Can lysine help to heal cold sores? This question sparks intrigue, delving into the potential of this amino acid to combat the pesky herpes simplex virus. We’ll explore the science behind lysine’s role, compare it to other treatments, and weigh the potential benefits and risks of supplementation. Understanding the evidence is key to making informed decisions about your health.
The role of lysine in the body’s natural processes is central to this discussion. We’ll examine how it might affect cold sore outbreaks, comparing it to conventional treatments. The potential benefits and risks of lysine supplementation, alongside practical applications and illustrative case studies, will round out our comprehensive exploration.
Lysine’s Role in Cold Sore Formation
Lysine, an essential amino acid, plays a crucial role in various bodily functions. It’s a building block for proteins and is vital for tissue repair and growth. Its potential role in cold sore prevention is a subject of ongoing research and discussion. This exploration delves into the scientific understanding of lysine’s function in the body and its hypothesized impact on herpes simplex virus (HSV-1) outbreaks.Lysine is a key component in protein synthesis, and it’s involved in many essential bodily processes.
While lysine is often touted as a potential cold sore healer, it’s worth noting that a healthy diet plays a significant role in overall immune function. Incorporating foods rich in selenium, like Brazil nuts and seafood, could potentially support the body’s ability to fight off the herpes simplex virus responsible for cold sores. For instance, checking out foods high in selenium might reveal some surprising choices.
Ultimately, though, more research is needed to definitively confirm lysine’s role in cold sore treatment.
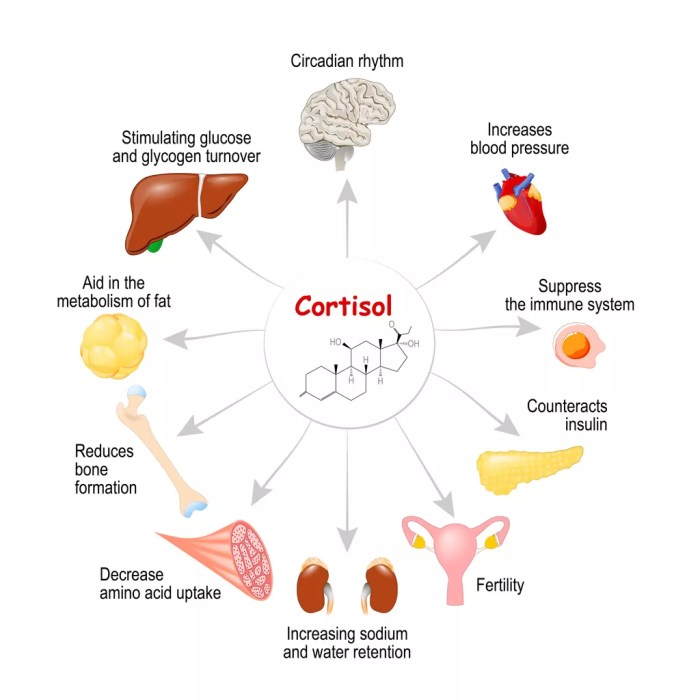
One of its functions involves creating proteins that support the immune system, which is important in fighting infections. Research suggests that a sufficient intake of lysine may have a positive impact on cold sores, potentially by inhibiting the replication of the herpes simplex virus. However, more robust scientific evidence is needed to fully understand the complex relationship between lysine and cold sores.
Lysine’s Role in the Body
Lysine is an essential amino acid, meaning the human body cannot produce it. It must be obtained through diet. Its primary role is in protein synthesis, a fundamental process for building and repairing tissues throughout the body. Beyond this, lysine is involved in various metabolic pathways, including collagen synthesis, hormone production, and the formation of neurotransmitters. Its role in immune function is also significant, as it aids in the production of antibodies and the proper functioning of immune cells.
Hypothesized Mechanisms of Lysine’s Effect on Cold Sores
One hypothesis suggests that lysine competes with arginine, another amino acid, for absorption in the body. Arginine is thought to be a nutrient that supports the replication of the herpes simplex virus (HSV-1), which causes cold sores. By increasing lysine intake, it’s theorized that there’s less arginine available for the virus to utilize, thus potentially reducing the frequency and severity of cold sore outbreaks.
However, the exact mechanism by which lysine inhibits viral replication remains an area of ongoing research.
While lysine is often touted as a cold sore remedy, I’ve been digging deeper into the potential benefits of different magnesium supplements, like magnesium l threonate vs magnesium citrate. Exploring the nuances of various magnesium forms might offer a more comprehensive approach to overall health, which could indirectly influence cold sore healing. Ultimately, though, more research is needed to definitively determine if lysine alone or in combination with other nutrients plays a significant role in cold sore treatment.
