Stages of palliative care guides patients and families through a journey of support and understanding. It’s a multifaceted approach, acknowledging the varying needs and challenges individuals face as their illness progresses. From initial diagnosis to end-of-life care, each stage presents unique opportunities for symptom management, communication, and emotional support. This exploration delves into the key elements that define the trajectory of palliative care, highlighting the evolving needs of patients and their loved ones.
This overview will cover the different phases of palliative care, the evolving symptoms, and the specific interventions used in each stage. We will explore the crucial roles of healthcare professionals, family members, and the patient in navigating this journey. Furthermore, we will discuss the importance of cultural sensitivity and ethical considerations throughout the process.
Introduction to Palliative Care
Palliative care is a specialized medical approach focused on improving the quality of life for individuals facing serious illness. It’s not about curing the disease, but rather about providing comprehensive support and relief from symptoms and stress associated with the illness. This support encompasses physical, emotional, social, and spiritual needs, aiming to enhance comfort and well-being throughout the entire course of the illness.This approach differs significantly from curative treatment, instead prioritizing the patient’s current needs and preferences.
It recognizes that the patient’s experience extends beyond medical interventions, encompassing the psychological and social aspects of their journey.
Key Differences Between Palliative Care and Hospice Care
Palliative care can be provided at any stage of a serious illness, even alongside curative treatments. Hospice care, on the other hand, is specifically for individuals whose life expectancy is estimated to be six months or less, and who have chosen to forgo curative treatments. Both approaches focus on comfort and quality of life, but hospice care typically takes over when curative efforts are no longer pursued.
A key differentiator lies in the timing and nature of care.
Philosophy and Principles of Palliative Care
Palliative care is grounded in a philosophy of holistic care, recognizing the interconnectedness of physical, emotional, social, and spiritual well-being. Key principles underpinning this approach include:
- Patient-centered care: Care decisions are driven by the patient’s values, preferences, and goals, ensuring their autonomy is respected.
- Symptom management: Addressing physical symptoms like pain, shortness of breath, nausea, and fatigue is a core component of palliative care.
- Emotional and psychological support: Palliative care addresses the emotional and psychological distress associated with serious illness, offering counseling and support to both the patient and their family.
- Spiritual and existential concerns: Palliative care acknowledges the importance of spiritual and existential needs, offering support for patients’ beliefs and values.
- Family and caregiver support: Caregivers and family members are actively involved in the care plan, receiving support and education to better manage their roles.
Settings for Palliative Care Services
Palliative care services are available in a variety of settings, ensuring accessibility and tailored care.
| Setting | Description |
|---|---|
| Hospitals | Palliative care teams often integrate within hospital settings, providing expertise to patients facing serious illness across various departments. |
| Clinics | Outpatient clinics provide specialized care and support to patients requiring ongoing palliative care outside of a hospital stay. |
| Nursing Homes | Palliative care teams can work with residents in nursing homes to enhance their comfort and quality of life. |
| Home Healthcare | Many patients benefit from palliative care services in their homes, allowing them to receive care in a familiar and comfortable environment. |
Stages of Palliative Care
Navigating the complexities of palliative care requires understanding the diverse needs of patients across different stages of their journey. This understanding empowers healthcare professionals to tailor interventions and support, optimizing comfort and quality of life. The progression of palliative care is not linear, and individuals may experience symptoms and challenges differently.This exploration delves into the typical stages of palliative care, outlining the evolving needs, common symptoms, and interventions employed at each phase.
This framework aims to provide a clearer picture of the dynamic nature of palliative care and how it adapts to the unique circumstances of each patient.
Early Stage of Palliative Care
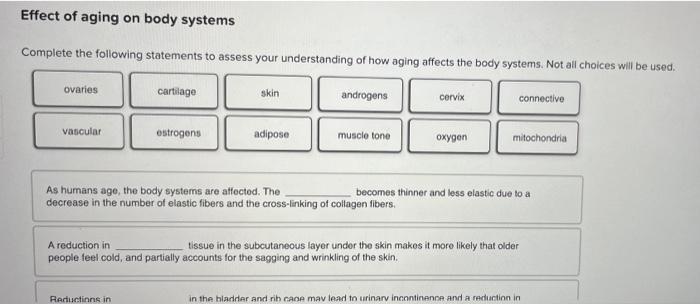
This phase typically involves the initial diagnosis of a life-limiting illness and the introduction of palliative care services. Patients often experience a range of emotional responses, including anxiety, fear, and grief. Physical symptoms might include fatigue, pain, or changes in appetite. Interventions at this stage often focus on symptom management, emotional support, and establishing a care plan.
