Best time of day to take vitamin D is a crucial question for maximizing its benefits. Factors like sunlight exposure, dietary habits, and individual health conditions all play a role in how well your body absorbs vitamin D. This exploration delves into the science behind optimal vitamin D intake, from understanding circadian rhythms to the ideal timing of supplements.
Sunlight is a primary source, but its effectiveness depends on several variables. The time of day, season, and even your location can impact how much vitamin D your body produces. We’ll also look at how different types of vitamin D supplements might affect absorption rates, and how individual needs might vary.
Factors Affecting Vitamin D Absorption
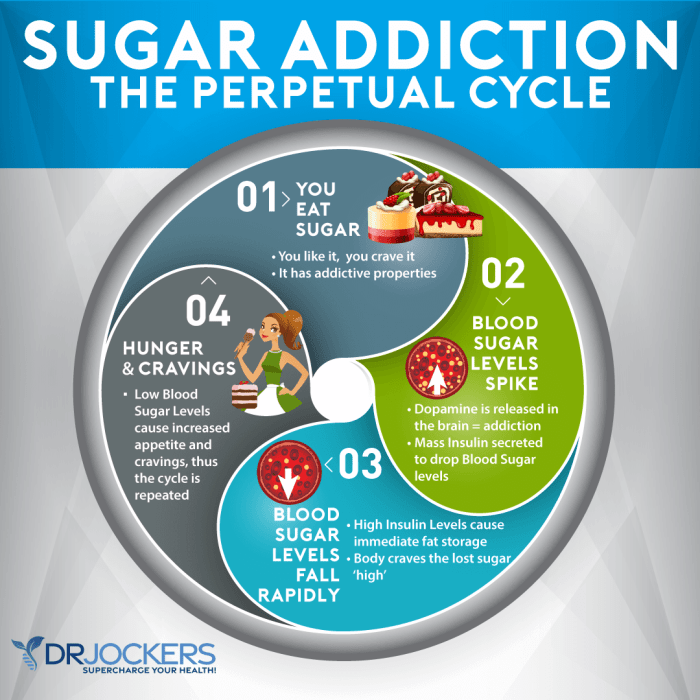
Vitamin D, crucial for bone health, immune function, and more, isn’t always readily absorbed by the body. Numerous factors influence its uptake, from dietary choices to individual health conditions. Understanding these factors allows for more informed strategies to optimize vitamin D levels.Dietary factors, lifestyle choices, and individual health conditions all play a significant role in vitamin D absorption. Different food sources offer varying amounts and forms of vitamin D, impacting absorption rates.
Taking vitamin D at the right time of day can really impact absorption, right? While researching the best time for optimal vitamin D intake, I stumbled across some fascinating insights into non surgical treatments for rotator cuff tears. Non surgical treatments for rotator cuff tears often involve targeted exercises and physical therapies, and it got me thinking about how the timing of my vitamin D supplement might be equally important for overall health.
So, back to the best time to take vitamin D – I’m still researching, but I’m leaning towards the morning for maximum benefits.
Sunlight exposure, skin pigmentation, and the body’s capacity to synthesize vitamin D are also key factors. Understanding these interconnections is essential for maintaining optimal vitamin D levels.
Dietary Factors Affecting Vitamin D Absorption, Best time of day to take vitamin d
Dietary factors play a substantial role in vitamin D absorption. The body’s ability to absorb vitamin D from food depends on the presence of other nutrients and the overall composition of the meal. For instance, consuming vitamin D alongside fats can enhance absorption.
- Fatty fish, such as salmon, tuna, and mackerel, are excellent sources of vitamin D. The fat content in these fish aids in the absorption process.
- Egg yolks and some cheeses also contain vitamin D, though in smaller amounts compared to fatty fish.
- Vitamin D-fortified foods, like milk and cereals, are crucial for individuals with limited dietary intake of vitamin D-rich foods.
- The presence of dietary fiber and oxalates can hinder vitamin D absorption, as they can bind to vitamin D, reducing its bioavailability.
Lifestyle Choices Impacting Vitamin D Absorption
Lifestyle choices have a direct impact on vitamin D levels. Regular physical activity, a balanced diet, and sufficient sun exposure are vital for optimal vitamin D status.
- Sun exposure is a primary source of vitamin D for many individuals. However, excessive sun exposure can increase the risk of skin damage.
- Individuals with darker skin pigmentation require longer sun exposure to synthesize the same amount of vitamin D as those with lighter skin.
- Certain medications, such as some anti-seizure medications and corticosteroids, can interfere with vitamin D metabolism and absorption.
