Foods to avoid with UTI can significantly impact your recovery. Understanding which foods might worsen your symptoms is key to managing this common infection effectively. This guide explores the relationship between diet and UTIs, providing insights into specific foods to limit or avoid, along with strategies for hydration and balanced meal plans. We’ll delve into the science behind these dietary recommendations and explore how to personalize your approach for optimal recovery.
A urinary tract infection (UTI) is an infection that can affect the kidneys, bladder, and urethra. Dietary modifications can play a crucial role in managing UTI symptoms and preventing complications. The specific foods to avoid with a UTI will vary depending on the type of UTI and individual circumstances. This guide aims to provide a comprehensive overview of dietary strategies for UTI management.
Foods to Avoid During a UTI
Urinary tract infections (UTIs) are common, affecting millions worldwide. While antibiotics are crucial for treating UTIs, dietary modifications can support the healing process and potentially reduce the risk of recurrence. These dietary adjustments focus on reducing irritants and promoting a healthy urinary environment. Understanding the connection between diet and UTIs is key to managing symptoms and preventing future infections.Dietary strategies for UTI management aim to minimize irritants to the urinary tract, optimize hydration, and potentially reduce the growth of bacteria that may contribute to infection.
The specifics of dietary recommendations may vary depending on the type of UTI and individual circumstances.
General Principles of Dietary Modifications
Dietary modifications for UTI management often involve limiting certain foods that may irritate the urinary tract or promote bacterial growth. This approach, however, is not a substitute for medical treatment. It is essential to consult a healthcare professional for proper diagnosis and treatment of UTIs.
- Hydration is paramount. Drinking plenty of water helps flush bacteria out of the urinary tract and promotes healthy urine flow. Aim for 8 glasses of water daily, or more, as advised by your healthcare provider.
- Reducing Irritants. Some foods and drinks can irritate the bladder, making symptoms worse. These foods should be consumed in moderation or avoided altogether if possible.
- Limiting Sugar Intake. High sugar content in certain foods can contribute to the growth of bacteria in the urinary tract. Opt for sugar-free alternatives where possible.
- Choosing a Healthy Diet. A balanced diet rich in fruits, vegetables, and whole grains promotes overall health and supports the immune system’s function.
Types of UTIs and Dietary Considerations
The severity and treatment approach for UTIs can vary based on whether the infection is uncomplicated or complicated.
| Type of UTI | Dietary Considerations |
|---|---|
| Uncomplicated UTI | Generally, uncomplicated UTIs are treated with antibiotics. Dietary modifications are focused on hydration and minimizing irritants. These infections typically affect the lower urinary tract (bladder and urethra). Focus on increasing fluid intake and avoiding overly acidic or spicy foods. Examples include cranberry juice and some highly processed foods. |
| Complicated UTI | Complicated UTIs often involve underlying medical conditions, such as diabetes or kidney stones, or are recurrent infections. Dietary recommendations for complicated UTIs might need to address specific health issues. For instance, managing blood sugar levels is crucial for individuals with diabetes. Dietary modifications are usually part of a comprehensive treatment plan, working in conjunction with prescribed medications and medical procedures. Individuals with underlying conditions should consult with a healthcare professional to determine specific dietary recommendations. |
Specific Foods to Avoid
A urinary tract infection (UTI) can be uncomfortable and disruptive. While antibiotics are often the primary treatment, dietary changes can play a significant role in managing symptoms and potentially preventing future infections. Understanding which foods to limit or avoid can be crucial for optimal recovery and overall urinary health.Foods high in sugar, artificial sweeteners, acidic ingredients, and those that irritate the urinary tract can all negatively impact the healing process and potentially worsen UTI symptoms.
Furthermore, certain foods can contribute to the formation of kidney stones, which can complicate UTI cases. This section dives into the specific dietary considerations to be mindful of during a UTI.
