Types of rheumatoid arthritis sets the stage for this enthralling narrative, offering readers a glimpse into the complexities of this chronic autoimmune disease. We’ll explore the various forms of rheumatoid arthritis, examining their unique characteristics, symptoms, and treatment approaches. Understanding the different types is crucial for effective management and a better quality of life.
This comprehensive guide will delve into the intricacies of each type, comparing and contrasting their symptoms, causes, and prognoses. From the initial diagnosis to ongoing management, we’ll cover the full spectrum of rheumatoid arthritis, providing valuable insights and practical information for those affected and those seeking to understand the disease better.
Introduction to Rheumatoid Arthritis
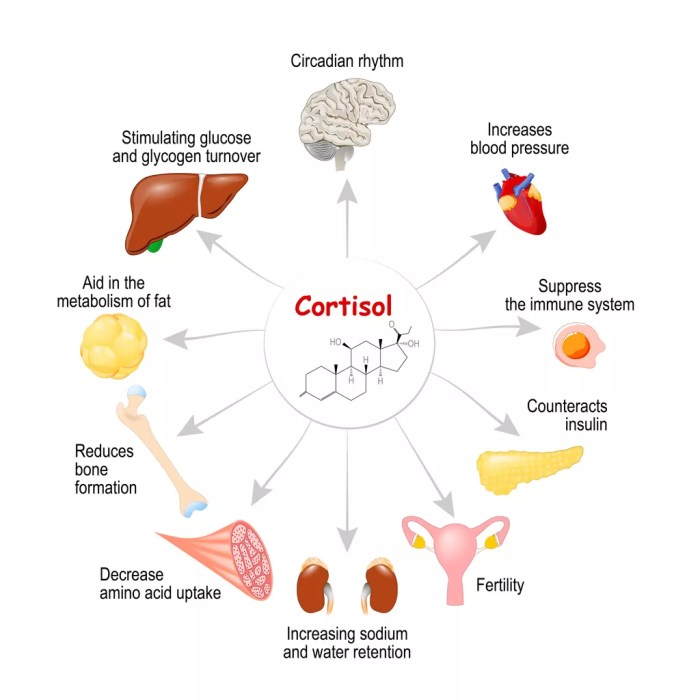
Rheumatoid arthritis (RA) is a chronic autoimmune disease that primarily affects the joints. It’s characterized by inflammation of the synovial lining, the membrane that cushions and lubricates joints. This inflammation can lead to pain, swelling, stiffness, and eventually, joint damage. Understanding RA’s various effects is crucial for effective management and treatment.The general characteristics of RA include persistent inflammation, often symmetrical involvement of joints, and the potential for systemic manifestations beyond the joints.
This means that RA can impact more than just the joints, potentially affecting other organs and systems in the body. Early diagnosis and appropriate treatment are vital for controlling the disease and minimizing long-term complications.
Different Ways Rheumatoid Arthritis Affects the Body
RA’s impact extends beyond the joints. It can manifest in a variety of ways, influencing overall well-being and quality of life. These extra-articular manifestations are crucial to recognize for comprehensive management.
- Joint inflammation and damage: This is a key feature of RA, leading to pain, swelling, stiffness, and ultimately, joint destruction. The inflammation can erode cartilage and bone, resulting in deformities and loss of function. Examples include hand deformities (like ulnar deviation) and difficulty with everyday tasks.
- Systemic effects: RA can also affect other organs and systems in the body. These systemic manifestations can vary in severity and include fatigue, fever, and weight loss. Some individuals may experience inflammation in the lungs (pleuritis) or the heart (pericarditis), potentially leading to cardiovascular complications. The involvement of the lungs, for instance, can result in reduced lung capacity, impacting breathing.
- Other potential complications: RA can increase the risk of developing other health problems. This includes an increased risk of cardiovascular disease, eye inflammation (scleritis), and certain types of cancers. For example, studies have shown a correlation between RA and an elevated risk of cardiovascular issues, emphasizing the importance of comprehensive cardiovascular health monitoring for individuals with RA.