- Lifestyle choices like smoking and alcohol consumption can negatively impact vitamin D levels.
Individual Health Conditions Affecting Vitamin D Absorption
Several health conditions can affect vitamin D absorption. Certain diseases can impact the body’s ability to process and utilize vitamin D.
- Chronic kidney disease can impair the body’s ability to convert vitamin D into its active form.
- Certain digestive disorders, like Crohn’s disease and celiac disease, can reduce the absorption of dietary vitamin D.
- Obesity can hinder vitamin D absorption due to the influence of adipose tissue on vitamin D metabolism.
- Age-related changes in the body can reduce the efficiency of vitamin D absorption.
Comparison of Vitamin D Absorption from Different Sources
Different sources of vitamin D affect absorption rates. The body’s efficiency in utilizing vitamin D from various sources varies.
| Factor | Description | Impact on Absorption |
|---|---|---|
| Sunlight Exposure | Vitamin D synthesis in the skin through UVB radiation from sunlight. | Efficient, but dependent on factors like time of day, season, and skin pigmentation. |
| Dietary Sources | Vitamin D obtained from food. | Dependent on the presence of other nutrients and the composition of the meal. |
| Supplements | Vitamin D supplements in various forms (e.g., pills, liquids). | Generally well-absorbed, but individual responses may vary. |
| Fortified Foods | Vitamin D added to food products like milk and cereals. | Can be a reliable source, but absorption rates depend on the food’s composition. |
The Role of Circadian Rhythms
Our internal body clock, the circadian rhythm, plays a significant role in regulating numerous physiological processes, including vitamin D metabolism. This rhythmic cycle influences when our bodies are most efficient at absorbing and utilizing certain nutrients. Understanding this connection can help us optimize our vitamin D intake for maximum benefit.Our bodies are finely tuned machines, responding to the natural cycles of day and night.
The circadian rhythm orchestrates a complex interplay of hormones and enzymes, including those crucial for vitamin D synthesis. This means that the time of day we expose ourselves to sunlight significantly impacts how our bodies process vitamin D.
Peak Vitamin D Production
The body produces vitamin D most effectively when exposed to ultraviolet B (UVB) radiation from sunlight. This process occurs primarily in the skin. While the optimal time for vitamin D production varies slightly depending on factors like latitude and individual skin tone, generally, peak production happens during the midday hours. The intensity of sunlight is strongest during this time, leading to more efficient vitamin D synthesis.
Influence of Sunlight Exposure Timing
The timing of sunlight exposure significantly impacts vitamin D levels. Exposure during the midday hours, when UVB radiation is strongest, results in higher vitamin D production compared to earlier or later in the day. This is because the intensity of the UVB rays is a key determinant in the process. Furthermore, factors like cloud cover and air pollution can also affect the amount of UVB reaching the skin, thus impacting vitamin D production.
Vitamin D Absorption Throughout the Day
| Time of Day | Absorption Rate | Reasons |
|---|---|---|
| Midday (12 PM – 2 PM) | Highest | Peak UVB radiation intensity. |
| Morning (8 AM – 12 PM) | Moderate | Lower UVB radiation intensity compared to midday. |
| Afternoon (2 PM – 6 PM) | Moderate | Lower UVB radiation intensity compared to midday. |
| Evening (6 PM onwards) | Lowest | Minimal UVB radiation. |
This table provides a general overview. Individual variations in skin tone, geographic location, and other factors can influence the precise timing of optimal vitamin D absorption.
Potential Effects of Different Time Zones
The optimal time for vitamin D intake is directly related to the local time zone. Individuals living in different time zones will experience different sunlight patterns and optimal times for vitamin D synthesis. For example, someone in a time zone with longer daylight hours will likely have more opportunities for vitamin D production during the midday hours. Conversely, those in time zones with shorter daylight hours might need to strategically plan their sun exposure times to maximize vitamin D production.
The timing of vitamin D intake is crucial for aligning with the natural rhythm of the body. Consistent sunlight exposure, particularly during midday hours, can lead to better overall vitamin D levels and contribute to better health.
Optimal Sunlight Exposure for Vitamin D
Sunlight is a crucial source of vitamin D for our bodies. Understanding the ideal conditions for sun exposure is vital for maximizing vitamin D production without increasing the risk of harm. Proper sun exposure can significantly contribute to overall well-being.Sunlight, particularly UVB rays, triggers the body’s production of vitamin D. This process is influenced by various factors, and the optimal approach involves understanding these factors to ensure a balance between benefit and safety.