Sugar Content and UTI Risk
High sugar intake can lead to an overgrowth of bacteria in the urinary tract, potentially exacerbating a UTI. Consuming excessive sugar can create an environment favorable for harmful bacteria, impacting the balance of the urinary tract’s natural defenses. For instance, sugary drinks, processed foods, and certain fruits can contribute to this effect.
Artificial Sweeteners and UTI Development
Artificial sweeteners, while often marketed as sugar-free alternatives, can have unforeseen effects on urinary health. Some studies suggest a potential link between artificial sweetener consumption and increased UTI risk. However, more research is needed to fully understand the exact mechanisms and extent of this relationship.
Acidic Foods and UTI Symptoms
Acidic foods can sometimes irritate the urinary tract, potentially exacerbating UTI symptoms. Foods with high acidity can affect the pH balance of urine, creating an environment potentially more conducive to bacterial growth. While avoiding all acidic foods is not necessarily required, moderation and awareness of individual sensitivities are key.
Foods Irritating the Urinary Tract
Certain foods and drinks can irritate the urinary tract, which can worsen symptoms of a UTI. These include highly spiced foods, certain types of alcohol, and overly acidic beverages. Identifying and avoiding such irritants can help ease discomfort and promote healing.
Foods to Avoid Categorized by Food Type
- Fruits: Highly acidic fruits like cranberries (despite their reputation for UTI prevention) can exacerbate symptoms in some individuals. Overconsumption of sugary fruits can also contribute to bacterial overgrowth.
- Vegetables: Certain vegetables, particularly those with high acidity, might trigger irritation. Moderation is crucial.
- Meats: Processed meats often contain high levels of sodium, which can increase fluid retention and potentially worsen UTI symptoms. Red meats, in some cases, can contribute to acidity.
- Dairy: Dairy products, especially those with high fat content, can impact hydration levels, which can influence UTI severity.
Foods to Avoid – Detailed Table
| Food Category | Specific Foods | Reason for Limitation |
|---|---|---|
| Fruits | Cranberries (in excess), highly acidic fruits | Can irritate the urinary tract and potentially worsen symptoms in some individuals. |
| Vegetables | Certain acidic vegetables | Potential to irritate the urinary tract, affecting pH balance. |
| Meats | Processed meats, overly seasoned meats | High sodium content can increase fluid retention and worsen symptoms. |
| Processed Foods | Sugary snacks, sugary drinks | High sugar content can create an environment favorable for bacteria overgrowth. |
| Dairy | High-fat dairy products | May impact hydration, which can influence UTI severity. |
Oxalate-Rich Foods and Kidney Stones
Foods high in oxalate, such as spinach, rhubarb, and beets, can contribute to the formation of kidney stones. Kidney stones can sometimes complicate UTI cases. Individuals prone to kidney stones should be mindful of oxalate intake.
Processed Foods and UTI Risk
Different types of processed foods can have varying impacts on UTI risk. Sugary processed foods can contribute to bacterial overgrowth, whereas processed meats can increase sodium intake and potentially worsen symptoms. Understanding the specific ingredients and their impact is essential.
Foods to Limit

Sometimes, completely avoiding certain foods isn’t necessary for managing a urinary tract infection (UTI). Instead, limiting certain foods can help prevent bacterial growth and promote faster healing. Moderation is key, as some foods can be more conducive to bacteria growth than others. This approach allows you to enjoy a balanced diet while supporting your body’s natural healing process.Limiting certain foods is crucial during a UTI, not only to prevent further bacterial growth but also to promote a healthier urinary tract environment.
This approach can significantly contribute to faster healing and a more comfortable experience during the infection. By understanding which foods to limit and why, you can make informed dietary choices that actively support your body’s recovery.
Foods High in Sugar and Refined Carbs
Consuming excessive amounts of sugary and refined carbohydrates can potentially promote bacterial growth in the urinary tract. Sugary drinks, candy, and highly processed foods often contain simple sugars that can fuel the growth of bacteria. This is important to understand, as these foods can directly impact the bacterial environment within the urinary tract.