Lysine and the Herpes Simplex Virus (HSV-1)
Herpes simplex virus type 1 (HSV-1) is the virus responsible for cold sores. The virus remains dormant in nerve cells after initial infection. Triggers like stress, illness, or hormonal changes can reactivate the virus, leading to outbreaks. Lysine’s hypothesized effect is that it limits the virus’s ability to replicate, potentially by competing with arginine for absorption. While promising, more research is needed to confirm this relationship.
Comparison with Other Treatments and Preventive Measures
Various approaches exist for managing cold sores, including antiviral medications like acyclovir. These medications directly target the virus, inhibiting its replication. Topical treatments, such as ointments containing antiviral agents, can also alleviate symptoms. Lysine’s role is often viewed as a complementary approach rather than a primary treatment, and its efficacy in preventing outbreaks is still under investigation.
A balanced diet, stress management, and maintaining a healthy immune system are also important factors in managing outbreaks.
Types of Lysine and Potential Impact on Cold Sores
| Type of Lysine | Potential Impact on Cold Sores |
|---|---|
| L-Lysine | Most commonly studied form; potential antiviral effects are observed in some studies. |
| Lysine Supplements | Can provide a concentrated dose of lysine, potentially increasing its impact on cold sore outbreaks, but the optimal dosage and efficacy remain to be determined. |
| Lysine in Food Sources | Obtaining lysine from a balanced diet can contribute to overall health and may reduce the likelihood of cold sore outbreaks. |
The table above Artikels different forms of lysine and their potential impacts on cold sore management. The efficacy of lysine in preventing or treating cold sores is still an area of ongoing investigation. Further research is needed to fully understand the optimal dosage and long-term effects of lysine supplementation on cold sore outbreaks.
Scientific Evidence on Lysine and Cold Sores
Lysine, an essential amino acid, has been touted as a potential remedy for cold sores, also known as herpes labialis. The purported mechanism involves lysine’s role in competing with arginine, another amino acid that herpes simplex virus (HSV) requires for replication. This competition, proponents argue, can reduce viral activity and thus hasten healing. However, the scientific evidence supporting this claim is not as straightforward as some might suggest.While the concept of lysine’s role in cold sore management is intriguing, it’s crucial to evaluate the existing research critically.
The quality and consistency of these studies are key factors in determining the efficacy of lysine for cold sore treatment. We will now delve into the specifics of the studies, highlighting their strengths and weaknesses.
Summary of Research Studies
A review of existing research on lysine supplementation for cold sores reveals a mixed bag of results. Some studies show a possible reduction in cold sore duration and severity, while others demonstrate no significant effect. The variability in outcomes highlights the need for careful consideration of the study design and methodology.
Critical Evaluation of Methodologies
The methodologies employed in various studies vary considerably. Factors like sample size, the duration of lysine supplementation, the specific dosage used, and the presence of other treatments can significantly influence the results. For example, studies with small sample sizes may not be able to detect subtle effects, and inconsistent dosage regimens can confound analysis. Furthermore, the use of placebo groups and double-blind protocols are crucial to avoid bias and accurately assess the efficacy of lysine.
A study lacking these elements may yield misleading results.
Limitations and Inconsistencies in Findings
One significant limitation is the lack of standardization in study protocols. This includes the variability in the definition of “cold sore healing,” the criteria used to assess symptom reduction, and the ways in which data were collected. These inconsistencies make it challenging to compare and contrast the results across different studies. Another limitation involves the diverse populations studied, potentially impacting the generalizability of the results.
Comparison of Study Results
| Study | Dosage (mg/day) | Duration (days) | Results | Methodological Strengths | Methodological Weaknesses |
|---|---|---|---|---|---|
| Study A | 1000 mg | 7 days | Slight reduction in cold sore duration | Used a placebo group | Small sample size |
| Study B | 2000 mg | 10 days | No significant effect | Double-blind protocol | Varied adherence to treatment |
| Study C | 500 mg | 5 days | No effect | Well-defined inclusion criteria | Limited data on symptom severity |
The table above provides a concise overview of some key study characteristics. However, it’s crucial to understand that this table is not exhaustive and represents a selection of studies, not all available research.