This includes discussions about goals of care, preferences for treatment, and the introduction of medications to manage symptoms.
Understanding the stages of palliative care is crucial for navigating complex health journeys. It’s about recognizing different phases, from diagnosis to end-of-life support. Sometimes, physical symptoms like finger locking can complicate these stages. For instance, if you’re experiencing issues like this, understanding the underlying causes can be key to managing symptoms effectively, such as in cases of why do my fingers lock up.
Ultimately, palliative care provides comfort and support through each stage of this challenging process.
Middle Stage of Palliative Care
As the illness progresses, patients in the middle stage may experience worsening symptoms, such as increased pain, shortness of breath, or difficulty swallowing. The need for more intensive symptom management and support becomes evident. Common challenges include navigating treatment decisions, adjusting to functional limitations, and managing escalating emotional distress. Interventions might involve adjustments to medications, the introduction of complementary therapies, and ongoing communication with family members.
Understanding the stages of palliative care is crucial for navigating the complexities of this journey. It’s a multifaceted process, much like a microdermabrasion treatment, where different phases involve varying levels of support and care. For example, learning what to expect during a microdermabrasion treatment here helps you anticipate the steps and prepare for the outcomes. Ultimately, palliative care aims to improve quality of life during these different stages.
Late Stage of Palliative Care
In the late stage, patients often experience a decline in physical function, with symptoms potentially becoming more severe and distressing. The focus shifts to maintaining comfort, dignity, and quality of life, often in the context of reduced responsiveness or inability to communicate. Common challenges include managing complex symptom clusters, supporting the patient’s and family’s emotional needs, and preparing for the end-of-life phase.
Interventions at this stage often involve maximizing comfort measures, such as pain management, and providing emotional support to both the patient and their family.
Table Comparing Stages of Palliative Care
| Stage | Primary Goals | Common Interventions |
|---|---|---|
| Early Stage | Symptom management, emotional support, establishing care plan, shared decision-making. | Symptom management medications, emotional counseling, advance care planning discussions, introduction of palliative care team. |
| Middle Stage | Enhanced symptom management, addressing functional limitations, adjusting treatment plans, supporting emotional well-being. | Adjustments to medications, introduction of complementary therapies, ongoing communication with family, psychosocial support. |
| Late Stage | Maximizing comfort, preserving dignity, ensuring quality of life, supporting family. | Aggressive pain management, comfort measures, emotional support for patient and family, advanced directives review. |
Assessment and Evaluation in Palliative Care
Accurate and comprehensive assessment is fundamental to effective palliative care. It’s not just about identifying symptoms; it’s about understanding the patient’s holistic needs, preferences, and values within the context of their illness and life situation. A thorough assessment forms the basis for developing a personalized care plan that addresses physical, emotional, social, and spiritual needs.
Importance of Comprehensive Patient Assessments
A comprehensive assessment in palliative care goes beyond simply recording symptoms. It delves into the patient’s overall experience of illness, considering their physical, emotional, social, and spiritual well-being. This multifaceted approach allows healthcare providers to create a personalized care plan that addresses the patient’s unique needs and preferences. Such a plan is vital for achieving optimal quality of life for the patient and their family.
Methods Used to Assess Patient Needs and Preferences
Various methods are employed to gain a deep understanding of the patient’s needs and preferences. These methods include standardized symptom scales, functional assessments, and interviews with the patient and their family. Symptom scales, such as the Edmonton Symptom Assessment System (ESAS), provide a quantifiable measure of symptom severity, enabling consistent tracking and evaluation of treatment effectiveness. Functional assessments, including the Katz Index of Independence in Activities of Daily Living (ADL) and the Lawton Instrumental Activities of Daily Living (IADL) scale, evaluate the patient’s ability to perform daily tasks, offering valuable insight into their independence and support requirements.
- Symptom Scales: These scales, like the Edmonton Symptom Assessment Scale (ESAS), allow for objective measurement of symptom severity (e.g., pain, nausea, fatigue). They facilitate consistent tracking and comparison, helping to evaluate the effectiveness of interventions.