Symptoms and Affected Areas of Rheumatoid Arthritis
Understanding the symptoms and affected areas is crucial for early diagnosis and treatment. This information helps in distinguishing RA from other conditions and guides appropriate management strategies.
| Disease | Symptoms | Affected Areas |
|---|---|---|
| Rheumatoid Arthritis | Pain, stiffness, swelling, warmth, and redness in affected joints; fatigue, fever, weight loss (in some cases); potential for extra-articular manifestations | Hands, wrists, feet, knees, ankles, elbows, shoulders, hips, neck; potentially other organs (lungs, heart, eyes, etc.) |
Types of Rheumatoid Arthritis
Rheumatoid arthritis (RA) isn’t a single entity; it encompasses various subtypes, each with its own characteristics. Understanding these distinctions is crucial for accurate diagnosis and personalized treatment plans. While the fundamental nature of RA—an autoimmune disorder causing chronic inflammation of the joints—remains consistent across these subtypes, variations in symptom presentation, progression, and response to treatment exist.The classification of rheumatoid arthritis types is often based on the severity, duration, and specific characteristics of the disease.
These classifications, though sometimes evolving, help healthcare professionals tailor treatment approaches for optimal patient outcomes.
Classification of Rheumatoid Arthritis Subtypes
Different classifications exist for rheumatoid arthritis, but a general approach involves differentiating based on the disease’s duration, severity, and the pattern of joint involvement. While these classifications can be helpful, they are not always distinct and overlap can occur. Important factors in distinguishing types include the speed of progression, the pattern of joint involvement, and the presence of extra-articular manifestations (beyond the joints).
Clinical Presentation and Progression
Understanding the clinical presentation and progression of various types of RA is vital for timely intervention and management. The symptoms and severity of RA can vary significantly between individuals, even within the same type. This variability emphasizes the importance of individualized treatment plans tailored to the specific needs of each patient.
Diagnostic Criteria
Accurate diagnosis of RA subtypes relies on established diagnostic criteria. These criteria usually incorporate a combination of clinical findings, laboratory tests, and imaging studies. The American College of Rheumatology (ACR) and the European League Against Rheumatism (EULAR) criteria are commonly used. These criteria, while evolving, remain crucial for defining RA and its subtypes.
| Type | Common Symptoms | Typical Progression |
|---|---|---|
| Early-onset RA | Insidious onset, often with symmetrical joint pain, stiffness, and swelling, primarily in the smaller joints. | Can progress rapidly in some individuals, while others may have a more gradual course. Early diagnosis and treatment are crucial to minimize joint damage. |
| Established RA | Chronic inflammation, potentially leading to joint deformity, erosion, and functional limitations. Symptoms are typically more persistent and widespread compared to early-onset RA. | Progression varies significantly. Some individuals experience periods of remission, while others experience persistent or worsening symptoms. Disease-modifying antirheumatic drugs (DMARDs) are often necessary for controlling the disease. |
| Juvenile Idiopathic Arthritis (JIA) | Rheumatoid symptoms that begin before age 16. Symptoms may include joint pain, swelling, stiffness, fever, and rash. | Progression varies considerably. Some cases may resolve spontaneously, while others may lead to permanent joint damage if not managed promptly. Treatment focuses on controlling inflammation and preserving joint function. |
Symptoms and Diagnosis
Understanding the symptoms and diagnostic process is crucial for early intervention and effective management of rheumatoid arthritis. Early diagnosis allows for prompt treatment, potentially minimizing long-term joint damage and improving overall quality of life. Accurate diagnosis relies on a combination of clinical evaluation, patient history, and specific diagnostic tests.
Common Symptoms
The symptoms of rheumatoid arthritis can vary in severity and presentation, even among different types. Recognizing these symptoms is vital for prompt medical attention. Common symptoms often include pain, stiffness, and swelling in the affected joints.
- Joint pain and stiffness, particularly in the morning or after periods of inactivity. This stiffness often lasts for at least 30 minutes.
- Swelling and warmth around the affected joints. This swelling can cause the joints to appear larger and feel tender to the touch.
