Diabetes nutrition and weight loss is a crucial aspect of managing this condition effectively. Understanding the connection between food choices, portion sizes, and activity levels is key to achieving and maintaining a healthy weight while controlling blood sugar. This guide delves into balanced nutrition plans, effective weight loss strategies, and considerations for diverse populations, all designed to help you navigate the complexities of diabetes management.
We’ll explore the role of macronutrients, micronutrients, and the glycemic index in controlling blood sugar. Different dietary approaches will be compared, and practical tips for grocery shopping, meal preparation, and managing blood sugar fluctuations will be shared. Furthermore, we’ll address the unique nutritional needs of specific populations, such as pregnant women, children, and the elderly. Don’t miss the essential information on the role of supplements and medications, along with the importance of consulting healthcare professionals.
Diabetes Management through Nutrition: Diabetes Nutrition And Weight Loss
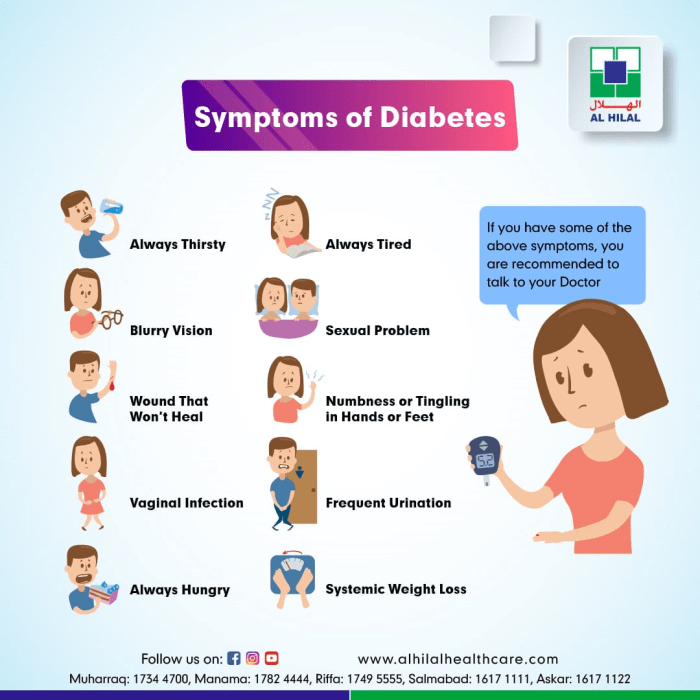
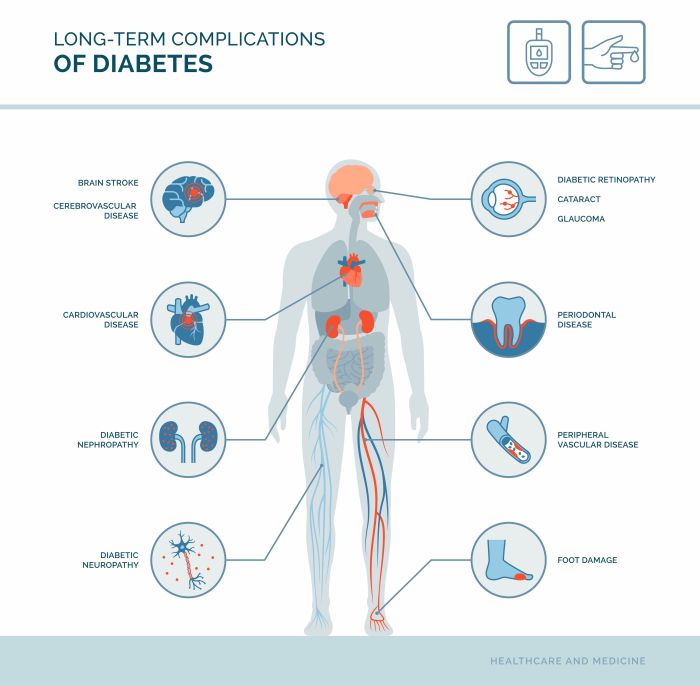
Proper nutrition plays a crucial role in managing diabetes, enabling individuals to effectively control their blood sugar levels and improve overall well-being. A well-planned diet that considers the balance of macronutrients and micronutrients is essential for optimal health and preventing long-term complications associated with the disease. This approach not only aids in blood sugar control but also supports weight management, a critical factor in diabetes management.
Importance of Balanced Nutrition
A balanced diet for diabetes management is characterized by a variety of nutrient-rich foods, portion control, and mindful eating habits. This approach ensures adequate intake of essential nutrients while minimizing the impact on blood sugar levels. By carefully selecting foods and controlling portion sizes, individuals can maintain stable blood glucose levels and promote overall health.