Ideal Conditions for Sunlight Exposure
Sunlight exposure for vitamin D synthesis is most effective when the sun is high in the sky. This maximizes the intensity of UVB rays reaching the skin. The best time for exposure typically falls between 10 am and 3 pm, when the sun’s angle is more direct. Clear skies, without cloud cover, are essential for allowing UVB rays to penetrate the atmosphere and reach the skin.
Impact of Environmental Factors
Several environmental factors affect the amount of vitamin D our bodies synthesize from sunlight. Cloud cover significantly reduces the amount of UVB radiation reaching the earth’s surface. The presence of clouds can substantially decrease the effectiveness of sun exposure for vitamin D production.The time of year plays a critical role in vitamin D synthesis. During the winter months, when the sun’s angle is lower, less UVB radiation reaches the Earth’s surface.
This results in reduced vitamin D production compared to the summer months. For example, in northern latitudes, vitamin D production is significantly lower during the winter.Latitude also impacts vitamin D synthesis. Individuals living closer to the equator receive more direct sunlight throughout the year, leading to higher vitamin D production compared to those living further from the equator.
This is because the sun’s rays are more perpendicular to the Earth’s surface at the equator.
Risks of Excessive Sun Exposure
While sunlight is essential for vitamin D production, excessive exposure can lead to serious health risks. Prolonged and unprotected sun exposure can damage the skin, increasing the risk of premature aging, sunburn, and skin cancer. It’s crucial to balance the benefits of vitamin D synthesis with the potential dangers of excessive sun exposure.
Recommended Duration of Sunlight Exposure
The recommended duration of sunlight exposure varies based on skin type. Individuals with lighter skin types generally require less time to synthesize vitamin D compared to those with darker skin types. This is because darker skin contains more melanin, which acts as a natural sunscreen, absorbing more UVB radiation. It’s vital to consult with a healthcare professional to determine the appropriate exposure time based on individual skin type and other factors.
Optimal Sunlight Exposure Duration Table
| Location | Time of Year | Recommended Exposure Time (minutes) |
|---|---|---|
| Miami, Florida | Summer | 10-15 |
| Miami, Florida | Winter | 15-20 |
| London, England | Summer | 20-25 |
| London, England | Winter | 30-45 |
| Anchorage, Alaska | Summer | 30-45 |
| Anchorage, Alaska | Winter | 60+ (Consult a professional) |
This table provides a general guideline. Individual needs may vary, and it is essential to consult with a healthcare professional for personalized recommendations.
Supplement Timing Considerations
Knowing the best time to take your vitamin D supplement is crucial for maximizing absorption and effectiveness. This goes beyond simply popping a pill; factors like meal timing and supplement form play significant roles in how your body utilizes this vital nutrient. Understanding these considerations allows you to make informed choices for optimal vitamin D levels.Supplement timing is not just about when you take it, but also how it interacts with other components of your diet and daily routine.
This section will delve into the specifics of meal timing, supplement types, and potential interactions to help you choose the optimal vitamin D intake strategy.
Meal Timing and Absorption
Proper meal timing significantly impacts vitamin D absorption. Consuming vitamin D with a meal containing healthy fats enhances absorption. Dietary fats help emulsify the vitamin D, making it more readily available for your body to absorb. A balanced meal, rich in healthy fats like those found in avocados, nuts, or fatty fish, can optimize vitamin D uptake.
While the best time of day to take vitamin D is often debated, recent research suggests it might not matter too much. However, if you’re experiencing skin peeling on hands, this could indicate a deficiency in vitamins or minerals , and in that case, a consultation with a doctor is highly recommended. Regardless, consistency in taking your vitamin D is key, no matter what time of day you choose.
This ensures that your body effectively utilizes the vitamin D you’re providing through supplementation.
Supplement Form and Absorption Rates
Different vitamin D supplement forms, such as vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol), exhibit varying absorption rates. Vitamin D3 is generally considered more bioavailable and effective in raising blood levels compared to vitamin D2. This is because vitamin D3 is structurally more similar to the vitamin D your body naturally produces.
Comparison of Vitamin D2 and D3
| Feature | Vitamin D2 (Ergocalciferol) | Vitamin D3 (Cholecalciferol) |
|---|---|---|
| Source | Plant-based | Animal-based (and can be produced by the body) |
| Bioavailability | Lower | Higher |
| Effectiveness | Often requires higher doses to achieve similar effects | Generally more effective at raising blood levels |
| Potential interactions | May interact with certain medications | Generally fewer reported interactions |
The table above highlights the key differences between the two forms. While vitamin D2 is a valuable source, vitamin D3 generally demonstrates superior absorption and efficacy. This doesn’t necessarily mean vitamin D2 is ineffective, but that vitamin D3 is often preferred for its efficiency.