- Sugary drinks (soda, juice): Limit consumption to avoid excessive sugar intake, which can contribute to bacterial growth in the urinary tract.
- Candy and sweets: Limit intake, as they contain simple sugars that may encourage bacterial growth.
- White bread, pastries, and other refined carbohydrates: Limit these foods, as they can potentially promote bacterial growth in the urinary tract.
Foods High in Oxalate
Certain foods are naturally high in oxalates, a compound that can sometimes contribute to kidney stone formation. While kidney stones are not directly linked to UTIs, it is prudent to limit foods high in oxalates to support overall urinary health during an infection.
Speaking of things to steer clear of, certain foods can really irritate a urinary tract infection (UTI). Things like sugary drinks and processed foods can often make the discomfort worse. Meanwhile, understanding the latest advancements in continuous glucose monitoring (CGM) technology is important too, like the recent FDA clearance for the Eversense 365 CGM eversense 365 cgm fda clearance.
Ultimately, paying attention to what you eat can significantly impact your overall well-being, including how you manage a UTI.
| Food | Suggested Portion Size |
|---|---|
| Spinach | 1/2 cup cooked |
| Beets | 1/2 cup cooked |
| Rhubarb | 1/2 cup cooked |
| Chocolate | A small square (15-20g) |
| Nuts and seeds | 1/4 cup |
High-oxalate foods may increase the risk of kidney stones. Reducing intake helps maintain a healthy urinary tract environment.
Foods High in Purines
Purines are compounds that can be broken down into uric acid, which may contribute to urinary tract issues in some individuals. Limiting purine-rich foods can help maintain a balanced urinary environment.
- Organ meats (liver, kidney): Limit intake as they are very high in purines.
- Seafood (herring, sardines, anchovies): Limit consumption, as these foods contain substantial amounts of purines.
- Red meat: Limit portions, as red meat is a significant source of purines.
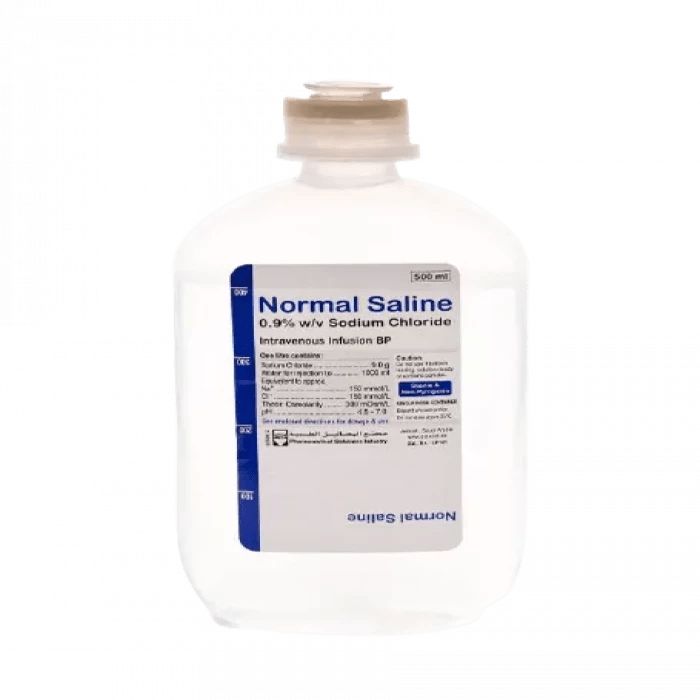
Hydration and Fluid Intake: Foods To Avoid With Uti
Staying hydrated is essential for overall health, and it plays a crucial role in preventing and managing urinary tract infections (UTIs). Proper hydration helps flush out bacteria from the urinary tract, reducing the risk of infection. This is especially important during a UTI to support the body’s natural healing process.Maintaining adequate fluid intake is a vital component of UTI management.
