What is crohns colitis – What is Crohn’s Colitis? This chronic inflammatory condition affects the digestive tract, causing a range of symptoms and impacting daily life. Understanding the nuances of this complex disease, from its causes and stages to potential complications and treatment options, is crucial for those affected and those seeking to learn more. Let’s explore this condition, shedding light on its intricacies.
Crohn’s Colitis is characterized by inflammation in the digestive tract, often spanning different areas. This inflammation can lead to a wide array of symptoms, from abdominal pain and diarrhea to fatigue and weight loss. The severity and location of the inflammation can vary significantly, making it a challenging condition to manage. This comprehensive guide explores the different aspects of Crohn’s Colitis, providing valuable insights into its various stages, potential causes, diagnosis, treatment options, and the overall management and lifestyle considerations.
Introduction to Crohn’s Colitis: What Is Crohns Colitis
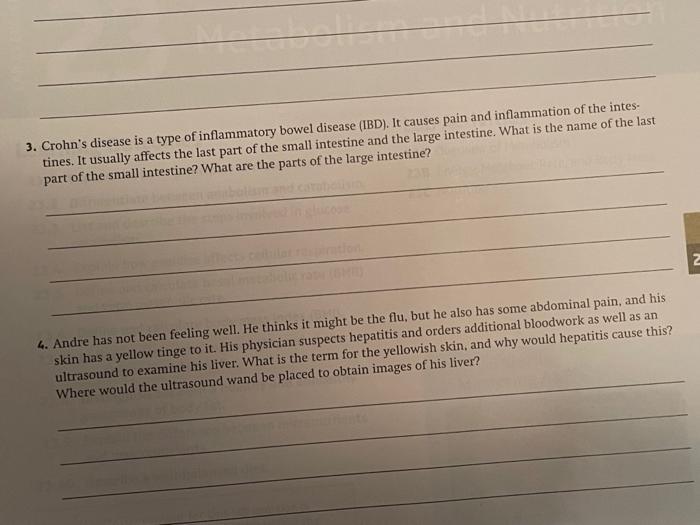
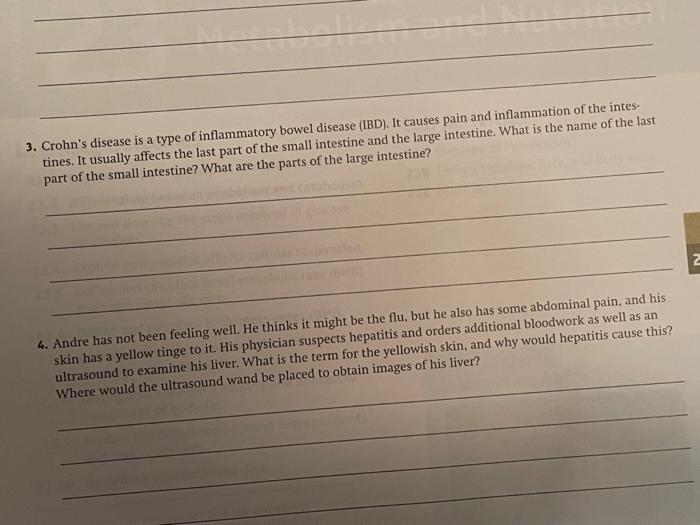
Crohn’s Colitis is a chronic inflammatory bowel disease (IBD) that affects the digestive tract. It’s characterized by inflammation that can occur anywhere along the digestive tract, from the mouth to the anus, although it most commonly affects the end of the small intestine and the beginning of the large intestine. Understanding the specific characteristics of this condition is crucial for accurate diagnosis and effective management.Crohn’s Colitis is distinct from another common IBD, Ulcerative Colitis.
While both involve inflammation in the digestive tract, Ulcerative Colitis primarily affects the colon and rectum, and the inflammation is typically confined to the lining of the colon. Crohn’s, in contrast, can affect any part of the gastrointestinal tract, and the inflammation can extend deeper into the intestinal wall, impacting various layers. This difference in location and depth of inflammation leads to different symptoms and treatment approaches.Common symptoms associated with Crohn’s Colitis include abdominal pain, diarrhea, fever, fatigue, and weight loss.