- Functional Assessments: These tools evaluate the patient’s ability to perform activities of daily living (ADLs) and instrumental activities of daily living (IADLs). Examples include the Katz ADL scale and the Lawton IADL scale. This helps determine the level of support required and plan for assistance.
- Patient Interviews: Direct conversations with the patient are crucial. These interviews explore the patient’s perception of their illness, their values, and their preferences for care. Open-ended questions allow the patient to express their needs and concerns, which are often more valuable than standardized measures.
Role of Family Members and Caregivers in the Assessment Process
Family members and caregivers play an indispensable role in the assessment process. Their insights into the patient’s daily life, their preferences, and their understanding of the patient’s emotional and social needs are invaluable. Their perspective helps to create a holistic picture of the patient’s situation, crucial for a personalized care plan.
- Family Input: Gathering information from family members helps understand the patient’s usual routines, emotional responses, and preferences in various situations. Their knowledge about the patient’s past and present health provides valuable context.
- Caregiver Perspectives: Caregivers are often the primary source of support and care. Their input on the patient’s needs, preferences, and challenges in daily life is essential for planning adequate care and support.
Key Elements in a Palliative Care Assessment
| Category | Elements |
|---|---|
| Physical | Pain, shortness of breath, fatigue, nausea, appetite, bowel/bladder function, mobility, sleep |
| Emotional | Anxiety, depression, fear, isolation, loss, grief |
| Social | Support system, social interactions, living arrangements, financial resources, cultural needs |
| Spiritual | Meaning and purpose in life, beliefs, values, religious affiliation, sense of hope |
| Practical | Advance care planning documents, living will, end-of-life wishes, needs for support, preferences for care |
This table provides a framework for a comprehensive assessment. The specific elements to include in each category may vary depending on the individual patient’s needs and circumstances.
Symptom Management
Symptom management is a cornerstone of high-quality palliative care. It’s not just about relieving discomfort; it’s about enhancing the patient’s overall well-being and quality of life during a challenging time. Effective symptom management allows patients to remain active, engaged, and comfortable, which is crucial for maintaining dignity and preserving their sense of self. This approach emphasizes holistic care, addressing not only the physical symptoms but also the emotional, social, and spiritual needs of the individual.A wide array of symptoms can affect palliative care patients.
Understanding and effectively managing these symptoms is paramount to providing compassionate and supportive care. These symptoms can range from the expected, like pain and nausea, to less obvious, but equally impactful, concerns like anxiety and depression. Effective symptom management requires a personalized approach, tailoring interventions to each patient’s unique needs and preferences.
Common Symptoms in Palliative Care
Palliative care patients frequently experience a range of symptoms that impact their daily lives. Recognizing these symptoms and implementing appropriate interventions is essential for maintaining patient comfort and well-being. Pain, nausea, shortness of breath, fatigue, and anxiety are among the most common symptoms. Other potential issues include insomnia, constipation, loss of appetite, and delirium.
Approaches to Symptom Management
Effective symptom management in palliative care often involves a multifaceted approach, combining pharmacological and non-pharmacological interventions. A holistic perspective is crucial, considering the patient’s physical, emotional, social, and spiritual needs. This means tailoring interventions to the individual’s specific situation, preferences, and values. Simply addressing the physical discomfort is not enough; the emotional and psychological impact of the illness and its treatment must also be considered.
Symptom Management Strategies
Symptom management in palliative care requires a careful consideration of both pharmacological and non-pharmacological approaches. A comprehensive strategy often involves a combination of these methods to achieve optimal results.
- Pharmacological Approaches: These strategies involve the use of medications to control symptoms. Pain management often requires a combination of analgesics, such as opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and adjuvant medications. Nausea and vomiting can be managed with antiemetics, while shortness of breath might necessitate bronchodilators or oxygen therapy. The selection of medications and dosages is carefully determined by the healthcare team, considering potential side effects and interactions with other medications.
- Non-Pharmacological Approaches: These strategies encompass a wide range of interventions that do not involve medications. For example, techniques like relaxation exercises, guided imagery, and music therapy can be valuable in managing anxiety and pain. Physical therapy and occupational therapy can help maintain mobility and independence. Nutritional support, including dietary modifications and supplements, can also play a vital role in managing symptoms like loss of appetite.
