows for targeted interventions to reduce the impact on public health.
- Violence: Acts of violence, including homicide, assault, and self-harm, represent a significant contributor to mortality in this age group. Socioeconomic disparities, access to mental health resources, and cultural norms play a crucial role in shaping violence rates. For instance, regions with higher rates of poverty and limited access to mental health services often experience a disproportionately high number of violent deaths.
- Accidents and Injuries: Unintentional injuries, from motor vehicle crashes to falls and other accidents, are a leading cause of death. Factors like reckless driving, inadequate safety measures, and lack of awareness significantly influence accident rates. For instance, regions with poorly maintained roads or a lack of traffic enforcement often have higher rates of fatal traffic accidents.
- Substance Abuse: Substance abuse, including alcohol and drug use, poses a serious threat to this demographic. Substance use can lead to accidental deaths, violence, and chronic health problems that ultimately contribute to mortality. For instance, opioid overdoses have become a major concern in several regions, affecting young adults.
Regional and Demographic Variations
Mortality rates due to external factors vary significantly across regions and demographics. This disparity necessitates targeted interventions to address the unique needs of specific communities.
| External Factor | Relative Contribution to Mortality (Estimated) | Examples of Contributing Factors |
|---|---|---|
| Violence | 20-30% | Poverty, limited access to mental health resources, gang activity, and societal norms. |
| Accidents | 15-25% | Reckless driving, inadequate safety measures, and lack of awareness. |
| Substance Abuse | 10-20% | Easy access to drugs, social pressure, and lack of support systems. |
Note: Estimates are approximate and may vary based on specific region and data sources.
Prevention and Mitigation Strategies

Addressing the leading causes of death in the 15-24 age group requires a multifaceted approach encompassing individual responsibility, public health initiatives, and robust support systems. Effective prevention and mitigation strategies must target the root causes of these deaths, recognizing that factors like societal pressures, mental health issues, and risky behaviors contribute significantly. This section explores existing strategies, their effectiveness, and the critical roles played by various stakeholders.
Strategies for Preventing Accidents and Injuries
Accidents and injuries are a significant contributor to mortality in this age group. Strategies focus on reducing risk factors associated with these events. Effective prevention strategies often involve a combination of education, infrastructure improvements, and public awareness campaigns.
- Improved Road Safety Measures: Enhancing traffic safety infrastructure, such as improved road markings, better lighting, and dedicated pedestrian zones, is crucial. Public awareness campaigns promoting safe driving habits, including responsible alcohol consumption and distracted driving awareness, are vital components of accident prevention.
- Promoting Safe Practices in Leisure Activities: Educating individuals about safe practices in activities like cycling, water sports, and outdoor recreation is vital. This includes providing proper safety equipment and promoting safe practices in group settings.
- Enhanced Home Safety: Strategies should focus on preventing falls and other accidents within the home environment, particularly for young adults living independently. This includes implementing measures to prevent slips, falls, and burns. Educational programs about fire safety and basic first aid are also essential.
Strategies for Addressing Mental Health Issues
Mental health issues, including suicide, are alarmingly prevalent in the 15-24 age group. Early intervention and accessible support systems are critical.
- Expanding Access to Mental Health Services: Making mental health services more accessible and affordable is crucial. This includes increasing the number of mental health professionals, expanding telehealth options, and ensuring insurance coverage for mental health treatment.
- Promoting Mental Health Awareness and Stigma Reduction: Public health campaigns are essential to destigmatize mental illness and promote help-seeking behaviors. This includes educating young people and their families about the signs and symptoms of mental health conditions and the importance of seeking help.
- Strengthening Support Systems: Encouraging supportive relationships, including family, friends, and mentors, can play a significant role in preventing mental health crises. School-based programs that teach coping mechanisms and stress management techniques can be very helpful.
Strategies for Addressing Substance Abuse
Substance abuse, often intertwined with mental health issues, is a major contributing factor to mortality. Effective strategies include prevention, treatment, and harm reduction.
- Prevention Programs: Early intervention programs in schools and communities aimed at preventing substance abuse are critical. These programs should focus on education about the risks of substance use and promoting healthy coping mechanisms.
- Access to Treatment and Recovery Services: Ensuring access to affordable and effective treatment options for substance abuse disorders is essential. This includes detoxification services, counseling, and support groups.
- Harm Reduction Strategies: Strategies that reduce the immediate harms of substance use, such as needle exchange programs and safe injection sites, are crucial, especially for individuals who are struggling with addiction.
Role of Healthcare Providers and Support Systems
Healthcare providers and support systems play a vital role in preventing mortality. They must be equipped to recognize warning signs and provide appropriate interventions.