The severity and frequency of these symptoms can vary significantly from person to person and even over time. These symptoms can significantly impact daily life and require careful management.Crohn’s Colitis severity is categorized into stages. These stages are based on the extent of the disease, the location of inflammation, and the overall impact on the patient’s health.
The stages represent a spectrum of disease activity, from mild to severe, allowing for appropriate medical intervention.
Stages of Crohn’s Colitis Severity
Understanding the different stages of Crohn’s Colitis severity is crucial for appropriate management. This table Artikels the typical symptoms, locations, and complications associated with each stage, providing a clearer picture of the disease’s progression.
| Stage | Typical Symptoms | Locations Affected | Potential Complications |
|---|---|---|---|
| Mild | Occasional abdominal pain, mild diarrhea, minimal weight loss. | Usually limited to a small section of the intestine. | Nutritional deficiencies, anemia, slight fatigue. |
| Moderate | Frequent abdominal pain, significant diarrhea, noticeable weight loss, fatigue. | Inflammation may affect multiple sections of the intestine, or extend deeper into the intestinal wall. | Malnutrition, dehydration, possible need for intravenous fluids, and an increased risk of infections. |
| Severe | Intense abdominal pain, severe diarrhea, significant weight loss, fever, nausea, vomiting, and significant fatigue. | Extensive inflammation across multiple sections of the intestine, potentially involving the entire length of the small or large intestine. | Toxic megacolon (a life-threatening condition where the colon becomes abnormally dilated and cannot function properly), strictures (narrowing of the intestine), fistulas (abnormal connections between organs), and abscesses (collections of pus). |
| Complicated | Severe symptoms from previous stages, along with complications such as fistulas, abscesses, or strictures. | Inflammation is widespread and has led to structural damage or complications. | Surgical intervention may be necessary to address the complications. Long-term management will be required to monitor and treat potential flare-ups. |
Causes and Risk Factors
Understanding the causes and risk factors of Crohn’s Colitis is crucial for both prevention and management. While a definitive cause remains elusive, research points towards a complex interplay of genetic predisposition and environmental triggers. This intricate interplay suggests that individuals with a family history of the disease are more susceptible, but environmental factors can significantly influence the development of the condition.
Potential Causes
Numerous factors are suspected to contribute to the development of Crohn’s Colitis. These include an overactive immune response targeting the gut lining, a disruption in the gut microbiome, and even possible viral or bacterial infections. The precise mechanisms behind these potential causes are still under investigation, but researchers are making progress in understanding the complexities of this inflammatory disease.
Genetic Factors
Genetic predisposition plays a significant role in Crohn’s Colitis. Individuals with a family history of the disease have a substantially higher risk of developing it themselves. Specific genes associated with an increased risk have been identified, highlighting the genetic component in susceptibility. This genetic influence suggests that certain individuals inherit a predisposition to the disease, making them more vulnerable to environmental triggers.
For instance, a sibling or parent with Crohn’s Colitis increases the risk in the individual.
Environmental Factors
Environmental factors also seem to play a crucial role in triggering or exacerbating Crohn’s Colitis. Factors such as diet, stress levels, and exposure to certain infections have been implicated in increasing the risk. Diet, while not a direct cause, can influence the gut microbiome, and stress can weaken the immune system, potentially increasing susceptibility to inflammation. Smoking is a well-documented environmental risk factor, as is a lack of exposure to certain microorganisms in early childhood.
Prevalence in Different Populations
The prevalence of Crohn’s Colitis varies across different populations. Factors like ethnicity, socioeconomic status, and geographical location can influence the frequency of the disease. For example, studies have shown that individuals of Ashkenazi Jewish descent may have a higher risk compared to other groups. Variations in environmental exposures and genetic backgrounds likely contribute to these observed differences.
Crohn’s colitis, a form of inflammatory bowel disease, can be a real challenge to manage. Understanding treatment options like Stelara (ustekinumab) is key, and learning more about stelara ustekinumab what you should know can help. Ultimately, though, the best approach to Crohn’s colitis depends on individual needs and symptoms, and it’s important to discuss all options with your doctor.