The right types of fluids and an appropriate daily intake can significantly contribute to preventing recurrence and promoting faster recovery. Conversely, certain fluids can exacerbate symptoms or interfere with the treatment process. This section provides guidance on appropriate hydration strategies for managing UTIs.
Importance of Hydration in UTI Prevention and Management
Adequate hydration is key to preventing UTIs. When you drink enough fluids, you dilute urine, which makes it harder for bacteria to multiply and cause infection. Proper hydration also helps to flush bacteria out of the urinary tract. This is particularly important in managing a UTI as it supports the body’s natural healing mechanisms.
Types of Fluids to Drink and Avoid During a UTI
The focus should be on fluids that support the body’s natural flushing action and do not contain substances that could irritate the urinary tract.
- Recommended Fluids: Water is the best choice. Other good options include unsweetened herbal teas (like chamomile or ginger), diluted fruit juices (like apple or cranberry), and clear broths. These fluids support hydration without irritating the urinary tract.
- Fluids to Avoid: Avoid sugary drinks like soda, juice (especially those high in citric acid), and alcoholic beverages. These can irritate the urinary tract and potentially hinder the healing process. Coffee and tea in large quantities may also have a diuretic effect, but in moderation they are not harmful.
Recommended Daily Fluid Intake for Individuals with UTIs
Individual fluid needs vary based on factors like activity level, climate, and overall health. However, a general guideline for individuals with UTIs is to aim for at least 8-10 glasses of fluids daily.
| Individual | Recommended Daily Fluid Intake (approx.) |
|---|---|
| Average Adult (mild to moderate activity) | 8-10 glasses |
| Active Individuals | 10-12 glasses |
| Individuals in Hot Climates | More than 10 glasses |
Importance of Cranberry Juice and Safe Incorporation
Cranberry juice is often recommended for UTI prevention and management due to its purported ability to prevent bacteria from adhering to the urinary tract walls. However, it’s crucial to consume it in moderation and consider individual tolerance.
- Benefits: Cranberry juice’s active compounds may help prevent bacteria from adhering to the walls of the urinary tract, reducing the risk of infection.
- Safety Considerations: Excessive cranberry juice consumption can cause digestive issues, such as diarrhea. Always dilute cranberry juice with water to minimize potential irritation.
- Incorporating Cranberry Juice Safely: Start with a small amount (e.g., 1/4 cup) of diluted cranberry juice and gradually increase it if tolerated. If you experience digestive upset, reduce the amount or stop altogether.
Creating a Personalized Hydration Plan
A personalized hydration plan considers individual needs and preferences. This approach helps ensure adequate fluid intake without overdoing it.
- Monitoring Intake: Track your fluid intake using a journal or app to ensure you’re meeting your goals.
- Listening to Your Body: Pay attention to your thirst cues and adjust your intake accordingly.
- Incorporating Fluids into Meals: Include fluids with meals and snacks to maintain hydration throughout the day.
- Adjusting for Activity: Increase your fluid intake during periods of increased activity or in hot weather.
Dietary Recommendations and Sample Meal Plans
A crucial aspect of managing a urinary tract infection (UTI) is following a diet that supports your body’s natural healing process. A balanced diet, with careful consideration of foods to avoid and those to include, can significantly impact the duration and severity of your symptoms. Proper nutrition plays a vital role in boosting your immune system and promoting overall well-being during this time.Dietary choices during a UTI can influence the infection’s progress and recovery time.
By incorporating specific foods and avoiding others, you can contribute to a more comfortable and efficient healing process. This section provides sample meal plans, emphasizing the importance of portion control and balanced nutrition for optimal recovery.
Importance of Portion Control
Maintaining a healthy weight and avoiding excessive caloric intake is important for overall health, and it’s especially relevant during UTI management. Overeating can strain your body’s resources, potentially hindering its ability to fight off infection. Careful portion control ensures that your body has the energy it needs without overwhelming its systems. Moderation in food intake is crucial for proper digestion and nutrient absorption.