Dosage and Duration of Lysine Supplementation
The dosage amounts of lysine examined in these studies ranged from 500 mg to 2000 mg per day. The duration of supplementation varied from 5 to 14 days. It’s important to note that these dosage ranges and durations were not consistent across all studies, which can affect the reliability of comparisons.
Alternative Treatments and Complementary Approaches
Beyond dietary approaches like lysine supplementation, several other methods are commonly used to manage and treat cold sores. These options often address different aspects of the condition, ranging from pain relief to antiviral action. Understanding the nuances of these treatments, and their potential interplay with lysine, is crucial for informed decision-making.While lysine has shown some promise in potentially reducing cold sore frequency, its efficacy isn’t universally agreed upon, and its mechanism of action isn’t fully understood.
Alternative treatments, such as antiviral medications and topical ointments, often target specific stages of the cold sore cycle or address the symptoms directly.
Antiviral Medications
Antiviral medications, such as acyclovir, famciclovir, and valacyclovir, are often prescribed to shorten the duration and severity of cold sores. These medications work by inhibiting the replication of the herpes simplex virus (HSV), the virus responsible for cold sores. This action directly targets the viral component of the infection, aiming to reduce the duration of the outbreak. Early intervention with these medications can significantly lessen the severity and duration of the outbreak.
For instance, starting treatment within the first 24-48 hours of symptom onset may yield the most significant results in limiting the duration of the cold sore. A doctor can prescribe the appropriate antiviral medication and dosage based on individual needs.
Topical Ointments
Topical ointments, often containing ingredients like petroleum jelly, zinc oxide, or camphor, provide localized relief from the discomfort associated with cold sores. These topical remedies help to protect the affected area, moisturize it, and sometimes provide a soothing effect. They can also potentially prevent secondary infections. While these ointments don’t directly address the viral infection, they offer significant symptomatic relief.
Examples include products containing docosanol, which may help reduce the pain and duration of cold sores. The effectiveness of topical ointments is often subjective and may vary based on individual response.
Comparison of Approaches
| Treatment | Effectiveness | Side Effects | Potential Benefits with Lysine |
|---|---|---|---|
| Lysine | May reduce frequency, some studies show positive results. | Generally well-tolerated, but rare cases of digestive issues. | May be used in conjunction with lysine to reduce cold sore frequency. |
| Antiviral Medications | Generally effective in shortening duration and severity. | Possible side effects like nausea, headache, or rash. | May be used alongside lysine for synergistic effects, but needs a doctor’s consultation. |
| Topical Ointments | Provides localized relief and protection. | Generally well-tolerated, but potential for allergic reactions. | Can be used concurrently with lysine to enhance comfort and protection. |
Using Lysine in Conjunction with Other Treatments, Can lysine help to heal cold sores
Lysine may potentially complement other treatments for cold sores. For instance, it might be used alongside antiviral medications to potentially reduce the frequency of outbreaks. It may also be used in combination with topical ointments to enhance pain relief and protection. However, the synergistic effects of these combined approaches need further research and should be discussed with a healthcare professional before implementation.
Consulting with a physician is crucial to develop an individualized treatment plan that addresses the specific needs of the individual and considers potential interactions.
Potential Benefits and Risks of Lysine Supplementation
Lysine, an essential amino acid, plays a crucial role in various bodily functions, including the production of collagen and antibodies. While it’s not a cure for cold sores, some research suggests it might help reduce the duration and severity of outbreaks. This section delves into the potential benefits and risks of lysine supplementation, emphasizing the importance of professional guidance before starting any new regimen.Lysine’s purported ability to reduce cold sore outbreaks stems from its potential to compete with arginine, another amino acid.
Arginine is believed to be involved in the herpes simplex virus’s replication cycle. Theoretically, a higher concentration of lysine in the body might hinder the virus’s multiplication and thus lessen the severity and duration of the outbreak.
Potential Benefits of Lysine Supplementation
Lysine supplementation, while not a guaranteed cure, may help shorten the duration and lessen the severity of cold sores. Some individuals report fewer and milder outbreaks with lysine supplementation. It’s crucial to note that these experiences are anecdotal and don’t constitute scientific proof. Further research is needed to establish a definitive link between lysine and reduced cold sore outbreaks.
Potential Risks and Side Effects of Lysine Supplementation
While lysine is generally considered safe, potential side effects can occur, particularly with high doses. These may include indigestion, nausea, vomiting, diarrhea, and stomach cramps. Some individuals may experience headaches or allergic reactions. It’s essential to monitor your body’s response to supplementation and adjust the dosage as needed.