Interactions with Medications
Certain medications can interact with vitamin D supplements, potentially affecting their absorption or efficacy. If you are taking any other medications, including those for high blood pressure, heart conditions, or cholesterol management, consult your doctor before starting vitamin D supplementation. This precaution ensures there are no unintended consequences due to drug interactions.
Figuring out the best time of day to take Vitamin D can be tricky, but it’s definitely not as complicated as trying to determine if you can get pregnant during your period! Recent studies suggest that absorption might be slightly better when taken with a meal, which makes it easier to remember. However, if you’re interested in learning more about the possibility of conception during menstruation, check out this insightful article on can you get pregnant while on period.
Ultimately, consistency is key, regardless of the time of day. Just try to stick to a routine that works for you.
Step-by-Step Guide for Choosing the Best Time
- Identify your dietary habits: Consider your usual meal patterns and the presence of healthy fats in your meals. Aim for meals that include healthy fats when taking vitamin D supplements.
- Evaluate your supplement type: If possible, choose vitamin D3 over vitamin D2, as it is generally more readily absorbed and effective.
- Consult with your doctor: If you’re taking other medications, or have any underlying health conditions, consult your physician to avoid potential interactions.
- Monitor your vitamin D levels: Regular blood tests can help you determine your vitamin D levels and ensure that your supplementation strategy is effective.
- Adjust as needed: Based on the results of your blood tests and your doctor’s guidance, adjust your supplementation schedule and/or dosage to maintain optimal vitamin D levels.
Individual Variability and Recommendations

Understanding your unique body and lifestyle is crucial for determining the right vitamin D intake. Individual factors like age, health conditions, and genetics play a significant role in how your body absorbs and utilizes vitamin D. This personalized approach is essential for achieving optimal vitamin D levels without unnecessary supplementation or potential risks.Personalized vitamin D recommendations are tailored to address individual needs and ensure optimal health outcomes.
This approach recognizes the diverse ways individuals process and utilize vitamin D, accounting for factors beyond simple sunlight exposure and supplementation. A personalized approach considers specific needs and factors that can impact vitamin D absorption and metabolism.
Factors Affecting Vitamin D Intake by Age Group
Age significantly influences vitamin D absorption and metabolism. Children, adolescents, and older adults have different requirements compared to adults in their prime. Factors like changing bone density, hormonal changes, and overall health status contribute to these age-specific needs. Meeting these age-specific needs is important for maintaining optimal bone health and overall well-being throughout life.
- Children and Adolescents: Growing bodies require adequate vitamin D for healthy bone development and growth. Insufficient vitamin D during these crucial periods can lead to skeletal deformities and increased risk of fractures later in life. Dietary intake and sunlight exposure are essential for meeting their specific needs.
- Adults: Maintaining healthy vitamin D levels is important for overall well-being, including muscle function, immune support, and mood regulation. Individual needs vary based on factors like lifestyle and health conditions.
- Older Adults: The absorption and utilization of vitamin D often decline with age. This is due to decreased sun exposure, reduced efficiency of vitamin D production, and potential health conditions. This group may require higher doses of vitamin D supplementation to maintain optimal levels.
Assessing Individual Vitamin D Needs
Determining individual vitamin D needs involves a combination of factors. Blood tests are crucial for assessing current vitamin D levels. A blood test, specifically a 25-hydroxyvitamin D test, provides a precise measurement of vitamin D in the body. These tests are vital for tailoring recommendations to individual needs.
Importance of Professional Consultation
Consulting a healthcare professional is crucial for personalized vitamin D advice. A healthcare professional can evaluate individual needs, health conditions, and lifestyle factors to provide tailored recommendations. This professional evaluation can help avoid potential risks associated with incorrect or excessive supplementation. A healthcare provider can assess the need for supplementation and provide guidance on the best course of action.