Avoiding certain foods can significantly impact your overall health, especially when dealing with a urinary tract infection (UTI). Things like sugary drinks and processed foods can irritate the urinary tract, hindering your body’s natural healing process. Taking simple steps to improve your overall health, such as a balanced diet and regular exercise, can be crucial in boosting your well-being and potentially increasing your life expectancy.
Check out simple steps to increase your life expectancy for more ideas. Ultimately, focusing on a diet low in processed foods and high in fruits and vegetables can help prevent UTIs and support your overall health.
Importance of Balanced Meals
A balanced meal plan provides your body with the essential nutrients it needs to function optimally, particularly during an infection. It includes a variety of foods from all food groups, ensuring you receive adequate vitamins, minerals, and antioxidants, which play a vital role in supporting the immune system. Such a balanced diet is important for supporting your body’s natural healing mechanisms and preventing nutrient deficiencies.
Importance of Following a Consistent Dietary Plan
Maintaining a consistent dietary plan for UTI prevention and management ensures your body receives a steady supply of essential nutrients. This consistency helps your body maintain optimal metabolic function, contributing to faster recovery. A consistent dietary plan reduces the risk of nutrient deficiencies and provides the building blocks your body needs to repair and restore itself. A consistent diet helps your immune system function optimally, contributing to a quicker recovery.
3-Day Sample Meal Plan
This table provides a 3-day sample meal plan designed for UTI prevention and management. It emphasizes foods to avoid and those to include, along with portion control and balanced meals. This sample plan is a guideline and can be adjusted based on individual dietary needs and preferences.
| Day | Breakfast | Lunch | Dinner |
|---|---|---|---|
| Day 1 | Oatmeal with berries and a sprinkle of nuts (avoiding sugary cereals). A glass of unsweetened almond milk. |
Grilled chicken salad with mixed greens, cucumber, and bell peppers (avoiding processed meats). A side of steamed broccoli. |
Baked salmon with roasted vegetables (avoiding fried foods). A small portion of quinoa. |
| Day 2 | Scrambled eggs with spinach and whole-wheat toast. A glass of water. |
Lentil soup with whole-grain bread. A side salad. |
Lean turkey meatballs with zucchini noodles. A small portion of brown rice. |
| Day 3 | Greek yogurt with fruit and a drizzle of honey (avoiding excessive sugar). A glass of water. |
Tuna salad sandwich on whole-wheat bread with a side of mixed greens. A piece of fruit. |
Chicken stir-fry with plenty of vegetables (avoiding excessive sodium). A small bowl of brown rice. |
Foods to Encourage
Fueling your body with the right nutrients is crucial for a speedy UTI recovery and overall well-being. Choosing foods that support a healthy urinary tract and immune system can significantly aid in your healing process. These foods work in harmony with your body’s natural defenses to fight infection and promote a faster return to optimal health.Supporting your urinary tract and immune system is more than just avoiding certain foods; it’s about proactively nourishing your body with beneficial nutrients.
By incorporating specific foods and drinks, you can create an environment that discourages bacterial growth and strengthens your body’s defenses against infection. This proactive approach will not only help you recover from a UTI faster but also maintain long-term urinary tract health.
Probiotics and Prebiotics
Probiotics and prebiotics are essential components of a healthy gut microbiome. A balanced gut microbiome plays a crucial role in overall health, including urinary tract health. Probiotics are live microorganisms, such as bacteria and yeasts, that offer numerous health benefits, including improved digestion and a strengthened immune system. Prebiotics are non-digestible food ingredients that selectively stimulate the growth and activity of beneficial bacteria in the gut, further supporting the beneficial gut microbiome.Incorporating fermented foods, such as yogurt, kefir, sauerkraut, and kimchi, provides a source of probiotics.