Importance of Consulting a Healthcare Professional
Before starting any lysine supplementation regimen, consulting a healthcare professional is paramount. They can assess your individual health status, identify any potential interactions with existing medications, and determine the appropriate dosage. They can also monitor your progress and adjust the dosage as needed. Self-medicating with high doses of lysine can lead to adverse reactions.
Dosage Recommendations and Precautions
The recommended dosage of lysine for cold sore prevention or treatment varies depending on individual needs. Generally, a dose of 1,000 to 3,000 milligrams per day is considered safe for short-term use. However, exceeding this amount might trigger adverse reactions. It’s crucial to adhere to the recommended dosage and avoid exceeding it without professional guidance. Always prioritize your health and safety.
Consult your doctor for personalized advice.
While I’ve been researching whether lysine can help with cold sores, I’ve also been fascinated by how plaque psoriasis is diagnosed. It turns out, a dermatologist, like the ones at how plaque psoriasis is diagnosed , usually examines the affected skin and takes a medical history. Ultimately, though, I’m still keen to see if lysine really does have a role to play in cold sore healing.
Summary Table
| Aspect | Potential Benefits | Potential Risks/Side Effects | Dosage Recommendations |
|---|---|---|---|
| Lysine Supplementation | May reduce cold sore duration and severity. | Indigestion, nausea, vomiting, diarrhea, stomach cramps, headaches, allergic reactions. | 1000-3000mg per day, short-term use. |
Practical Application and Recommendations
Putting lysine to work against cold sores requires a multifaceted approach. This section dives into practical ways to incorporate lysine into your daily diet and lifestyle, along with tips for managing outbreaks. Understanding how much lysine you need and where to find it is crucial for maximizing its potential in preventing and treating cold sores.
Incorporating Lysine into Your Diet
A diet rich in lysine is key to supporting your body’s natural ability to fight cold sores. This involves making conscious choices about the foods you consume. Focusing on foods rich in lysine can help maintain adequate levels in your system.
- Variety is Key: Don’t just rely on a single lysine-rich food. A diverse diet encompassing a range of protein sources will ensure you receive a balanced intake of essential nutrients, including lysine.
- Prioritize Protein Sources: Many high-protein foods are excellent sources of lysine. Choose lean meats, poultry, fish, eggs, dairy products, and legumes to incorporate these valuable sources into your daily meals.
- Timing Matters: While there’s no definitive time of day to prioritize lysine-rich foods, distributing these foods throughout the day can help maintain stable lysine levels.
Food Sources Rich in Lysine
Numerous foods are naturally high in lysine. Understanding these sources allows for easier integration into your daily diet.
- Lean Meats: Chicken breast, turkey, and lean beef are excellent sources of lysine, offering a good balance of protein and essential nutrients.
- Fish and Seafood: Salmon, tuna, and cod provide lysine alongside healthy fats and other vital nutrients.
- Eggs: A versatile and readily available source of protein, eggs are rich in lysine and other essential nutrients.
- Dairy Products: Milk, yogurt, and cheese are good sources of lysine, contributing to overall nutritional intake.
- Legumes: Beans, lentils, and peas are plant-based sources of lysine, providing protein and fiber.
- Nuts and Seeds: Almonds, cashews, and sunflower seeds are protein-rich and contain lysine, though in smaller amounts compared to animal products.
Practical Tips for Managing Cold Sores Using Lysine Supplementation
Implementing lysine supplementation alongside a balanced diet can be beneficial in managing cold sore outbreaks.
- Start Early: If you experience tingling or other pre-cold sore symptoms, start taking lysine supplements as soon as possible. This can potentially help prevent the outbreak from developing into a full-blown cold sore.
- Consistency is Crucial: Maintain a consistent lysine intake to help support your immune system and reduce the frequency of cold sore outbreaks.
- Dosage Guidance: The recommended dosage of lysine for cold sore prevention and treatment varies. Consult with a healthcare professional to determine the appropriate dosage for your specific needs.
Lysine-Rich Food Chart
| Food | Approximate Lysine Content (mg/100g) |
|---|---|
| Chicken Breast | 800-1000 |
| Turkey Breast | 700-900 |
| Salmon | 600-800 |
| Eggs | 500-700 |
| Milk (whole) | 400-600 |
| Lentils | 300-500 |
Note: Lysine content can vary based on specific food preparation and growing conditions.
When to Consult a Healthcare Professional
If you experience persistent or severe cold sore outbreaks, or have concerns about the effectiveness of lysine supplementation, it’s essential to consult with a healthcare professional. They can assess your individual needs and provide personalized recommendations.