Furthermore, emotional support, counseling, and spiritual care can significantly contribute to symptom management by addressing the emotional and psychological dimensions of the illness.
Symptom Management Table
| Symptom | Pharmacological Approaches | Non-Pharmacological Approaches |
|---|---|---|
| Pain | Opioids, NSAIDs, adjuvant analgesics | Relaxation techniques, massage, acupuncture, guided imagery |
| Nausea | Antiemetics | Dietary modifications, acupressure, ginger |
| Shortness of Breath | Bronchodilators, oxygen therapy | Positioning, breathing exercises, relaxation techniques |
| Constipation | Laxatives, stool softeners | Dietary fiber, increased fluid intake, exercise |
| Anxiety | Anxiolytics | Counseling, relaxation techniques, support groups, mindfulness |
Communication and Support

Effective communication and compassionate support are cornerstones of high-quality palliative care. These elements not only enhance the patient’s experience but also provide crucial assistance to families navigating this challenging journey. Open dialogue fosters trust and understanding, enabling patients to express their needs and preferences, and allowing healthcare professionals to tailor their approach to each individual’s unique circumstances.Understanding the patient’s perspective and honoring their choices are paramount.
This necessitates a multi-faceted approach, including active listening, empathy, and the ability to convey complex information clearly and sensitively. Families play a vital role in this process, and their involvement should be encouraged and facilitated.
Importance of Effective Communication
Open and honest communication between healthcare providers, patients, and families is essential. Shared understanding and a common language are vital for creating a supportive and trusting environment. This shared understanding empowers patients to actively participate in their care decisions, leading to a more positive and fulfilling experience. It allows for the exploration of concerns, the expression of emotions, and the clarification of expectations.
Understanding the stages of palliative care is crucial for navigating the complexities of this journey. It’s important to remember that everyone experiences these stages differently, and finding comfort and support along the way is key. Sometimes, simple self-care measures like soaking your feet in epsom salt for feet here can provide a much-needed respite, and this can be beneficial during any stage of palliative care.
Ultimately, focusing on quality of life and comfort is paramount in these stages.
Communication Strategies
Various strategies can improve the patient experience in palliative care. These include active listening, empathetic responses, and clear, concise explanations of medical information. Using simple language, avoiding jargon, and acknowledging the patient’s emotions are crucial. Acknowledging the patient’s emotional response to their condition is critical to building trust and fostering a supportive environment. Emphasizing hope and offering practical support, such as connecting patients with community resources, also contribute significantly.
Role of Psychosocial Support
Psychosocial support in palliative care addresses the emotional, psychological, and social needs of patients and their families. It recognizes that illness affects not only physical well-being but also mental and emotional health. This holistic approach is crucial for fostering a sense of comfort and dignity during a challenging time. This support can include counseling, support groups, and access to spiritual or religious resources.
For instance, a patient might benefit from grief counseling, while a family might find solace in a support group for caregivers.
Communication Methods for Different Situations
| Situation | Communication Method | Example |
|---|---|---|
| Delivering bad news | Direct, empathetic, and compassionate approach; use simple language; acknowledge emotions; offer support; provide written materials. | “Mr. Smith, unfortunately, the scans show a progression of the disease. We need to discuss options for managing the symptoms.” |
| Discussing end-of-life wishes | Create a safe space for open conversation; encourage the patient to express their desires; document these wishes; involve family members as appropriate; ensure the patient understands the implications of their choices. | “Mrs. Jones, we want to understand your preferences regarding medical interventions in the coming weeks. Could you share what you’d like to happen?” |
| Addressing concerns about pain management | Active listening; address concerns openly; provide information about available pain relief options; ensure patient comfort and safety; involve family members in decision-making. | “Mr. Patel, I understand you’re concerned about the side effects of the medication. Let’s discuss the potential risks and benefits, and we can explore alternative options.” |
| Providing updates on treatment progress | Regular, clear, and honest communication; provide realistic expectations; address concerns; avoid medical jargon; offer resources. | “Ms. Lee, we’ve seen a slight improvement in your condition. However, we need to be mindful of the potential for future complications. We’ll continue monitoring your condition closely.” |
Ethical Considerations: Stages Of Palliative Care
Navigating the complexities of palliative care often involves confronting challenging ethical dilemmas. These dilemmas arise from the multifaceted nature of patient needs, the varying perspectives of healthcare providers, and the inevitable uncertainties surrounding end-of-life decisions. Understanding these ethical considerations is crucial for ensuring compassionate and ethically sound care for patients and their families.
