Should I take Xiidra or Restasis to treat dry eye? This crucial question faces many struggling with this common eye condition. Dry eye, a frustrating ailment affecting millions, often leaves sufferers searching for effective relief. Understanding the nuances of different treatments is key, and this exploration delves into the specifics of Xiidra and Restasis, comparing their mechanisms, potential side effects, and ultimately, helping you decide which might be the best option for your needs.
We’ll also look at patient considerations, lifestyle factors, and when it’s essential to consult an eye care professional.
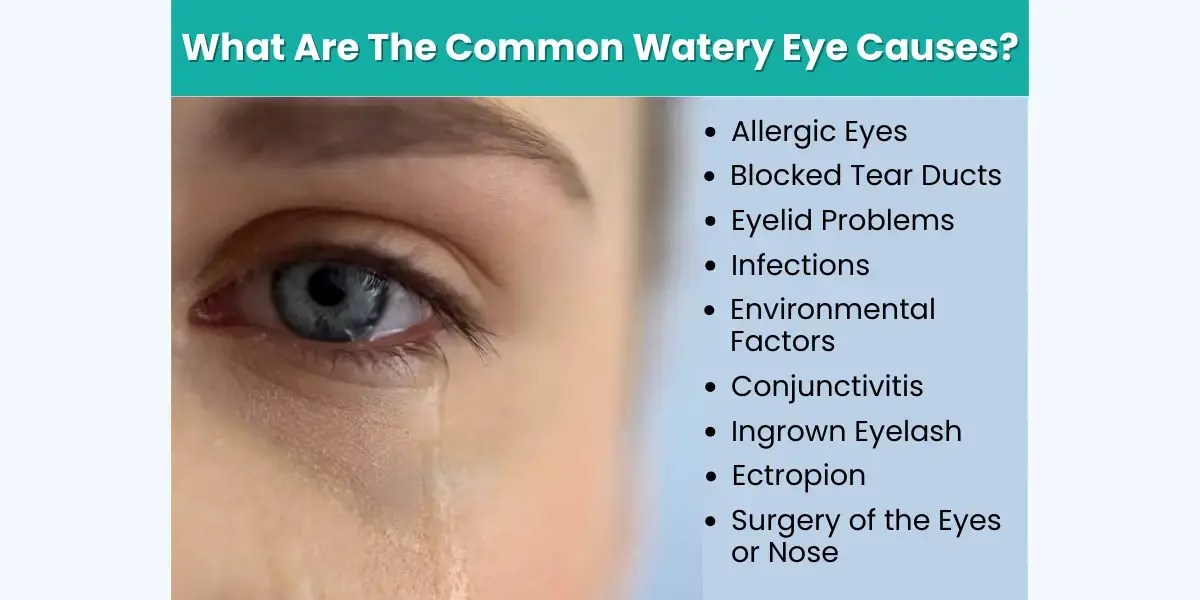
Dry eye disease is a common condition characterized by insufficient tear production or excessive tear evaporation. This can lead to discomfort, blurry vision, and even damage to the eyes if left untreated. The causes can range from environmental factors to underlying medical conditions, making a proper diagnosis essential for effective treatment. Understanding the different types of dry eye and the potential long-term consequences of untreated disease is critical for choosing the right treatment.