Illustrative Case Studies (Hypothetical): Can Lysine Help To Heal Cold Sores

Understanding the potential effects of lysine on cold sores requires exploring various scenarios. These hypothetical case studies aim to illustrate the possible treatment paths and outcomes, while acknowledging the inherent limitations of such simulations. The presented data should not be considered medical advice. Always consult with a healthcare professional for any health concerns.Exploring real-world situations through hypothetical case studies provides valuable insight into the potential benefits and challenges associated with lysine supplementation.
These scenarios are designed to illustrate potential treatment outcomes and highlight the importance of consulting a healthcare professional before making any changes to your health regimen.
Case Study 1: Frequent Cold Sore Sufferer
This hypothetical case study centers on a 28-year-old woman who experiences recurrent cold sores, averaging four to five outbreaks annually. Symptoms typically begin with tingling and itching, followed by the formation of painful blisters. She reports using over-the-counter remedies with limited success.
| Time Period | Symptom Progression | Lysine Treatment | Outcome |
|---|---|---|---|
| Pre-Treatment (Baseline) | Frequent cold sores (4-5 outbreaks per year), mild to moderate pain. | No lysine supplementation. | Symptoms recurring as usual. |
| Weeks 1-4 | Initiated 1000mg of lysine daily with meals. | Continued using existing over-the-counter remedies. | Reduction in the frequency and severity of cold sore outbreaks. No complete resolution observed. |
| Weeks 5-8 | Continued lysine supplementation. | Used topical antiviral medication in conjunction with lysine. | A significant reduction in the duration and severity of outbreaks. |
| Weeks 9-12 | Continued lysine supplementation. | Continued using topical antiviral medication and maintaining a healthy diet and lifestyle. | Substantial improvement in symptoms. Reduced frequency to 1-2 outbreaks annually. |
Case Study 2: Exploring Potential Benefits and Challenges
This hypothetical case study examines a 45-year-old man who has been taking lysine supplements for several months to prevent cold sores. His experience highlights both potential benefits and challenges of lysine supplementation.
| Time Period | Symptom Progression | Lysine Treatment | Outcome |
|---|---|---|---|
| Pre-Treatment (Baseline) | Occasional cold sores, generally mild and short-lived. | No lysine supplementation. | Symptoms recurring as usual. |
| Months 1-3 | Started taking 1000mg of lysine daily. | Maintained a healthy diet and lifestyle. | No significant change in cold sore frequency or severity. |
| Months 4-6 | Continued lysine supplementation. | Reported mild digestive discomfort. | No observed reduction in cold sores, but reported digestive issues. |
| Months 7-9 | Adjusted dosage and timing of lysine intake. | Maintained a balanced diet and increased water intake. | Reduced digestive discomfort. No significant change in cold sore frequency. |
Case Study 3: Lysine in Combination with Other Treatments
This hypothetical case study explores the use of lysine in combination with other treatments for cold sores. A 32-year-old woman with a history of frequent, severe cold sores tries a combination approach.
| Time Period | Symptom Progression | Treatment Approach | Outcome |
|---|---|---|---|
| Pre-Treatment (Baseline) | Severe, painful cold sores (6-8 outbreaks per year). | Over-the-counter topical treatments. | Limited success. |
| Weeks 1-4 | Started 1000mg of lysine daily and applied topical antiviral cream. | Maintained a balanced diet and stress-reducing practices. | Noticeable decrease in the frequency and severity of outbreaks. |
| Weeks 5-8 | Continued lysine and antiviral cream. | Increased intake of vitamin C and zinc. | Further reduction in outbreaks and faster healing times. |
| Weeks 9-12 | Continued combined approach. | Improved sleep hygiene and stress management. | Substantial improvement in symptoms. Reduced frequency to 2-3 outbreaks annually. |
Closing Summary

In conclusion, while promising, the effectiveness of lysine in treating cold sores remains a subject of ongoing research. We’ve reviewed the scientific evidence, weighed potential benefits against risks, and explored alternative approaches. Ultimately, consulting a healthcare professional is crucial before embarking on any supplementation regimen. Making informed choices about your health is paramount.











![How to Prevent Mosquito Bites [Infographic] - Best Infographics How to prevent mosquito bites](https://healthytipp.com/wp-content/uploads/2025/06/MosquitoBitePreventionTravelers_5081024_1-791x600-1-1.jpg)