Bendopnea a new symptom of heart failure – Bendopnea, a new symptom of heart failure, describes a specific type of shortness of breath that occurs when bending over. This distinct respiratory response, different from typical dyspnea, may indicate underlying heart conditions. Understanding its characteristics, physiological mechanisms, and clinical presentation is crucial for accurate diagnosis and…
Category: Health Conditions
Celiac Disease Symptoms in Women A Deep Dive
Celiac disease symptoms in women often manifest differently than in men, leading to unique challenges in diagnosis and management. This comprehensive guide explores the spectrum of symptoms, from common gastrointestinal issues to less-obvious non-gastrointestinal problems, providing valuable insights for women experiencing potential symptoms. The prevalence of celiac disease in women compared to men, along with…
What is the Latex Food Syndrome? A Deep Dive
What is the latex food syndrome? This intriguing condition connects seemingly unrelated foods, triggering allergic reactions in susceptible individuals. It’s not just about a simple aversion; it’s a complex interplay of immune responses and a wide range of symptoms. This exploration delves into the nuances of latex food syndrome, from its underlying mechanisms to the…
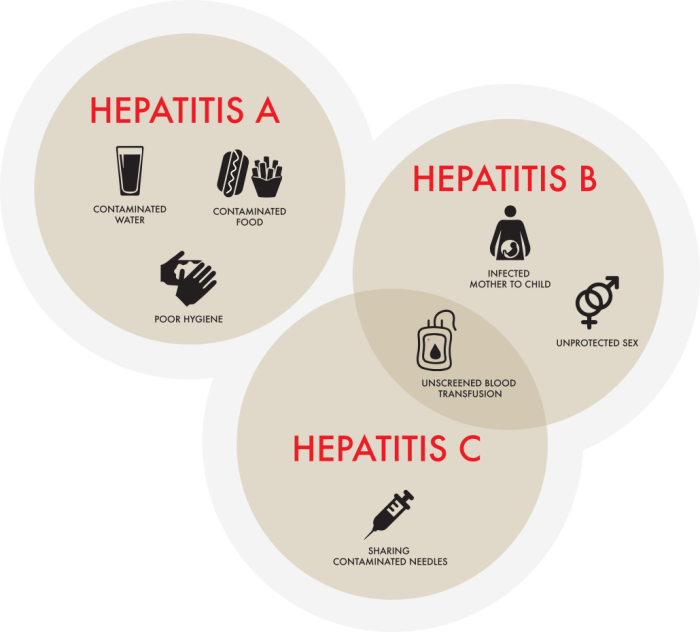
Which Hepatitis is the Worst? A Deep Dive
Which hepatitis is the worst? This question often arises, but there’s no single answer. The severity of hepatitis, a liver inflammation, varies significantly depending on the type (A, B, C, D, E) and individual factors. Understanding the different types, their transmission methods, and the potential long-term consequences is crucial for informed discussion. This exploration delves…
What is Barretts Esophagus A Deep Dive
What is barretts esophagus – What is Barrett’s esophagus? This condition occurs when the lining of your esophagus, the tube connecting your mouth and stomach, changes. It’s a significant health concern that can lead to serious complications if not properly managed. This in-depth exploration will delve into the causes, symptoms, diagnosis, complications, treatment options, and…
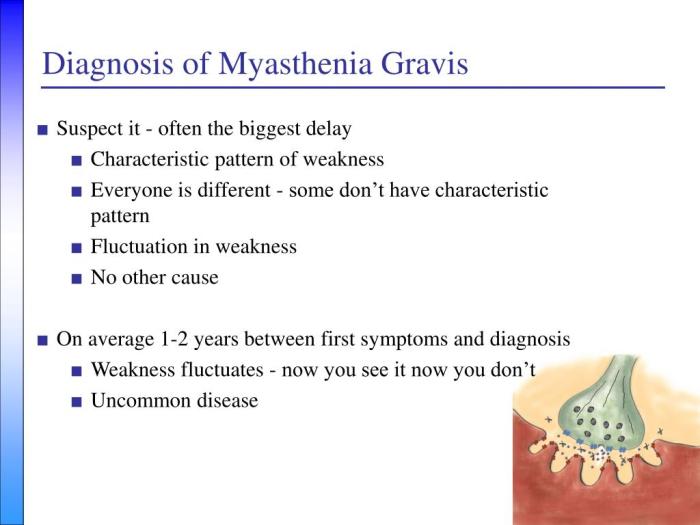
How Myasthenia Gravis Is Diagnosed A Comprehensive Guide
How myasthenia gravis is diagnosed is a crucial process, often involving a multifaceted approach. This journey begins with recognizing the subtle and sometimes overlooked initial symptoms, progressing through neurological examinations, and culminating in a series of diagnostic tests. Understanding the various methods used in the diagnostic process can help patients and their families navigate this…
Signs of Liver Disease Early Detection Matters
Signs of liver disease can be subtle, often overlooked, but early detection is crucial. This guide delves into the various indicators, from common symptoms to risk factors, empowering you to understand your liver health better. We’ll explore different types of liver disease, their causes, and how to recognize the early warning signs. From digestive issues…
Autoimmunity Neuroinflammation in Fibromyalgia Unveiling the Link
Autoimmunity neuroinflammation in fibromyalgia is a fascinating and complex area of research. This condition, characterized by widespread pain and fatigue, is increasingly understood to involve interactions between the immune system and the nervous system. We’ll delve into the potential mechanisms by which these processes intertwine, exploring the suspected roles of autoimmunity and neuroinflammation in the…
Drugs That Cause Erectile Dysfunction A Comprehensive Guide
Drugs that cause erectile dysfunction are a significant concern for many men. This issue is often overlooked, but understanding the various medications that can lead to erectile problems is crucial for maintaining overall health and well-being. This guide will explore the mechanisms by which certain drugs impact erectile function, examining specific drug categories, underlying mechanisms,…
Back Pain A Lung Cancer Symptom
Back pain as a symptom of lung cancer is a complex and often overlooked possibility. While back pain is frequently associated with other conditions, its unusual manifestation in relation to lung cancer warrants careful consideration. This exploration delves into the potential link, highlighting the various ways back pain can manifest, its location, characteristics, and the…