Introduction to Dry Eye
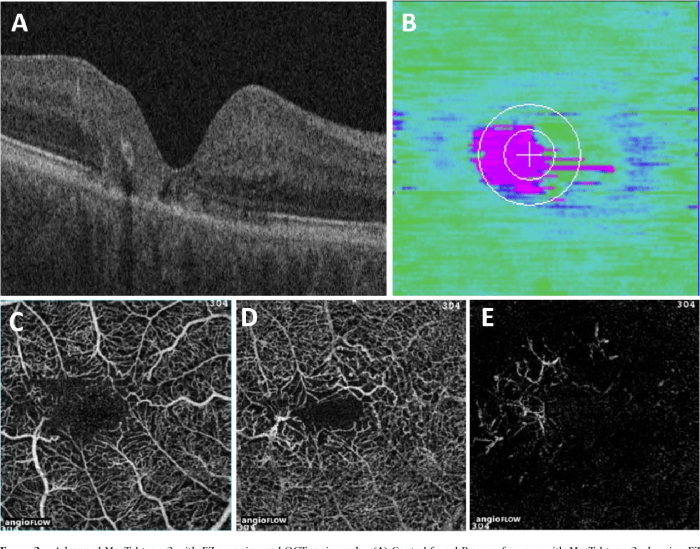
Dry eye disease is a common condition affecting millions worldwide. It occurs when the tear film, the protective layer on the surface of the eye, is insufficient or unstable. This leads to discomfort, irritation, and potentially vision problems. Understanding the different types and causes of dry eye is crucial for proper diagnosis and effective treatment.The tear film, a crucial component of eye health, is composed of three layers: an oily outer layer, a watery middle layer, and a mucous inner layer.
Proper lubrication and tear production are essential for maintaining the health of the cornea and conjunctiva, the outermost layers of the eye. Dry eye arises when any of these layers are disrupted, leading to insufficient moisture and protection for the eye.
Causes of Dry Eye
Several factors contribute to dry eye development. Age-related changes in tear production are a significant factor. Medical conditions like diabetes, rheumatoid arthritis, and Sjögren’s syndrome can also increase the risk of dry eye. Certain medications, such as antihistamines and antidepressants, can have a drying effect on the eyes. Lifestyle factors, such as prolonged screen time, air conditioning, and exposure to wind and dry air, play a significant role.
Additionally, environmental factors such as low humidity or exposure to pollutants can contribute to dry eye symptoms.
Deciding between Xiidra and Restasis for dry eye can be tough. It’s a personal choice, really, but considering the potential side effects is key. Interestingly, some of the hormonal factors involved in dry eye are similar to those in the the cortisol weight loss controversy , which highlights the complex interplay of hormones and their effects on the body.
Ultimately, the best course of action is to discuss your specific needs and concerns with an eye doctor to determine the most suitable treatment for you.
Types of Dry Eye
Dry eye can be broadly categorized into two primary types: aqueous deficient and evaporative dry eye. Aqueous deficient dry eye is characterized by reduced production of the watery component of the tear film. In contrast, evaporative dry eye results from the rapid evaporation of the oily component of the tear film, often due to factors like meibomian gland dysfunction (MGD).
MGD involves the malfunctioning of tiny oil-producing glands in the eyelids, leading to insufficient lubrication of the tear film. The specific type of dry eye impacts the choice of treatment.
Symptoms of Dry Eye
Common symptoms of dry eye include a gritty or sandy feeling in the eyes, redness, burning, and itching. Blurred vision, particularly after prolonged periods of reading or computer use, is also a frequent complaint. These symptoms can vary in severity, from mild discomfort to significant impairment of vision. Proper diagnosis is essential to identify the underlying cause and select the most appropriate treatment.
Importance of Proper Diagnosis
Accurate diagnosis is critical in selecting the appropriate treatment for dry eye. Symptoms can mimic other eye conditions, and a comprehensive evaluation by an ophthalmologist is essential to determine the precise type of dry eye. This evaluation often involves examining the tear film, assessing eyelid health, and conducting other diagnostic tests to identify the underlying cause. This approach ensures the most effective and tailored treatment plan.
Environmental Factors in Dry Eye
Environmental factors can significantly impact dry eye development. Exposure to dry air, such as in air-conditioned environments or during winter months, can lead to increased tear evaporation. Prolonged exposure to wind or smoke can also exacerbate dry eye symptoms. Furthermore, factors like low humidity in the home or workplace can contribute to dryness. These factors often interact with other conditions to increase the likelihood of developing dry eye.