- Fatigue and general malaise. This can be a significant symptom and often accompanies the joint pain and stiffness.
- Loss of function in the affected joints. This can range from mild difficulty performing everyday tasks to significant impairment.
- Systemic symptoms, such as fever, weight loss, and loss of appetite. These symptoms may indicate a more severe form of the disease.
Diagnostic Process
The diagnostic process for rheumatoid arthritis involves a thorough evaluation of the patient’s medical history, a physical examination, and specific diagnostic tests. Physicians consider the duration and pattern of symptoms, as well as any potential contributing factors.
A crucial part of the diagnostic process is ruling out other conditions that may mimic rheumatoid arthritis symptoms. This may involve blood tests, imaging scans, and even joint aspiration, if necessary. The goal is to pinpoint the underlying cause of the symptoms and confirm a diagnosis of rheumatoid arthritis, or another condition.
Diagnostic Tests
Several tests are employed to confirm the diagnosis of rheumatoid arthritis, including various blood tests and imaging studies.
- Rheumatoid factor (RF) test: This blood test detects the presence of rheumatoid factor, an antibody that is often found in people with rheumatoid arthritis. However, the presence of RF is not specific to rheumatoid arthritis, as it can be found in other conditions.
- Anti-cyclic citrullinated peptide (anti-CCP) antibody test: This test detects antibodies directed against proteins that have been modified. Anti-CCP antibodies are highly specific for rheumatoid arthritis and are often present before the onset of noticeable symptoms.
- Complete blood count (CBC): This blood test measures various components of the blood, including red blood cells, white blood cells, and platelets. Changes in these components may indicate inflammation.
- Erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP): These blood tests measure markers of inflammation. Elevated levels of ESR or CRP often suggest inflammation, which is characteristic of rheumatoid arthritis.
- Imaging studies: X-rays and other imaging techniques (e.g., ultrasound, MRI) may be used to visualize the joints and identify structural damage. These studies can help assess the extent of the disease and monitor its progression over time.
Comparison of Symptoms and Diagnostic Methods
| Type of Rheumatoid Arthritis | Common Symptoms | Diagnostic Methods |
|---|---|---|
| Rheumatoid Arthritis (RA) | Joint pain, stiffness, swelling, fatigue, potential systemic symptoms | RF, anti-CCP, CBC, ESR/CRP, imaging studies |
| Juvenile Idiopathic Arthritis (JIA) | Similar to RA but often affects children and adolescents; can present with eye inflammation, skin rashes, and growth issues | RF, anti-CCP, CBC, ESR/CRP, imaging studies, possibly genetic testing or specific markers for JIA |
| Psoriatic Arthritis | Joint pain, stiffness, swelling, often accompanied by skin conditions like psoriasis | RF, anti-CCP, CBC, ESR/CRP, imaging studies, assessment of skin conditions |
Treatment and Management
Rheumatoid arthritis, while not curable, is highly manageable. Effective treatment focuses on reducing inflammation, controlling symptoms, and preventing long-term joint damage. Early intervention is crucial for slowing disease progression and improving quality of life. Different treatment approaches are tailored to the individual’s specific needs and disease activity.Understanding the available treatment options, potential side effects, and the importance of symptom management is vital for successful RA management.
Understanding the different types of rheumatoid arthritis is crucial for effective management. While focusing on physical health is essential, consider exploring the potential benefits of supplements for brain health, such as those found at supplements for brain health. Ultimately, a holistic approach, combining medical guidance with potentially beneficial lifestyle choices, can significantly impact managing the diverse forms of rheumatoid arthritis.
This section details the diverse range of therapies used to treat the different types of rheumatoid arthritis, highlighting the importance of patient-physician collaboration and ongoing monitoring.
Medication Strategies
Various medications play a key role in managing rheumatoid arthritis. These medications target different aspects of the inflammatory process, aiming to reduce pain, stiffness, and swelling. Different classes of medications are used depending on the severity of the disease and the individual’s response.