Summary Table
| Potential Causes | Risk Factors | Protective Factors | Further Considerations |
|---|---|---|---|
| Overactive immune response, gut microbiome imbalance, infections | Family history, smoking, certain diets, stress, lack of early childhood exposure to certain microorganisms | Maintaining a healthy gut microbiome, managing stress, following a balanced diet, limiting smoking | Ongoing research is necessary to fully understand the intricate relationship between these factors and the disease. |
Diagnosis and Treatment
Navigating Crohn’s Colitis involves a multifaceted approach, encompassing accurate diagnosis and effective treatment strategies. Understanding the diagnostic process and the range of treatment options is crucial for managing the disease and improving quality of life. The journey often requires collaboration between patients and healthcare professionals to tailor a plan that best addresses individual needs.Crohn’s Colitis diagnosis hinges on a careful evaluation of symptoms, medical history, and physical examination.
This is followed by a series of tests to confirm the suspected diagnosis. Early and precise diagnosis allows for prompt treatment, which can significantly impact the course of the disease.
Diagnostic Methods
Confirming a diagnosis of Crohn’s Colitis necessitates a combination of methods. This approach is essential to rule out other conditions with similar symptoms and to establish the extent and location of inflammation within the digestive tract.
- Colonoscopy: This procedure involves inserting a flexible tube with a camera into the rectum and colon to visualize the lining. Biopsies can be taken during the procedure to examine tissue samples under a microscope for inflammation and characteristic patterns.
- Endoscopy: Similar to a colonoscopy, but focused on the upper digestive tract (esophagus, stomach, and duodenum). This helps determine if the inflammation extends beyond the colon.
- Imaging Tests: X-rays, CT scans, and MRI scans can reveal structural abnormalities in the digestive tract, including narrowing or inflammation. These provide critical insights into the extent and location of the disease.
- Blood Tests: Blood tests can reveal markers of inflammation, such as elevated C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR). They also help identify anemia or other complications associated with Crohn’s Colitis.
- Stool Tests: These tests can detect the presence of blood, white blood cells, or other abnormalities in the stool, which may suggest inflammation or infection.
Treatment Options
Effective management of Crohn’s Colitis requires a personalized approach. Treatment aims to reduce inflammation, control symptoms, and prevent complications.
- Medications: Pharmacological interventions play a significant role in managing Crohn’s Colitis. Different medications target various aspects of the disease process.
- Nutritional Support: A balanced diet, tailored to individual needs, can help manage symptoms and promote healing. This often includes dietary modifications to reduce digestive stress.
- Surgery: In some cases, surgery may be necessary to remove affected portions of the digestive tract or to repair complications, such as strictures or fistulas. This is often a last resort when other treatments are ineffective.
Medications Used
A variety of medications are used to manage Crohn’s Colitis, each with specific mechanisms of action and potential side effects.
- Aminosalicylates: These medications, such as mesalamine, aim to reduce inflammation in the colon.
- Corticosteroids: These potent anti-inflammatory drugs, such as prednisone, can quickly reduce inflammation but are often used for short periods due to potential side effects.
- Immunomodulators: Medications like azathioprine and 6-mercaptopurine can modify the immune response, potentially reducing inflammation and improving long-term outcomes.
- Biologics: These targeted therapies, such as infliximab and adalimumab, are effective in reducing inflammation by blocking specific proteins in the immune system.
Diagnostic and Treatment Summary
| Diagnostic Method | Treatment Option | Potential Side Effects | Example |
|---|---|---|---|
| Colonoscopy | Aminosalicylates | Gastrointestinal upset, headache | Mesalamine |
| Endoscopy | Corticosteroids | Increased appetite, insomnia | Prednisone |
| Imaging Tests | Immunomodulators | Liver problems, infections | Azathioprine |
| Blood Tests | Biologics | Injection site reactions, infections | Infliximab |
Management and Lifestyle
Living with Crohn’s Colitis requires a proactive approach that encompasses both medical interventions and lifestyle adjustments. Effective management hinges on understanding how daily choices impact the course of the disease. By embracing healthy habits and tailored strategies, individuals can significantly improve their quality of life and manage symptoms effectively.