Ethical Dilemmas in Palliative Care
Palliative care professionals face a range of ethical dilemmas, often involving conflicts between patient autonomy, family wishes, and the healthcare team’s professional obligations. These situations frequently involve decisions about treatment options, symptom management, and end-of-life care. For example, a patient might desire aggressive treatment, while their family members might prefer comfort measures and hospice care. These differing perspectives require careful consideration and sensitive communication to reach a mutually acceptable solution.
Patient Autonomy and Informed Consent
Patient autonomy is paramount in palliative care. Patients have the right to make informed decisions about their care, even when those decisions are difficult or unconventional. Informed consent involves providing patients with sufficient information about their condition, treatment options, and potential outcomes. This ensures that patients understand the implications of their choices and can make decisions that align with their values and preferences.
A crucial component of informed consent is ensuring the patient understands the information presented, and not just passively receiving it.
Advance Care Planning in Palliative Care
Advance care planning (ACP) plays a vital role in palliative care. ACP empowers patients to document their preferences regarding future medical care, including decisions about life-sustaining treatments. These documents, such as advance directives or living wills, provide guidance for healthcare providers when patients are unable to communicate their wishes directly. This proactive approach helps ensure that care aligns with the patient’s values and goals, reducing potential conflicts and promoting patient autonomy.
ACP helps families navigate difficult decisions, too, by providing clear guidance from the patient’s perspective.
Common Ethical Principles in Palliative Care
| Ethical Principle | Description | Example |
|---|---|---|
| Beneficence | Acting in the best interest of the patient. | Prioritizing symptom relief and comfort measures to maximize quality of life. |
| Non-maleficence | Avoiding actions that could harm the patient. | Carefully weighing potential risks and benefits of treatment options, avoiding interventions that could cause unnecessary suffering. |
| Autonomy | Respecting the patient’s right to make decisions about their own care. | Honoring a patient’s choice to refuse treatment, even if it is against medical advice. |
| Justice | Ensuring fair and equitable access to palliative care services. | Providing equitable access to palliative care regardless of socioeconomic status or location. |
| Veracity | Being truthful and honest with patients and families. | Providing accurate information about the patient’s prognosis and treatment options. |
Interdisciplinary Team Collaboration
Palliative care is a multifaceted approach requiring a collaborative effort from various healthcare professionals. Effective interdisciplinary teamwork is crucial for providing holistic and patient-centered care, addressing the physical, emotional, social, and spiritual needs of individuals facing life-limiting illnesses. This collaborative approach ensures that patients receive comprehensive support throughout their journey.
The Critical Role of Interdisciplinary Teams
Interdisciplinary teams in palliative care bring together diverse expertise to create a comprehensive care plan. This approach is vital as it acknowledges the multifaceted nature of palliative care needs, encompassing physical symptoms, emotional distress, social support, and spiritual well-being. The expertise of different professionals, working in harmony, enhances the quality of care and improves patient outcomes.
Roles and Responsibilities of Healthcare Professionals
The success of palliative care hinges on the effective collaboration of various healthcare professionals. Each member plays a unique role, contributing their expertise to address the multifaceted needs of the patient and family.
- Physicians (e.g., oncologists, primary care physicians, palliative care specialists): Physicians are responsible for coordinating care, managing symptoms, and making treatment decisions in conjunction with the patient and family. They provide medical expertise, including diagnosis, prognosis, and treatment options, considering the patient’s goals and preferences.
- Nurses (e.g., registered nurses, palliative care nurses): Nurses play a critical role in providing direct patient care, assessing symptoms, administering medications, educating patients and families, and coordinating care with other team members. They are often the primary point of contact for patients and families.
- Social Workers: Social workers focus on the psychosocial aspects of palliative care. They help patients and families navigate the emotional and practical challenges of the illness, connect with community resources, and develop coping strategies. They also assist with advance care planning.
- Chaplains or Spiritual Counselors: These professionals address the spiritual and existential needs of patients and families, offering support and guidance in finding meaning and peace during a challenging time. They facilitate discussions about values, beliefs, and end-of-life wishes.