- Disease-modifying antirheumatic drugs (DMARDs): These medications aim to slow or stop the progression of joint damage. They work by suppressing the immune system’s overactive response, which is central to the inflammatory process in RA. Examples include methotrexate, sulfasalazine, leflunomide, hydroxychloroquine, and biologics. The choice of DMARD depends on the specific type of RA and the patient’s overall health.
- Corticosteroids: These potent anti-inflammatory medications can rapidly reduce inflammation and pain. They are often used in combination with other medications to manage flares or acutely painful episodes. However, long-term use of corticosteroids can lead to significant side effects, so they are typically used short-term.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): These over-the-counter and prescription medications help reduce pain and inflammation. They are often used as a first-line treatment for mild to moderate symptoms, but they don’t modify the disease course. Examples include ibuprofen, naproxen, and celecoxib. NSAIDs can have gastrointestinal side effects, so they should be used cautiously and under medical supervision.
- Biologics: These targeted therapies are a newer class of DMARDs that precisely target specific proteins involved in the inflammatory response. They are typically reserved for cases where other DMARDs have not been effective. Biologics can significantly improve disease activity and reduce joint damage, but they can also carry a higher risk of specific side effects. Examples include TNF inhibitors (e.g., adalimumab, etanercept), interleukin-6 inhibitors, and T-cell inhibitors.
Symptom Management Techniques
Effective RA management extends beyond medication. Symptom management plays a crucial role in improving quality of life. Techniques like regular exercise, heat and cold therapy, and occupational therapy can significantly reduce stiffness, pain, and fatigue.
- Physical Therapy: Physical therapists can develop tailored exercise programs to improve joint mobility, strength, and endurance. This is essential for maintaining function and preventing further joint damage.
- Occupational Therapy: Occupational therapists can help individuals adapt their daily routines to accommodate the limitations imposed by RA. This includes modifying activities, using assistive devices, and optimizing home environments.
- Assistive Devices: Adaptive devices, such as splints, braces, and ergonomic tools, can help compensate for joint pain and weakness. These devices can help maintain independence and reduce the strain on affected joints.
Treatment Efficacy and Side Effects
The effectiveness of treatment for rheumatoid arthritis varies depending on the specific type of RA, the individual’s response to medication, and adherence to treatment plans.
| Treatment Type | Potential Side Effects | Overall Efficacy |
|---|---|---|
| Disease-modifying antirheumatic drugs (DMARDs) | Gastrointestinal upset, liver damage, mouth sores, bone marrow suppression | Generally effective in slowing disease progression, but individual responses vary. |
| Corticosteroids | Weight gain, osteoporosis, high blood pressure, cataracts, infections | Highly effective in reducing inflammation, but long-term use is associated with significant side effects. |
| Nonsteroidal anti-inflammatory drugs (NSAIDs) | Gastrointestinal bleeding, kidney problems, high blood pressure | Effective in managing pain and inflammation, but not disease-modifying. |
| Biologics | Increased risk of infections, allergic reactions, and certain types of cancers | Highly effective in reducing disease activity and preventing joint damage in patients who do not respond to other treatments. |
Risk Factors and Prevention
Understanding the risk factors for rheumatoid arthritis (RA) is crucial for both prevention and early detection. While a definitive cause remains elusive, researchers have identified several potential contributing elements. Knowing these factors can help individuals make informed lifestyle choices and potentially reduce their risk of developing this complex autoimmune disease.
Potential Risk Factors
Several factors can increase a person’s susceptibility to rheumatoid arthritis. These include genetic predisposition, environmental triggers, and certain lifestyle choices. Genetic factors play a significant role. Family history of RA is a strong indicator, suggesting a genetic link. Certain genes may make individuals more susceptible to developing the disease.
Environmental triggers, such as exposure to certain infections or environmental toxins, have also been implicated. Some research suggests that smoking can increase the risk of RA.
Lifestyle Choices and Their Impact
Lifestyle choices play a crucial role in managing potential risk factors for RA. Maintaining a healthy weight is important, as obesity is linked to an increased risk of developing several chronic diseases, including RA. A balanced diet rich in fruits, vegetables, and whole grains is essential for overall health and may contribute to a reduced risk. Regular physical activity is beneficial for both physical and mental well-being, and may help mitigate some risk factors.