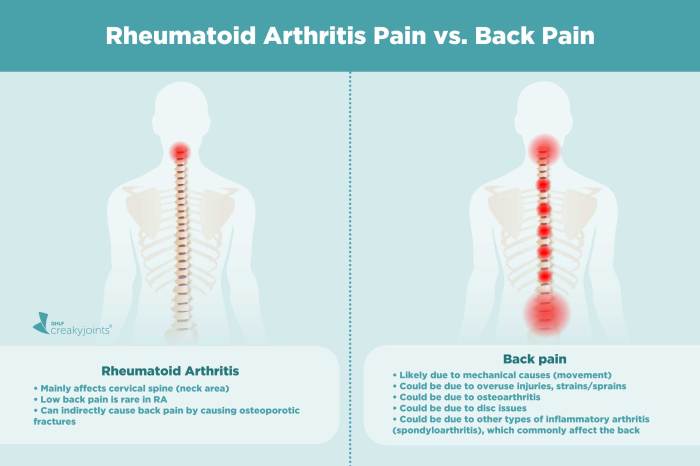
Crohn’s colitis, a form of inflammatory bowel disease, can cause a whole host of digestive issues. While not directly related, experiencing acute low back pain can sometimes be a symptom of a more serious underlying issue, like Crohn’s. If you’re struggling with this, checking out this article on acute low back pain try this first might offer some helpful insights into potential causes and treatments.
However, it’s crucial to remember that Crohn’s colitis needs to be diagnosed and managed by a medical professional.
Dietary Modifications
Dietary management plays a crucial role in Crohn’s Colitis management. Individual responses to different foods vary, necessitating a personalized approach. The goal is to identify and minimize triggers that exacerbate inflammation and discomfort.
- A balanced and nutrient-rich diet, emphasizing easily digestible foods, is paramount. This often involves limiting high-fiber foods initially to reduce digestive strain and focus on easily digestible proteins and carbohydrates.
- Avoiding trigger foods is essential. These foods may vary from person to person, but common culprits include fatty or greasy foods, spicy foods, alcohol, caffeine, and certain dairy products.
- Frequent, small meals throughout the day are frequently recommended to avoid overloading the digestive system, which can be particularly helpful for managing symptoms.
- Hydration is critical. Maintaining adequate fluid intake helps maintain bowel regularity and aids in nutrient absorption.
Stress Management Techniques
Stress can exacerbate Crohn’s Colitis symptoms. Implementing stress management strategies can be instrumental in improving overall well-being and managing the disease.
- Mindfulness and meditation practices can help individuals regulate their stress response. Regular practice can foster a sense of calm and reduce anxiety.
- Yoga and tai chi are also beneficial. These practices combine physical postures and breathing techniques, promoting relaxation and reducing stress.
- Engaging in hobbies and activities that bring joy and relaxation, such as reading, listening to music, or spending time in nature, can provide respite from stress and promote a sense of well-being.
Exercise Routines
Regular physical activity can contribute to overall health and well-being, which is particularly beneficial for managing Crohn’s Colitis. It is important to consult with a healthcare provider before starting any new exercise regimen.
- Low-impact exercises, such as swimming, walking, or cycling, are generally recommended. These activities are gentler on the digestive system and can help improve overall fitness without exacerbating symptoms.
- Consistency is key. Aim for regular exercise, even if it’s just for short periods, to maintain a healthy lifestyle.
- Listen to your body. Rest when needed and avoid overexertion, which can potentially trigger symptoms.
Daily Routine Organization
A structured daily routine can facilitate the management of Crohn’s Colitis by optimizing medication schedules, dietary adherence, and activity levels.
- A daily schedule should incorporate medication times, meal schedules, and exercise routines. Consistency in these aspects can aid in maintaining symptom control and minimizing flare-ups.
- Scheduling specific times for stress-reducing activities, such as meditation or yoga, can contribute to overall well-being and help manage symptoms effectively.
- Maintaining a food diary can help identify potential triggers and patterns associated with symptoms. This provides valuable insights into how dietary choices affect the disease.