These foods contain live bacteria that help restore and maintain a healthy gut balance. Similarly, prebiotics can be found in foods like bananas, onions, garlic, asparagus, and leeks. These foods serve as a food source for the beneficial bacteria, fostering a healthy gut microbiome. A healthy gut microbiome is directly linked to a healthier urinary tract and immune system.
Nutrients for UTI Recovery
A diet rich in vitamins and minerals plays a vital role in supporting the body’s natural defenses against infection. Many vitamins and minerals contribute to immune function, promoting a faster recovery from a UTI. These nutrients work together to support the body’s overall health and well-being.
- Vitamin C: A potent antioxidant, vitamin C strengthens the immune system and aids in the production of collagen, which is crucial for tissue repair. Citrus fruits, berries, and bell peppers are excellent sources. A daily intake of vitamin C can significantly support immune function and contribute to faster recovery.
- Vitamin D: Vitamin D is known for its immune-boosting properties and plays a role in maintaining healthy gut bacteria. Fatty fish, eggs, and fortified foods are good sources. Sufficient vitamin D levels are essential for overall immune function, aiding in the fight against infection.
- Zinc: Zinc is crucial for immune function and wound healing. Oysters, beef, and pumpkin seeds are rich in zinc. Zinc supports the body’s ability to fight infection and promote healing.
- Potassium: Potassium is an essential mineral for overall health, including maintaining healthy fluid balance and supporting kidney function. Bananas, sweet potatoes, and spinach are good sources. Potassium helps regulate fluid balance and supports the kidneys’ ability to filter waste, promoting urinary tract health.
Hydration
Maintaining adequate hydration is essential for flushing out bacteria and supporting overall urinary tract health. Water is crucial for a healthy urinary system.
- Water: Water is the best choice for hydration, supporting the natural cleansing process of the urinary tract. Drinking plenty of water throughout the day helps to dilute urine and flush out bacteria.
- Electrolyte-rich drinks: Electrolyte drinks, such as coconut water or sports drinks, can help replenish lost electrolytes during recovery. These drinks provide essential minerals and aid in maintaining proper hydration.
Potential Interactions with Medications
Taking medications for a urinary tract infection (UTI) is crucial, but certain foods can interact with these drugs, affecting their effectiveness or causing side effects. Understanding these potential interactions is vital for managing your UTI and ensuring your treatment is as safe and effective as possible.Dietary choices can influence how your body absorbs and utilizes medications. It’s important to be mindful of these potential interactions and to always consult your doctor before making significant dietary changes while taking UTI medications.
This proactive approach will help ensure that your treatment plan is optimized for your specific needs and circumstances.
Medication Absorption and Food Interactions, Foods to avoid with uti
Dietary choices can significantly impact how your body absorbs medications. Certain foods can bind to medications, reducing their absorption into the bloodstream. Conversely, other foods might enhance absorption, potentially leading to increased side effects.
Trying to manage a urinary tract infection (UTI)? One thing to consider is the difference between dried and fresh fruits. While fresh fruit is generally a healthy choice, some dried fruits, like raisins or dates, can be high in sugar, which can potentially irritate the bladder. This makes them something to think about avoiding if you’re battling a UTI.
Understanding the nutritional differences between these options is key, especially when comparing the sugar content and how it affects your body. Check out this comparison of dried fruit vs fresh fruit to learn more about the potential impact on your health. Ultimately, focusing on a balanced diet, including plenty of water, is important for recovery and preventing future UTIs.
- Some antibiotics, for instance, are better absorbed on an empty stomach. Eating a meal containing high-fat content might reduce the medication’s absorption rate, making it less effective.
- Calcium-rich foods, such as dairy products, can interfere with the absorption of certain antibiotics. This is because calcium competes with the medication for absorption sites in the gut.
- Grapefruit juice can interact with many medications, including some UTI treatments. It can inhibit the enzymes responsible for breaking down medications, leading to higher concentrations in the bloodstream and potentially causing adverse reactions.