- Pharmacists: Pharmacists ensure appropriate medication management, including accurate prescribing, monitoring for adverse effects, and providing education about medications to patients and families.
- Physical Therapists, Occupational Therapists, and Speech-Language Pathologists: These professionals address physical limitations and functional impairments, enabling patients to maintain their independence and quality of life to the greatest extent possible. They develop individualized plans to manage pain, improve mobility, and enhance communication skills.
Examples of Interdisciplinary Collaboration
Effective interdisciplinary collaboration in palliative care can be exemplified by a case where a patient with advanced cancer experiences severe pain. The physician consults with the palliative care nurse to adjust pain medication, while the social worker connects the patient with community support services. The chaplain provides spiritual support, and the physical therapist helps maintain mobility and function.
This collaborative approach ensures the patient receives comprehensive and holistic care, addressing not only the physical pain but also the emotional and spiritual aspects of their experience.
Table of Roles and Responsibilities, Stages of palliative care
| Role | Primary Responsibilities |
|---|---|
| Physician | Diagnosis, prognosis, treatment decisions, symptom management, coordination of care. |
| Nurse | Direct patient care, symptom assessment, medication administration, education, coordination with team. |
| Social Worker | Psychosocial support, resource identification, advance care planning, family support. |
| Chaplain/Spiritual Counselor | Spiritual support, guidance, addressing existential needs, facilitating discussions on values. |
| Pharmacist | Medication management, monitoring for adverse effects, education on medications. |
| Physical Therapist | Physical limitations assessment, mobility improvement, functional restoration. |
| Occupational Therapist | Adaptive strategies, maintaining independence, daily living skills. |
| Speech-Language Pathologist | Communication support, swallowing difficulties assessment and management. |
Cultural Considerations
Understanding and respecting diverse cultural backgrounds is paramount in palliative care. Cultural beliefs, values, and practices profoundly influence how individuals and families perceive illness, death, and end-of-life care. This sensitivity is crucial for providing holistic and effective support during a challenging time. Failing to acknowledge and address these differences can lead to misunderstandings, mistrust, and ineffective interventions.
Importance of Cultural Sensitivity
Cultural sensitivity in palliative care necessitates a deep understanding of the diverse perspectives and experiences of patients and their families. This involves recognizing that cultural values shape individual responses to illness and suffering. It includes acknowledging that rituals, beliefs, and traditions surrounding death and dying vary significantly across cultures. A culturally sensitive approach ensures that care is tailored to meet the unique needs of each individual, fostering trust and enabling a more comfortable and respectful experience.
This sensitivity goes beyond mere awareness; it requires active engagement and a commitment to learning about and respecting different cultural norms.
Impact of Cultural Beliefs on End-of-Life Decisions
Cultural beliefs and practices significantly influence end-of-life decisions. For example, some cultures prioritize family-centered care, emphasizing the collective well-being of the family unit. Others might emphasize individual autonomy and personal preferences. Religious or spiritual beliefs may dictate specific rituals, preferences for treatment, and views on life-sustaining measures. A deep understanding of these beliefs is vital for navigating complex decisions regarding medical interventions, treatment choices, and end-of-life rituals.
Adapting Care to Meet Diverse Needs
Providing culturally sensitive palliative care requires adaptability and a willingness to learn. Care providers should actively seek information about the patient’s cultural background and preferences. Open communication, active listening, and a willingness to accommodate cultural practices are essential. For example, if a patient’s culture dictates a specific type of food or herbal remedy, incorporating those elements into the care plan can significantly enhance the patient’s comfort and well-being.
Similarly, understanding and respecting religious or spiritual practices is vital for providing culturally sensitive care. This could include allowing time for prayer, ensuring access to religious leaders, or accommodating specific dietary restrictions.