Long-Term Consequences of Untreated Dry Eye, Should i take xiidra or restasis to treat dry eye
Untreated dry eye can have serious long-term consequences. Chronic dryness can lead to corneal damage, resulting in corneal erosions, ulcers, and scarring. These complications can significantly impair vision and require further intervention. In some cases, untreated dry eye can also lead to increased susceptibility to infections and potentially vision loss.
Comparing Xiidra and Restasis
Choosing between Xiidra and Restasis for dry eye treatment can be overwhelming. Both medications aim to improve tear production, but their mechanisms of action, side effects, and costs differ. Understanding these nuances will help you make an informed decision with your doctor.
Mechanisms of Action
Xiidra and Restasis work through distinct pathways to increase tear production. Xiidra, a topical ophthalmic solution, inhibits the enzyme cyclooxygenase-2 (COX-2), which plays a role in inflammation and tear production. This inhibition leads to a reduction in inflammation and a possible improvement in tear production. Restasis, also a topical ophthalmic solution, is a different approach. It increases the production of the enzyme responsible for creating the proteins that make up healthy tears.
Restasis works by stimulating the meibomian glands, which produce the oily component of tears, improving the stability of the tear film.
Key Ingredients and Their Effects
Xiidra’s active ingredient is lifitegrast. Lifitegrast’s action on COX-2 is crucial in reducing inflammation, a key contributor to dry eye symptoms. Restasis, on the other hand, contains the active ingredient, cyclosporine A. Cyclosporine A is an immunomodulator that helps reduce inflammation and promote the production of healthy tears.
Potential Side Effects
Both medications can cause side effects, although they are generally well-tolerated. Common side effects of Xiidra include mild eye irritation, such as burning, stinging, or redness. These symptoms are usually temporary and resolve with continued use. Restasis, while often well-tolerated, may cause more frequent or severe stinging, burning, or redness. Some individuals experience blurry vision or a foreign body sensation.
It’s important to note that individual responses vary.
Dosage and Administration
The dosage and administration of Xiidra and Restasis differ. Xiidra is typically administered once daily, usually in the morning. Restasis, however, requires a longer treatment period with a dosage typically twice daily for several months. Following the prescribed dosage and administration instructions is crucial for optimal results.
Comparison Table
| Feature | Xiidra | Restasis | Comparison |
|---|---|---|---|
| Mechanism of Action | Inhibits COX-2, reducing inflammation | Stimulates tear production proteins, promoting tear stability | Xiidra focuses on inflammation, Restasis on tear production. |
| Side Effects | Mild eye irritation (burning, stinging, redness) | Frequent or severe stinging, burning, redness, blurry vision | Xiidra tends to have milder side effects, though individual responses vary. |
| Cost | Generally more expensive | Potentially less expensive initially, but the longer treatment period can increase the overall cost. | Cost varies by insurance coverage and pharmacy. |
| Duration of Treatment | Usually, results are seen within a few weeks; continuous treatment is often necessary. | Treatment can take several months to show significant improvement, often with continuous treatment. | Long-term use is often necessary for both. |
Patient Considerations: Should I Take Xiidra Or Restasis To Treat Dry Eye
Choosing between Xiidra and Restasis for dry eye treatment involves careful consideration of individual patient factors. A thorough understanding of these factors can help patients and their eye care professionals make the most informed decision regarding their specific needs. Ultimately, the best choice depends on a combination of the medication’s potential benefits, potential side effects, and the patient’s overall health profile.Patient responses to medications can vary significantly.
What works well for one person might not be as effective or even well-tolerated by another. This is why a personalized approach to treatment is crucial. Open communication with your eye care professional is key to navigating this process.
Age
Age can influence the choice between Xiidra and Restasis. Younger patients might respond well to both medications, but potential long-term usage needs to be considered. Older patients might experience different side effects or have other health concerns that may affect the treatment choice. For example, older patients might have a higher risk of developing certain side effects from certain medications, so careful monitoring and consideration of alternative options may be necessary.