Complications and Prognosis
Living with Crohn’s Colitis can be challenging, and understanding potential complications and long-term effects is crucial for effective management. This section delves into the complexities of Crohn’s, focusing on the various complications that can arise, their impact on quality of life, and strategies for mitigation. We’ll also explore the overall prognosis for individuals with this condition, considering factors that influence the course of the disease.
Potential Complications
Crohn’s Colitis, while often manageable, can lead to a range of complications. These complications can affect various parts of the body, impacting health and well-being. Some complications can be quite serious, requiring immediate medical attention.
- Strictures and Obstructions: Scar tissue formation (strictures) can narrow the intestines, leading to blockages (obstructions). This can cause severe pain, vomiting, and potentially require surgery for relief. A common example is a patient experiencing persistent abdominal discomfort and a change in bowel habits, eventually requiring surgical intervention to restore normal bowel function.
- Fistulas: Abnormal connections (fistulas) can form between the intestines and other organs, such as the bladder or vagina. These fistulas can cause infections, pain, and drainage. This complication often necessitates careful medical monitoring and potentially surgical repair.
- Abscesses: Collections of pus (abscesses) can develop within the abdomen. These infections can cause significant pain and fever and may require drainage procedures.
- Nutritional Deficiencies: Malabsorption and poor dietary intake due to the disease can lead to deficiencies in essential vitamins and minerals. These deficiencies can range from anemia to vitamin B12 deficiency. A patient with Crohn’s may experience fatigue and weakness due to these nutritional deficiencies, necessitating dietary adjustments and potentially supplemental therapies.
- Anal Fistulas and Fissures: Inflammation in the anal area can lead to painful fissures (tears) and fistulas. These conditions can cause significant discomfort and require treatment.
Long-Term Effects
The long-term effects of Crohn’s Colitis can vary significantly among individuals. While the disease can impact various aspects of life, it’s important to acknowledge that proactive management and ongoing medical care can significantly improve outcomes.
- Reduced Quality of Life: The chronic nature of Crohn’s Colitis can significantly impact daily life, leading to fatigue, pain, and emotional distress. This is often a consequence of frequent hospitalizations, surgeries, and other complications.
- Increased Risk of Cancer: Individuals with long-standing Crohn’s Colitis have an increased risk of developing colorectal cancer. Regular screening is crucial for early detection and intervention.
- Joint Pain (Enteropathic Arthritis): Some individuals experience joint pain and inflammation as a manifestation of the disease. This is known as enteropathic arthritis and can affect various joints in the body.
Nutritional Deficiencies, What is crohns colitis
The inflammatory nature of Crohn’s Colitis can interfere with the absorption of essential nutrients, leading to a range of deficiencies.
Crohn’s colitis is a chronic inflammatory bowel disease, causing significant discomfort. While I’ve been researching its complexities, I’ve also been curious about something seemingly unrelated: is talking to yourself normal? It turns out there’s a lot of interesting research on that topic too, if you’re interested in learning more, check out this article about is talking to yourself normal.
Ultimately, though, understanding Crohn’s colitis is still my main focus, and I’m determined to uncover more about its causes and treatments.
- Iron Deficiency Anemia: Chronic inflammation can impair iron absorption, leading to anemia.
- Vitamin B12 Deficiency: Malabsorption can lead to a deficiency in vitamin B12.
- Calcium Deficiency: Chronic inflammation can affect calcium absorption.
- Other Deficiencies: Deficiencies in other vitamins and minerals, such as folate and vitamin D, are also possible.
Overall Prognosis
The prognosis for individuals with Crohn’s Colitis is highly variable. While the disease can be challenging, significant improvements in treatment and management have led to better outcomes for many. Early diagnosis and effective treatment can greatly influence the long-term course of the disease.