Table: Impact of Cultural Factors on Palliative Care
| Cultural Factor | Impact on Palliative Care | Examples of Adaptation |
|---|---|---|
| Family-centered care | Decisions about treatment and end-of-life care may be shared within the family unit, rather than solely with the individual patient. | Involving family members in care planning discussions and decision-making processes. |
| Spiritual beliefs | Religious or spiritual beliefs may influence preferences for treatment, rituals, and end-of-life care. | Providing access to religious leaders or spiritual advisors; accommodating prayer or meditation times. |
| Communication styles | Different cultures have varying communication styles, which may affect how information is shared and received. | Using interpreters if needed; being patient and understanding when communication styles differ. |
| Dietary restrictions | Dietary restrictions based on cultural or religious beliefs may need to be accommodated. | Ensuring access to culturally appropriate foods; adapting meal plans to meet specific needs. |
| Death rituals | Cultural practices surrounding death and dying may involve specific rituals or ceremonies. | Respecting and accommodating these rituals, such as traditional mourning practices or burial customs. |
Resources and Support for Patients and Families

Navigating the complexities of palliative care often requires comprehensive support for both patients and their families. This phase extends beyond medical interventions, encompassing emotional, practical, and spiritual needs. Understanding the available resources can significantly ease the burden and improve the quality of life for everyone involved.Accessing the right support can be overwhelming, but it’s crucial for successful palliative care.
This section details various resources, support groups, and organizations dedicated to assisting patients and families during this journey. Learning how to effectively access these resources is paramount to maximizing their benefits.
Available Resources for Patients and Families
Knowing where to turn for assistance can be challenging during a difficult time. A wide range of organizations and individuals are dedicated to providing support to those facing palliative care needs. This comprehensive list aims to highlight some of the most vital resources.
- Hospice Organizations: Hospice organizations play a pivotal role in providing comprehensive care for individuals facing life-limiting illnesses. They offer a wide array of services, including pain and symptom management, emotional support, and practical assistance. Many hospice programs offer bereavement support for families after the loss of a loved one.
- Support Groups: Support groups provide a vital space for patients and families to connect with others facing similar experiences. Sharing stories, exchanging advice, and receiving emotional support from others can be incredibly beneficial. Support groups can be facilitated by trained professionals or fellow members of the community.
- Professional Counselors and Therapists: Professional counselors and therapists offer specialized support for patients and families struggling with emotional distress, grief, or adjustment to a life-limiting illness. Their expertise in mental health can provide coping mechanisms and strategies for navigating the emotional challenges associated with palliative care.
- Social Workers: Social workers are invaluable resources for patients and families navigating the complexities of palliative care. They can assist with practical issues such as financial aid, housing, transportation, and other social needs. Social workers can also connect individuals with other relevant resources in the community.
- Spiritual Counselors: Spiritual counselors offer support to those seeking guidance on matters of faith, spirituality, or existential concerns. They provide a safe space to address spiritual needs and connect individuals with their faith communities or alternative support systems.
Accessing Resources Effectively
Finding the right resources requires proactive steps. It’s essential to understand the various options available and know how to connect with them.
- Online Databases: Online databases and search engines can provide a starting point for locating local resources. Many organizations have websites that list contact information, services offered, and eligibility criteria.
- Healthcare Providers: Healthcare providers, including physicians, nurses, and social workers, can often provide referrals to relevant resources in the community.
- Community Centers: Community centers, religious organizations, and volunteer groups may offer support services tailored to the specific needs of the community.
- Local Hospitals and Clinics: Hospitals and clinics often have their own resources and support systems for patients and families undergoing palliative care.
- Referral Services: Many organizations specialize in providing referrals to support services. These services can help individuals navigate the complex system of resources and connect with the most appropriate providers.
Table of Resources and Support Systems
This table summarizes various resources and support systems available for patients and families undergoing palliative care.
| Category | Resource | Description |
|---|---|---|
| Hospice Organizations | Hospice of [Local Area] | Provides comprehensive care, including symptom management, emotional support, and practical assistance. |
| Support Groups | [Local Support Group for [Specific Condition]] | Offers a space for patients and families to connect with others facing similar experiences. |
| Professional Counselors | [Name of local counseling service] | Provides specialized support for emotional distress, grief, or adjustment to a life-limiting illness. |
| Social Workers | [Name of local social work agency] | Assists with practical issues like financial aid, housing, and transportation. |
| Spiritual Counselors | [Name of local spiritual counseling service] | Provides guidance on matters of faith, spirituality, or existential concerns. |
Wrap-Up
In conclusion, navigating the stages of palliative care requires a holistic approach that encompasses physical, emotional, and spiritual well-being. The journey is unique for each individual, and the collaborative efforts of healthcare professionals, patients, and families are essential in providing the best possible support. This comprehensive framework underscores the significance of understanding the evolving needs of patients and their loved ones, emphasizing the importance of compassion, empathy, and respect throughout each stage.