Underlying Conditions
Certain underlying health conditions can impact the efficacy and safety of both Xiidra and Restasis. Conditions such as autoimmune diseases, certain allergies, or other chronic medical issues might necessitate a different approach to dry eye treatment. For example, patients with a history of kidney or liver disease may require careful monitoring when using Xiidra or Restasis due to potential interactions.
Medication History
A comprehensive medication history is crucial when deciding between Xiidra and Restasis. Interactions with other medications can alter how these dry eye treatments function or cause adverse side effects. For instance, patients taking certain blood thinners may need to be monitored more closely when using Restasis, due to a potential increased risk of bleeding. Similarly, patients on medications that affect the liver or kidneys may need to have their dosage adjusted when using Xiidra.
Deciding between Xiidra and Restasis for dry eye can be tricky. While I’m not a medical professional, I’ve been researching the latest treatments, and a fascinating new trial for breast cancer treatment, the enhertu breast cancer treatment trial , is showing promising results. Ultimately, the best course of action for dry eye depends on individual needs and, of course, what your doctor recommends.
So, what are your thoughts on the best way to approach dry eye?
Individual Patient Responses
Individual patient responses to medications are significant factors to consider. Some patients may experience rapid improvements with one medication, while others might require a longer period of treatment or even a different approach. This variation highlights the need for a personalized approach to treatment and regular monitoring of response.
Potential Interactions
Interactions with other medications or health conditions are possible with both Xiidra and Restasis. Therefore, full disclosure of all medications, supplements, and existing medical conditions is essential. This ensures the eye care professional can make an informed decision regarding the most appropriate treatment plan, minimizing potential adverse interactions.
| Patient Factor | Description | Impact on Treatment Choice |
|---|---|---|
| Age | Patient’s chronological age. | Younger patients may tolerate both medications well, while older patients may require careful consideration of potential side effects or interactions with other medications. |
| Underlying Conditions | Pre-existing medical conditions, such as autoimmune diseases, allergies, or chronic health issues. | Certain conditions might necessitate a different treatment approach due to potential interactions or reduced efficacy. |
| Medication History | List of current medications, including prescription drugs, over-the-counter medications, and supplements. | Potential interactions between Xiidra or Restasis and other medications should be carefully evaluated to prevent adverse effects. |
Lifestyle and Environmental Considerations
Dry eye isn’t just about the medications you take; your daily habits and surroundings play a significant role. Understanding how lifestyle choices and environmental factors affect your eyes can help you take proactive steps to manage your dry eye symptoms effectively. This section explores the influence of lifestyle and environment on dry eye, offering practical preventative measures and recommendations for overall eye health.Lifestyle and environmental factors can significantly impact tear production and quality, contributing to dry eye symptoms.
Factors like stress, diet, and even the type of work you do can influence the health of your tear film. By understanding these influences, you can make informed decisions about your daily habits and surroundings to support your eye health.
Deciding between Xiidra and Restasis for dry eye can be tough. While I’m no doctor, I’ve been researching the different treatments and the potential long-term effects. Interestingly, the human body’s ability to endure without food is a fascinating area of study, though completely unrelated to dry eye treatments. To learn more about how long humans can survive without food, check out this fascinating article: how long live without food.
Ultimately, the best course of action for dry eye is to consult an eye doctor who can properly assess your specific situation and recommend the most suitable option.
Impact of Lifestyle Choices on Dry Eye
Lifestyle choices, such as diet and stress levels, can directly affect the health of your eyes and the production of tears. A diet deficient in essential nutrients, like omega-3 fatty acids, can compromise tear film stability. Chronic stress can disrupt the body’s hormonal balance, which can also impact tear production. Lack of sleep can further exacerbate these issues, contributing to dry eye symptoms.