Potential Complications Table
| Potential Complication | Impact | Prevention Strategies | Examples |
|---|---|---|---|
| Strictures and Obstructions | Pain, vomiting, potential surgery | Regular medical checkups, adherence to treatment plan | Bowel blockages, needing emergency surgery |
| Fistulas | Infections, pain, drainage | Early diagnosis and treatment, strict adherence to medication regimens | Connections between intestines and other organs, requiring surgical intervention |
| Abscesses | Pain, fever, potential surgery | Prompt medical attention for infections, proper wound care | Pus collections in the abdomen, needing drainage procedures |
| Nutritional Deficiencies | Weakness, fatigue, anemia | Balanced diet, nutritional supplements, regular monitoring | Iron deficiency, vitamin B12 deficiency |
Research and Future Directions
The quest to understand and conquer Crohn’s Colitis continues to drive intense research efforts. Scientists are exploring various avenues, from deciphering the intricate pathophysiology of the disease to developing novel and more effective treatment strategies. This ongoing investigation promises to improve the lives of those affected by this chronic condition.Current research is meticulously examining the complex interplay of genetics, environmental factors, and the immune system’s response in Crohn’s Colitis.
This comprehensive approach seeks to pinpoint the precise triggers and mechanisms that lead to inflammation and damage within the digestive tract.
Current Research Efforts
Researchers are actively investigating the role of specific genetic variations in susceptibility to Crohn’s Colitis. They are also exploring environmental triggers, such as diet, infections, and stress, that might contribute to the disease’s development. Understanding these factors is crucial for developing preventative strategies and personalized treatment plans. Further, the immune response within the digestive tract is under intense scrutiny.
Researchers are trying to decipher how dysregulation of the immune system leads to chronic inflammation in Crohn’s Colitis.
Advancements in Treatments
Significant progress has been made in the development of targeted therapies. These treatments aim to modulate the immune response, reduce inflammation, and promote healing in the affected areas. One example is the development of biologics that specifically target inflammatory pathways. This approach allows for a more precise and effective treatment strategy, minimizing side effects. Another avenue of research focuses on developing therapies that stimulate tissue repair and regeneration, aiding in long-term recovery.
Potential Future Research Areas
Future research efforts are expected to focus on precision medicine approaches for Crohn’s Colitis. This involves developing personalized treatment strategies based on individual genetic profiles and disease characteristics. Further, the development of early diagnostic tools and biomarkers will be crucial. These tools could help in early detection and prompt intervention, leading to improved outcomes. Finally, the exploration of novel therapeutic targets beyond the immune system is a promising avenue.
Researchers are looking into factors such as the gut microbiome and its role in the disease’s progression.
Pathophysiology: Current Understanding
The current understanding of Crohn’s Colitis pathophysiology revolves around the concept of an overactive immune response in the digestive tract. This leads to inflammation and damage in various segments of the intestine. The inflammation can cause lesions and ulcers, disrupting the normal functioning of the digestive system. The exact mechanisms behind this immune dysregulation remain under investigation.
The interplay between genetic predisposition, environmental triggers, and the gut microbiome are key elements in the complex pathogenesis.
A Potential Experimental Treatment Approach
One potential experimental treatment approach for Crohn’s Colitis involves the use of mesenchymal stem cells. These cells have the potential to reduce inflammation, promote tissue repair, and modulate the immune response. They may also restore the balance of the gut microbiome. The approach involves isolating and modifying these cells to target the specific inflammatory pathways in the affected areas.
The therapeutic effect would be achieved by the cells’ regenerative capacity and anti-inflammatory properties.
End of Discussion
In conclusion, Crohn’s Colitis is a multifaceted disease requiring a multi-pronged approach to management. From understanding its diverse symptoms and stages to exploring the potential causes and diagnostic methods, this exploration provides a comprehensive overview. The crucial role of lifestyle modifications, dietary changes, and stress management, alongside appropriate medical interventions, cannot be overstated. Ultimately, managing Crohn’s Colitis effectively requires a strong understanding of the condition and a collaborative approach between patients, healthcare professionals, and support networks.
Further research and ongoing advancements in treatment hold promise for improved outcomes in the future.

/leukemia-myeloid-250x-at-35mm-this-type-of-leukemia-has-its-origin-in-the-bone-marrow-myeloid-tissue-it-involves-a-malignant-proliferation-of-immature-white-blood-cells-this-action-can-crowd-out-production-of-rbc-s-and-platelets-leading-to-an--58aca68c3df78c345b81d051.jpg?w=700)