Macronutrients and Blood Sugar Control
Macronutrients, including carbohydrates, proteins, and fats, significantly influence blood sugar levels. Understanding their impact is crucial for creating an effective meal plan. Carbohydrates are the primary source of energy and directly affect blood sugar. Proteins help regulate blood sugar by slowing down the absorption of carbohydrates. Healthy fats, such as those found in avocados and nuts, can also contribute to stable blood sugar levels and overall health.
Micronutrients for Overall Health
Micronutrients, including vitamins and minerals, are essential for maintaining optimal health in individuals with diabetes. Vitamins and minerals support various bodily functions, including the immune system and energy production. A diet rich in fruits, vegetables, and whole grains ensures an adequate intake of these vital micronutrients.
Healthy Meal Plans for Diabetes
Creating healthy meal plans tailored to individual needs is essential for effective diabetes management. These plans should consider factors such as blood sugar targets, personal preferences, and dietary restrictions. Meal planning tools and resources can assist individuals in developing customized plans. Consulting a registered dietitian is highly recommended for personalized guidance and support.
Sample Weekly Meal Plan (Type 2 Diabetes)
This sample weekly meal plan provides a framework for managing type 2 diabetes. Portion sizes are estimations and should be adjusted based on individual needs and activity levels. It’s vital to monitor blood sugar levels and adjust the plan accordingly.
- Monday: Breakfast (Oatmeal with berries and nuts – 1/2 cup, 1/4 cup berries, 1/4 cup nuts); Lunch (Grilled chicken salad with mixed greens and vegetables – 4 oz chicken, 2 cups greens, 1 cup vegetables); Dinner (Baked salmon with roasted vegetables – 4 oz salmon, 1.5 cups vegetables)
- Tuesday: Breakfast (Greek yogurt with fruit and granola – 1 cup yogurt, 1/2 cup fruit, 1/4 cup granola); Lunch (Lentil soup with whole-wheat bread – 1.5 cups soup, 1 slice bread); Dinner (Lean beef stir-fry with brown rice – 4 oz beef, 1/2 cup stir-fry, 1/2 cup brown rice)
- Wednesday: Breakfast (Whole-wheat toast with avocado and egg – 2 slices toast, 1/4 avocado, 1 egg); Lunch (Turkey and avocado sandwich on whole-wheat bread – 3 oz turkey, 1/2 avocado, 2 slices bread); Dinner (Chicken breast with quinoa and steamed broccoli – 4 oz chicken, 1/2 cup quinoa, 1 cup broccoli)
- Thursday – Sunday: Similar meal combinations using a variety of protein sources, vegetables, and whole grains. Portion sizes should be adjusted based on individual needs.
Glycemic Index and its Impact
The glycemic index (GI) measures how quickly a carbohydrate-containing food raises blood sugar levels. Foods with a high GI cause a rapid increase in blood sugar, while those with a low GI have a more gradual effect. Understanding the GI of foods helps in choosing options that promote stable blood sugar control.
Dietary Approaches for Diabetes Management
Various dietary approaches can be effective in managing diabetes. The Mediterranean diet, emphasizing fruits, vegetables, whole grains, and healthy fats, is often recommended. A low-carbohydrate diet focuses on reducing carbohydrate intake to manage blood sugar levels. Choosing the most suitable approach depends on individual preferences and health conditions.
Glycemic Index Table
| Food | Glycemic Index |
|---|---|
| White bread | 70 |
| White rice | 70 |
| Potatoes (baked) | 75 |
| Corn flakes | 80 |
| Sweet potatoes | 60 |
| Oatmeal | 55 |
| Apples | 30 |
| Broccoli | 15 |
Weight Loss Strategies for Individuals with Diabetes

Maintaining a healthy weight is crucial for managing diabetes effectively. Excess weight, particularly around the abdomen, can significantly impact blood sugar control and increase the risk of diabetes-related complications. Weight loss, even modest amounts, can dramatically improve insulin sensitivity, lower blood glucose levels, and reduce the risk of heart disease, stroke, and nerve damage. This section explores effective and safe weight loss strategies tailored for individuals with diabetes.
Relationship Between Weight Management and Diabetes Control
Weight management plays a pivotal role in controlling blood sugar levels in individuals with diabetes. Excess weight, especially abdominal fat, often leads to insulin resistance. This means the body’s cells don’t respond properly to insulin, hindering the uptake of glucose from the bloodstream. Consequently, blood sugar levels rise, increasing the risk of complications. Weight loss, by improving insulin sensitivity, allows the body to utilize insulin more effectively, thus regulating blood glucose levels.