Environmental Factors Aggravating Dry Eye
Certain environmental conditions can trigger or worsen dry eye symptoms. Dry air, often found in heated or air-conditioned environments, can evaporate tears more quickly, leading to discomfort. Prolonged screen time, common in today’s digital world, can also strain the eyes and reduce tear production. Exposure to smoke, pollutants, and harsh chemicals can further irritate the delicate eye surface, aggravating dry eye.
Preventative Measures and Recommendations
Several preventative measures can mitigate the risk of dry eye and improve overall eye health. Maintaining a balanced diet rich in essential nutrients, including omega-3 fatty acids, is crucial for tear film health. Prioritizing adequate sleep and managing stress through relaxation techniques can also help regulate tear production. Limiting screen time and taking regular breaks during extended computer use can significantly reduce eye strain.
Lifestyle Tips for Managing Dry Eye
Implementing these lifestyle tips can help you manage dry eye symptoms effectively:
- Hydration: Drinking plenty of water throughout the day is essential for overall health, including eye health. Adequate hydration helps maintain the volume and quality of tears.
- Balanced Diet: A diet rich in omega-3 fatty acids, found in fatty fish like salmon and flaxseeds, can enhance tear film stability. Include plenty of fruits, vegetables, and healthy fats in your diet.
- Stress Management: Chronic stress can negatively impact tear production. Incorporate stress-reducing activities like yoga, meditation, or spending time in nature into your routine.
- Environmental Control: In dry climates or during cold months, use a humidifier to add moisture to the air. This can help prevent tear evaporation.
- Screen Breaks: When using electronic devices, take frequent breaks to rest your eyes. The 20-20-20 rule (look at something 20 feet away for 20 seconds every 20 minutes) can be helpful.
- Protective Measures: Wear sunglasses to protect your eyes from harsh sunlight, wind, and dust. This can help prevent further irritation.
- Regular Eye Exams: Regular checkups with an ophthalmologist are crucial for early detection and management of dry eye. Discuss your lifestyle and environmental factors with your eye doctor to develop a personalized strategy.
When to Consult an Eye Care Professional
Dry eye, while often manageable with over-the-counter remedies and lifestyle changes, can sometimes signal underlying health issues. Understanding when to seek professional medical advice is crucial for timely diagnosis and effective treatment. Proactive consultation can prevent complications and ensure the best possible outcome.
Crucial Situations Requiring Professional Advice
Ignoring dry eye symptoms can sometimes lead to more serious issues. Certain conditions and symptoms warrant immediate consultation with an eye care professional. These include:
- Persistent or worsening dry eye symptoms despite home remedies and over-the-counter treatments.
- Sudden onset of severe pain, redness, or swelling in the eye.
- Changes in vision, such as blurry vision or halos around lights.
- Sensitivity to light (photophobia).
- Discharge from the eye, especially if accompanied by pain or redness.
- Eye pain that doesn’t subside with over-the-counter pain relievers.
- Eyelid abnormalities, such as crusting, redness, or swelling.
- History of autoimmune diseases, such as rheumatoid arthritis or lupus.
- Use of certain medications known to cause dry eye as a side effect.
When to Seek Immediate Medical Attention
Certain symptoms demand immediate attention. If you experience any of the following, seek emergency medical care:
- Severe eye pain that prevents you from opening your eye.
- Sudden vision loss or significant changes in vision.
- Severe eye injury, such as a chemical burn or penetrating injury.
- A foreign object lodged in the eye.
- Signs of infection, such as pus or a yellowish discharge.
Importance of Regular Eye Exams
Regular eye exams, even for individuals without apparent dry eye symptoms, are vital for overall eye health. These exams allow early detection of potential problems, including early stages of dry eye. Early detection enables timely intervention and prevents further complications. Comprehensive eye exams can also identify other underlying health conditions.