Importance of Consulting a Healthcare Professional
Before making any substantial dietary changes while taking UTI medications, it’s essential to consult your doctor or pharmacist. They can assess your individual needs and provide personalized recommendations.
- A healthcare professional can advise you on foods to avoid or limit while taking specific medications, tailoring their advice to your unique situation.
- They can also advise on appropriate food timing relative to medication intake, maximizing absorption and effectiveness.
- Furthermore, your doctor can identify potential interactions between medications and specific foods relevant to your individual health conditions, allergies, or any other relevant medical history.
Maintaining a Consistent Medication Schedule
Adhering to a consistent medication schedule is crucial for UTI treatment. This regularity ensures a steady level of medication in the body, maximizing its effectiveness. Dietary changes can impact this schedule.
- Consistent medication intake is key for effective UTI treatment. This is because a consistent dose of the medication at regular intervals helps maintain an appropriate level of the active substance in the bloodstream, which is crucial for successful treatment.
- If you experience any changes in your appetite or dietary habits, you should discuss these with your doctor or pharmacist to adjust the timing of your medication or food intake to ensure the medication is effectively absorbed.
- For example, if you experience nausea or vomiting, you might need to adjust your medication timing or dosage in consultation with a healthcare professional to prevent any gaps in treatment and optimize the medication’s effectiveness.
Cultural and Dietary Considerations

A UTI diet plan should be tailored to individual needs, and this includes respecting cultural and dietary preferences. Understanding how cultural practices shape food choices is crucial for successful UTI management. Different cultures have unique dietary traditions, and these traditions can impact the foods we eat and how we handle illness.Cultural norms often dictate what foods are considered acceptable or taboo, and these norms can significantly influence dietary changes during illness.
Furthermore, religious beliefs and cultural traditions surrounding food can play a role in how people approach dietary modifications. Respecting these aspects is vital to ensure the dietary plan is both effective and sustainable.
Cultural Influences on Food Choices
Cultural traditions heavily influence food choices. For example, some cultures may favor high-sodium foods, while others prioritize fresh produce. Religious dietary laws, such as those followed by Muslims or Jews, can further restrict food choices. Understanding these nuances is essential when designing a UTI diet.
Adapting Cultural Practices for UTI Management
A UTI diet plan should be flexible and adaptable to different cultural practices. Instead of completely eliminating foods, explore ways to substitute or modify them. For example, if a particular dish is high in sodium, find lower-sodium alternatives. This allows for the maintenance of cultural traditions while managing the UTI.
Examples of Cultural Dietary Adjustments During Illness
In some cultures, a common practice during illness involves consuming warm, comforting soups or broths. This aligns with the principles of a UTI diet, as these soups often contain hydrating elements and can support overall recovery. In other cultures, specific herbs or spices might be used to soothe symptoms or promote healing. These cultural approaches can be incorporated into a UTI diet plan.
Incorporating Dietary Modifications with Respect for Beliefs
When creating a UTI diet plan, prioritize open communication with the individual. Engage in a discussion about their cultural dietary preferences and beliefs. Work together to find ways to incorporate healthy dietary modifications that respect their beliefs and traditions. A collaborative approach ensures the plan is personalized and sustainable. For instance, if someone follows a vegetarian diet, the plan should incorporate plenty of plant-based protein sources.
Similarly, if someone has religious restrictions, the plan should comply with those restrictions. This involves consulting with registered dietitians who have experience in cultural dietary needs and are knowledgeable about dietary restrictions.
End of Discussion
In conclusion, managing a UTI involves a multi-faceted approach, and dietary considerations are an essential part of the process. By understanding the specific foods to avoid and the importance of proper hydration, you can actively support your body’s healing process. This guide offers practical strategies and insights to help you navigate dietary changes during a UTI, ensuring a more comfortable and effective recovery.
Remember, consulting with a healthcare professional is crucial for personalized advice and treatment.