Preventive Measures
While there’s no guaranteed way to prevent RA, several preventative measures can potentially reduce the likelihood of developing the disease. These include maintaining a healthy weight, adopting a balanced diet, and engaging in regular physical activity. Quitting smoking is a significant step to reducing various health risks. Managing stress effectively is also important, as stress can affect the body’s immune response.
Early detection and treatment of any existing health conditions, such as infections, can potentially reduce the risk of developing RA.
Summary Table
| Risk Factor | Preventive Measure | Efficacy |
|---|---|---|
| Family history of RA | Maintaining a healthy lifestyle | While not eliminating the risk, a healthy lifestyle can help mitigate other risk factors. |
| Smoking | Quitting smoking | Significant reduction in risk. Studies show a clear correlation between smoking and RA development. |
| Obesity | Maintaining a healthy weight through diet and exercise | Research suggests a correlation between obesity and increased RA risk. |
| Environmental factors (e.g., infections) | Maintaining good hygiene and addressing potential exposures. | While some factors are impossible to avoid, minimizing potential exposures can reduce risk. |
| Stress | Stress management techniques (e.g., yoga, meditation) | Managing stress can potentially help maintain overall health and well-being. |
Living with Rheumatoid Arthritis
Living with rheumatoid arthritis (RA) is a multifaceted journey that extends beyond managing physical symptoms. It encompasses emotional, social, and practical challenges that require proactive strategies for coping and well-being. Understanding these aspects is crucial for individuals navigating this condition and developing a supportive approach to daily life.Living with RA often involves adjusting to persistent pain, fatigue, and limitations in mobility.
These physical challenges can significantly impact daily routines, work, and social interactions. The chronic nature of RA also introduces emotional hurdles, such as anxiety, depression, and feelings of isolation. Addressing these emotional and social factors is just as important as managing the physical aspects of the disease.
Emotional Well-being and Support
Emotional well-being is integral to managing RA effectively. Experiencing persistent pain and limitations can lead to feelings of frustration, anger, and sadness. Recognizing and acknowledging these emotions is the first step towards coping. Seeking support from trusted friends, family, or support groups is crucial. Connecting with others who understand the unique challenges of living with RA can provide a sense of community and shared experience.
Social Implications and Support Networks
Social life can be impacted by RA. Maintaining relationships and participating in social activities can become more challenging due to fatigue, pain, and limitations. Open communication with loved ones about the condition’s effects is vital for understanding and support. Joining support groups or online forums provides a safe space for connecting with others facing similar experiences and sharing coping strategies.
This can foster a sense of community and provide valuable insights into how others are managing their lives with RA.
Self-Management Strategies
Effective self-management plays a central role in improving quality of life for individuals with RA. This involves developing a personalized plan to manage symptoms and daily challenges. Prioritizing rest and sleep, incorporating regular exercise (with guidance from healthcare professionals), and adopting healthy eating habits are crucial components of self-management. Regular communication with healthcare providers is vital for monitoring disease activity, adjusting treatment plans, and addressing any concerns.
Understanding the different types of rheumatoid arthritis is crucial for effective management. While researching this, I stumbled upon an interesting correlation with triple negative breast cancer recurrence after mastectomy, which is a complex and often challenging situation. Triple negative breast cancer recurrence after mastectomy highlights the need for comprehensive support and tailored treatment plans. Ultimately, different types of rheumatoid arthritis each require specific approaches to ensure the best possible outcomes.
Adapting to Daily Challenges
Adapting to daily challenges is an essential aspect of living with RA. Finding ways to simplify tasks, utilize assistive devices, and adjust routines to accommodate symptoms can significantly improve daily functioning. For example, a person with RA might utilize a standing desk or ergonomic chair at work to manage fatigue and discomfort. These adjustments not only enhance physical comfort but also boost self-efficacy and empower individuals to maintain a fulfilling lifestyle.