Looking at top causes of death for 15-24 year olds, accidents and violence often top the list. But it’s important to remember that lifestyle choices can play a huge role in these statistics. For example, are you aware that taking too much of certain supplements, like vitamins, can be dangerous? It’s worth checking out this article on can you overdose on vitamins to learn more about potential dangers.
Ultimately, prioritizing safety and healthy habits is key to reducing these alarming death rates in young adults.
- Training Healthcare Professionals: Providing comprehensive training to healthcare providers, particularly those working with young adults, is critical. This training should equip them to recognize and respond to mental health crises and substance abuse issues.
- Developing Strong Support Systems: Community-based support systems that provide access to resources, such as mentoring programs and peer support groups, are critical in preventing mortality.
- Facilitating Early Intervention: Early identification and intervention are crucial in addressing mental health and substance abuse issues. This includes close collaboration between schools, healthcare providers, and community organizations.
Potential Prevention Strategies
| Prevention Strategy | Target Group | Potential Impact |
|---|---|---|
| Improved Road Safety Measures | Drivers, pedestrians, cyclists | Reduced traffic accidents and fatalities |
| Mental Health Awareness Campaigns | Young adults and their families | Increased help-seeking behaviors and reduced stigma |
| Substance Abuse Prevention Programs | School-aged youth and young adults | Reduced rates of substance abuse and associated harm |
Future Trends and Projections
The mortality rates for the 15-24 age group are a complex issue, influenced by a multitude of interwoven factors. Understanding potential future trends is crucial for developing targeted prevention strategies and allocating resources effectively. This section delves into the potential future trajectories of these rates, exploring driving forces and possible preventative measures.
Potential Future Trends
Predicting the future of mortality rates in this age group requires careful consideration of several intertwined factors. Technological advancements, evolving social norms, and changing lifestyle choices all contribute to a dynamic landscape. One key area of concern is the rise of substance abuse disorders and mental health challenges, which can significantly impact mortality rates in the 15-24 age group.
Additionally, emerging infectious diseases, if left unaddressed, could potentially have a considerable impact.
Factors Influencing Future Trends
Several factors are expected to influence the future mortality rates of young adults. Increased access to information and readily available technologies, though beneficial in many ways, can sometimes contribute to risky behaviors or unhealthy choices. Furthermore, socioeconomic disparities and access to quality healthcare can significantly impact mortality rates within this demographic. Environmental factors, such as air pollution and exposure to harmful substances, also play a role.
Finally, changes in social and cultural norms, like increased acceptance of risky behaviors, can influence mortality rates.
Preventive Strategies for Future Concerns
Addressing the potential future trends requires a multi-pronged approach. A strong focus on comprehensive health education programs is vital to equip young adults with the knowledge and skills necessary to make informed choices about their health. These programs should be integrated into schools and communities, targeting both individual and community-level interventions. Early detection and treatment of mental health conditions are also crucial.
Furthermore, promoting healthy lifestyle choices, including balanced diets and regular physical activity, can significantly reduce the risk of preventable deaths. This approach needs to consider specific cultural contexts and socioeconomic factors. Furthermore, policies aimed at reducing exposure to environmental hazards and providing equitable access to healthcare are necessary.
Visualizing Future Trends
A compelling visualization of future trends in mortality rates for the 15-24 age group could take the form of a line graph. The x-axis would represent time (years), and the y-axis would display the mortality rate. Different colored lines could represent specific causes of death, such as accidents, suicides, or substance abuse-related deaths. The graph could also include shaded areas to highlight periods of increased or decreased mortality rates.
This visualization would clearly demonstrate the potential trajectory of mortality rates and any significant shifts. Further details about the visualization would include a legend, providing context for the different lines and their respective colors. A key would explain what the colored lines represent and their corresponding timeframes.
Estimated Timeframe
Potential future trends in mortality rates for the 15-24 age group are expected to unfold over a period of at least 10-20 years. This timeframe allows for the implementation and evaluation of prevention strategies, as well as the monitoring of emerging trends and challenges. The influence of long-term societal shifts and technological advancements on mortality rates is a complex issue.
Factors such as rising levels of chronic diseases and evolving social norms will also have a significant impact on the long-term mortality rates. It’s crucial to acknowledge that the pace of change is not always predictable, and the impact of emerging factors can vary.
Last Point: Top Causes Of Death For Ages 15 24
In conclusion, the top causes of death for young adults are multifaceted, involving a complex interplay of individual choices, societal factors, and access to healthcare. This analysis has illuminated the significance of addressing these issues to reduce mortality rates and promote well-being. By understanding the underlying factors and implementing effective prevention strategies, we can create a healthier future for young people worldwide.