Individual Factors and Vitamin D Intake Recommendations
| Individual Factor | Impact on Vitamin D Absorption | Recommendations for Optimal Intake Time |
|---|---|---|
| Age | Absorption and metabolism vary significantly with age. Children and older adults may require adjustments. | Tailored to age-specific needs, considering growth stages, bone health, and overall well-being. |
| Health Conditions | Certain conditions like kidney disease, liver disease, or malabsorption syndromes can affect vitamin D metabolism. | Consult a healthcare professional for personalized recommendations. Dietary modifications may be necessary. |
| Genetics | Genetic variations can influence vitamin D receptor activity and absorption. | Consult a healthcare professional to determine optimal intake and potential need for supplementation. |
| Lifestyle | Sun exposure, diet, and physical activity can impact vitamin D levels. | Adjusting intake based on individual lifestyle choices. Regular blood tests are vital. |
Potential Health Implications of Timing: Best Time Of Day To Take Vitamin D

The optimal time to take vitamin D supplements isn’t just about absorption; it also potentially impacts how your body utilizes this crucial nutrient. Understanding the potential benefits and drawbacks of different intake times can help you tailor your vitamin D regimen for maximum health impact. Different biological processes occurring at various times of the day might influence how your body responds to vitamin D, impacting its overall effect on your well-being.Taking vitamin D at a time when your body is most receptive to its effects could maximize its potential benefits.
Conversely, taking it at a less optimal time might diminish its impact or even introduce potential drawbacks. Furthermore, inconsistencies in intake could negatively affect overall health outcomes. This section will delve into the potential health implications of varying vitamin D intake times.
Potential Benefits and Drawbacks of Different Intake Times
Different times of day may influence how your body processes vitamin D, potentially affecting various health aspects. The timing of vitamin D intake might impact its interaction with other bodily functions and processes.
- Morning Intake: Taking vitamin D in the morning could align with peak absorption rates and potentially enhance its role in supporting immune function, particularly during the day when immune responses are needed. However, potential drawbacks might include disruption to circadian rhythm if taken too early or with breakfast, and potential interactions with morning medications. This may be less of a concern for those who are generally less sensitive to the timing of intake.
- Evening Intake: Evening intake could potentially support sleep quality and bone health, which are often more active during this time. However, if taken too late, it might interfere with sleep, as some individuals might be more sensitive to vitamin D’s potential stimulating effects. For instance, evening intake might be beneficial for older adults whose bone remodeling activity tends to peak at night.
- Mid-day Intake: Mid-day intake might align with other meals and routines, potentially aiding in overall nutrient balance. However, it might be less impactful compared to other times due to potentially lower absorption rates at this time. It is also important to note that individual factors may affect the ideal timing, as some people might not feel the effects of vitamin D as quickly as others.
Potential Links to Health Outcomes
Vitamin D intake timing might have noticeable effects on specific health areas.
- Bone Health: Consistent vitamin D intake, ideally timed with peak bone remodeling activity, could potentially enhance bone density and strength. However, inconsistent intake could lead to fluctuations in calcium absorption and potentially weaken bones over time. For example, elderly individuals might benefit from a late-afternoon vitamin D intake to support bone remodeling that occurs more prominently during this time of day.
But a different schedule may be better for other groups.
- Immune Function: Optimal vitamin D timing could potentially enhance the body’s ability to fight off infections. However, if taken at a time that disrupts normal bodily functions, it might not produce the same effect. Individuals with weakened immune systems or those frequently exposed to pathogens might benefit from a more strategic intake schedule.
- Mood and Sleep: Vitamin D is associated with mood regulation. Taking vitamin D at the right time might enhance these benefits. However, if intake disrupts sleep patterns, it could negatively affect mood and overall well-being. This might be particularly important for individuals with seasonal affective disorder (SAD) or other mood-related conditions.
Inconsistent Intake and Overall Well-being
Maintaining consistent vitamin D intake, whether through sunlight exposure or supplements, is vital for overall well-being.
- Impact on Health Conditions: Inconsistent vitamin D intake might lead to fluctuating blood levels, potentially affecting various bodily functions. For example, inconsistent vitamin D levels could negatively impact blood sugar regulation in individuals with diabetes.
- Overall Well-being: A consistent schedule might promote stability in bodily functions and better overall well-being. For example, a daily vitamin D intake schedule might help maintain a more consistent level of vitamin D in the body.
Comparison Table
| Time of Day | Potential Benefits | Potential Drawbacks |
|---|---|---|
| Morning | Potentially enhanced immune function, alignment with peak absorption | Potential disruption of circadian rhythm, interactions with morning medications |
| Evening | Potential support for sleep quality, bone health | Potential interference with sleep, individual sensitivities to stimulation |
| Mid-day | Alignment with meals, potentially aiding in overall nutrient balance | Potentially less impactful compared to other times due to absorption rates |
Summary
Ultimately, the best time to prioritize vitamin D intake is a personalized decision. By understanding the complex interplay of sunlight, supplements, and individual factors, you can make informed choices to support your overall health and well-being. Remember, consulting a healthcare professional is essential for personalized recommendations.