Symptom Management and Healthy Lifestyle
Managing symptoms and maintaining a healthy lifestyle are intertwined. Different types of RA may require different symptom management approaches. A combination of medication, physical therapy, and lifestyle choices can help minimize pain, stiffness, and fatigue. Regular exercise, a balanced diet, and stress-reduction techniques can all play a significant role in overall well-being and managing RA symptoms. Maintaining a positive mindset and seeking support from healthcare professionals and support groups are crucial in this process.
Understanding the different types of rheumatoid arthritis is crucial for effective management. While some forms might not directly affect digestion, others can potentially impact the liver or gallbladder, leading to issues like pale or clay-colored stools. If you’re experiencing this, it’s essential to consult your doctor to determine the underlying cause, like potential digestive complications from certain types of rheumatoid arthritis.
For a better understanding of what might be causing this discoloration, check out this helpful resource: what can cause pale or clay colored stool. Ultimately, recognizing the different types of rheumatoid arthritis is key to personalized treatment and overall well-being.
For instance, incorporating yoga or Tai Chi can help manage pain and improve flexibility for those with RA.
Support Groups and Resources
Numerous support groups and resources are available to assist individuals with RA. Local support groups offer opportunities for peer-to-peer interaction, sharing experiences, and learning coping strategies. Online forums and websites provide access to a broader network of individuals living with RA. Healthcare professionals, such as rheumatologists, physical therapists, and occupational therapists, play a crucial role in providing guidance and support.
Organizations dedicated to RA also offer educational materials and support services. These resources can offer invaluable assistance in navigating the challenges of living with RA.
Illustrative Case Studies: Types Of Rheumatoid Arthritis
Understanding rheumatoid arthritis (RA) through real-life examples is crucial for comprehending the diverse ways it affects individuals. These case studies highlight the variations in symptom presentation, disease progression, and treatment responses. They emphasize that RA isn’t a one-size-fits-all condition, and personalized approaches to care are vital.These illustrative cases provide a glimpse into the complexities of RA. Each individual experience, while unique, underscores the importance of early diagnosis, prompt treatment, and ongoing patient support in managing the disease effectively.
Case Study 1: Early-Onset Aggressive RA
“A 28-year-old woman, Sarah, presented with severe morning stiffness and swelling in her wrists and hands. Within weeks, the inflammation spread to her ankles and knees. Laboratory tests revealed elevated inflammatory markers and positive rheumatoid factor. Rapidly progressive joint damage was evident on X-rays, necessitating aggressive treatment with disease-modifying antirheumatic drugs (DMARDs) and biologics to prevent long-term disability.”
This case exemplifies early-onset aggressive RA, where symptoms escalate rapidly. The swift progression highlights the importance of prompt diagnosis and aggressive treatment to halt joint damage and preserve function. Aggressive therapies like DMARDs and biologics were crucial to manage the condition effectively and prevent further joint deterioration.
Case Study 2: Seronegative RA
“A 55-year-old man, David, experienced insidious onset of fatigue and joint pain, primarily affecting his hips and lower back. He did not exhibit the typical rheumatoid factor or anti-CCP antibodies. Symptoms progressed gradually over several years, leading to significant mobility limitations. Treatment initially focused on pain management and physical therapy, eventually incorporating DMARDs to slow the disease progression.”
This case illustrates seronegative RA, where the characteristic autoantibodies are absent. The gradual onset and specific joint involvement (hips and lower back) provide insight into the varied presentation of RA. The need for a tailored treatment approach, including a combination of non-pharmacological and pharmacological interventions, is evident in this scenario.
Case Study 3: Juvenile Idiopathic Arthritis (JIA)
“A 10-year-old girl, Emily, developed persistent joint pain and swelling in her knees and elbows. Physical examination revealed inflammation in multiple joints. Laboratory tests revealed elevated inflammatory markers, but the presence of rheumatoid factor was negative. Treatment focused on reducing inflammation and pain, along with supporting her overall well-being and physical development.”