What to Expect During a Consultation
During a consultation with an ophthalmologist or optometrist, expect a thorough evaluation. This typically involves:
- A detailed discussion of your symptoms, including their duration, frequency, and severity.
- A comprehensive eye examination, including assessments of tear production, surface health, and vision.
- Discussion of your medical history and current medications.
- Potential diagnostic tests, such as tear film analysis or fluorescein staining.
- Development of a personalized treatment plan, if necessary.
Flowchart for Seeking Medical Advice
This flowchart provides a visual guide to help determine when to seek medical attention for dry eye symptoms.
| Symptom/Situation | Action |
|---|---|
| Mild dry eye symptoms; home remedies ineffective | Consult an eye care professional |
| Sudden onset of severe pain, redness, or swelling | Consult an eye care professional immediately |
| Significant changes in vision, such as blurry vision or halos | Consult an eye care professional immediately |
| Severe eye pain preventing eye opening | Seek emergency medical care |
| Severe eye injury or foreign object | Seek emergency medical care |
| Signs of infection (pus, yellow discharge) | Seek emergency medical care |
Alternative Treatments for Dry Eye

Beyond prescription medications, several alternative and complementary therapies can help manage dry eye symptoms. These approaches often focus on supporting the eyes’ natural lubrication and addressing underlying factors contributing to dryness. Lifestyle adjustments, combined with these techniques, can significantly improve comfort and quality of life for those experiencing dry eye.
Lifestyle and Environmental Adjustments
Maintaining a healthy lifestyle plays a crucial role in managing dry eye. Adequate hydration is paramount, as proper fluid intake helps the body produce tears. Reducing stress through relaxation techniques can also positively impact tear production. Environmental factors like air conditioning and excessive screen time can exacerbate dry eye. Minimizing these factors and utilizing appropriate humidifiers or eye protection can be beneficial.
Over-the-Counter Remedies
Many over-the-counter remedies can offer temporary relief from dry eye symptoms. These include lubricating eye drops, often containing hyaluronic acid, which helps to create a protective layer over the eye surface. Other options include artificial tears, which are designed to mimic natural tears and provide moisture. These products are generally safe for daily use and are readily available without a prescription.
Lubricating Eye Drops: Artificial Tears
Lubricating eye drops, often called artificial tears, are a cornerstone of dry eye management. These drops are formulated to mimic the natural components of tears, providing moisture and comfort. Different formulations contain varying ingredients, including hyaluronic acid, polymers, and other moisturizing agents. The effectiveness of artificial tears can vary from person to person, depending on the specific formulation and individual needs.
Proper use, typically several times a day as needed, is key to maximizing their benefits. The most effective artificial tears often include preservatives to help maintain sterility and prevent microbial growth, although some people may experience sensitivity to these preservatives. Selecting a preservative-free option can be beneficial for those with sensitivities. Regular use of artificial tears is often recommended for maintaining eye moisture and comfort throughout the day.
Complementary Therapies
Certain complementary therapies, while not a replacement for conventional medical care, may provide additional support in managing dry eye symptoms. These therapies include warm compresses, which can help improve blood flow to the eye area and promote tear production. Additionally, incorporating healthy eating habits, rich in omega-3 fatty acids, can potentially contribute to healthier tear production. Proper eyelid hygiene, like gentle cleansing and massage, can also help maintain the delicate balance of the tear film.
However, it’s crucial to note that these complementary approaches should not be considered a substitute for medical advice or treatment plans provided by an eye care professional.
Final Summary
Ultimately, deciding between Xiidra and Restasis for dry eye treatment requires careful consideration of individual needs and preferences. Factors like cost, potential side effects, and your personal response to the medication play a crucial role. Consulting with an eye care professional is essential for a personalized diagnosis and treatment plan. Remember that lifestyle choices and environmental factors also contribute significantly to managing dry eye symptoms.
By understanding the complexities of this condition and actively participating in your eye health management, you can take control of your dry eye experience and improve your overall eye health.