This case highlights JIA, which affects children and adolescents. The focus on managing inflammation and maintaining the child’s physical and developmental progress is critical. The treatment plan must be adaptable to address the unique needs of the child.
Case Study 4: RA with Systemic Manifestations
“A 60-year-old woman, Maria, experienced joint pain and swelling, accompanied by fever, fatigue, and skin rashes. Laboratory tests revealed elevated inflammatory markers, positive rheumatoid factor, and evidence of vasculitis. Treatment involved a multidisciplinary approach, including DMARDs, corticosteroids, and interventions to manage the systemic manifestations.”
This case exemplifies RA with systemic involvement. The combination of joint inflammation with systemic symptoms like fever and skin rashes requires a comprehensive treatment strategy. The need for a multidisciplinary approach, involving specialists in various fields, is evident in this scenario.
Research and Future Directions
Rheumatoid arthritis (RA) research is a dynamic field, constantly evolving with new discoveries and innovative approaches. This ongoing investigation into the intricacies of RA is crucial for refining diagnostics, developing more effective therapies, and ultimately improving the lives of those affected. Understanding the diverse subtypes of RA and their underlying mechanisms is pivotal for targeted treatments.Current research efforts are focusing on multiple fronts, aiming to understand the disease’s pathogenesis better, identify biomarkers for early detection, and explore novel therapeutic targets.
Scientists are also working to improve existing treatments and develop entirely new approaches to manage RA’s debilitating symptoms and prevent long-term complications.
Current Research Focuses
A multitude of research avenues are being explored to better understand and manage rheumatoid arthritis. Researchers are investigating the genetic and environmental factors contributing to RA development, aiming to identify individuals at high risk. This knowledge could lead to preventative measures and earlier interventions.
Ongoing Efforts to Find New Treatments and Cures, Types of rheumatoid arthritis
Significant progress is being made in developing innovative therapies. Research is exploring the potential of targeted therapies that directly address specific inflammatory pathways involved in RA. These targeted approaches aim to minimize side effects and maximize treatment efficacy.
Importance of Continued Research
The importance of continued research into rheumatoid arthritis cannot be overstated. Improved understanding of the disease’s complexities will pave the way for more personalized treatment strategies. Early diagnosis, tailored interventions, and preventative measures will become increasingly attainable with continued research efforts. This will ultimately lead to improved quality of life for individuals living with RA.
Summary of Current Research Findings and Future Research Directions
| Research Topic | Findings | Next Steps |
|---|---|---|
| Genetic Predisposition | Several genes have been linked to an increased risk of developing RA, and research is identifying specific genetic variations associated with different subtypes of RA. | Further investigation into gene-environment interactions to pinpoint individuals at high risk and develop personalized preventative strategies. |
| Biomarker Discovery | Studies are identifying potential biomarkers that could predict disease activity and response to treatment. This could lead to earlier diagnosis and more effective treatment selection. | Validation of biomarkers in large-scale clinical trials and development of diagnostic tools based on these findings. |
| Immunomodulatory Therapies | Immunomodulatory drugs are showing promise in reducing inflammation and slowing disease progression. | Further development of therapies targeting specific inflammatory pathways and exploring combination therapies to optimize outcomes. |
| Early Detection and Prevention | Research suggests that early intervention can significantly improve outcomes. | Identification of individuals at high risk for developing RA and development of preventative strategies. |
Closing Summary
In conclusion, the diverse types of rheumatoid arthritis highlight the need for personalized care and a deep understanding of the individual patient’s experience. We’ve explored the complexities of the disease, from its varied presentations to the challenges of living with it. Ultimately, this journey underscores the importance of ongoing research, support systems, and a proactive approach to managing this condition.
The future promises innovative treatments and a more comprehensive understanding of these specific types of rheumatoid arthritis, leading to better outcomes for those affected.








![How to Prevent Mosquito Bites [Infographic] - Best Infographics How to prevent mosquito bites](https://healthytipp.com/wp-content/uploads/2025/06/MosquitoBitePreventionTravelers_5081024_1-791x600-1-1.jpg)