Studies consistently demonstrate that even modest weight loss can lead to significant improvements in blood glucose control and reduce the need for medication.
Diabetes nutrition and weight loss are crucial for overall health, but what about other conditions impacting exercise tolerance? Sometimes, seemingly unrelated issues like seid systemic exertion intolerance disease can significantly affect your ability to manage your weight and blood sugar. Even with a carefully planned diet, overcoming physical limitations can make achieving optimal diabetes nutrition goals more challenging.
Finding ways to adapt your nutrition and exercise routine for such conditions is key to maintaining good health.
Potential Benefits of Weight Loss for Improving Blood Sugar Levels and Reducing Complications
Weight loss can significantly improve blood sugar control and reduce the risk of diabetes-related complications. By reducing insulin resistance, weight loss allows the body to utilize insulin more effectively. This often leads to a decrease in blood glucose levels, which in turn lowers the risk of complications such as heart disease, stroke, nerve damage, kidney disease, and eye problems.
Furthermore, weight loss can also improve blood pressure and cholesterol levels, further reducing the risk of cardiovascular issues. A study published in the
New England Journal of Medicine* reported that a 5-10% weight loss in individuals with type 2 diabetes led to substantial improvements in blood glucose control and cardiovascular risk factors.
Safe and Effective Weight Loss Strategies for Individuals with Diabetes
Safe and effective weight loss strategies for individuals with diabetes emphasize a balanced approach encompassing diet, exercise, and behavioral modifications. These strategies should be personalized and tailored to individual needs and preferences. Crucially, individuals should consult with their healthcare provider or a registered dietitian to create a safe and effective plan. Rapid weight loss is generally not recommended as it can be detrimental to health.
Exercises That Promote Weight Loss and Support Overall Health
Regular physical activity is essential for weight loss and overall health. Exercise increases calorie expenditure, boosts metabolism, and improves insulin sensitivity. A combination of cardiovascular exercises and strength training is recommended. Examples of effective exercises include brisk walking, jogging, swimming, cycling, and strength training exercises using weights or resistance bands. Consistency is key, aiming for at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic activity per week, along with strength training exercises twice a week.
Importance of Regular Physical Activity in Conjunction with Dietary Changes
Dietary changes alone are often insufficient for sustainable weight loss. Combining dietary changes with regular physical activity maximizes weight loss effectiveness and overall health benefits. Exercise strengthens muscles, improves metabolism, and enhances the body’s ability to burn calories. This synergistic effect of dietary changes and regular exercise leads to greater improvements in blood sugar control and long-term weight management.
Furthermore, exercise improves mood, reduces stress, and promotes overall well-being, crucial factors for sustained weight loss.
Comparison of Weight Loss Approaches
| Weight Loss Approach | Description | Suitability for People with Diabetes |
|---|---|---|
| Diet | Focuses on reducing calorie intake and modifying dietary patterns to meet individual needs. | Crucial for managing blood sugar and reducing calorie surplus. |
| Exercise | Incorporates physical activity into daily routine to increase calorie expenditure and improve overall health. | Essential for improving insulin sensitivity and blood sugar control. |
| Surgery | Bariatric surgery, for example, can result in significant weight loss and improve metabolic conditions. | Considered for individuals with severe obesity and uncontrolled diabetes. |
Comparison and Contrast of Different Weight Loss Strategies
Different weight loss strategies offer varying degrees of effectiveness and suitability for individuals with diabetes. Dietary approaches, including low-calorie diets, Mediterranean diets, and low-carbohydrate diets, can help manage calorie intake and improve blood sugar control. Exercise programs, including cardiovascular and strength training, enhance calorie expenditure and improve insulin sensitivity. Bariatric surgery may be an option for individuals with severe obesity and uncontrolled diabetes.
Diabetes nutrition and weight loss often involve careful meal planning. Adding certain superfoods can significantly help, like sea buckthorn, which is packed with antioxidants and vitamins. The benefits of sea buckthorn can support a healthy gut and potentially improve blood sugar control, making it a great addition to a diabetes-friendly diet. Ultimately, a balanced approach combining good nutrition and regular exercise is key to managing diabetes and weight loss goals.
The best approach is individualized and depends on factors like current health status, lifestyle preferences, and severity of diabetes.
Use of a Food Journal in Tracking Dietary Intake for Weight Management
A food journal is a valuable tool for tracking dietary intake and monitoring progress toward weight loss goals. It allows individuals to become more aware of their eating habits and identify patterns that may be contributing to weight gain or hindering weight loss efforts. By meticulously recording everything eaten and the corresponding calorie count, individuals can identify areas where they might need to adjust their dietary intake.
Detailed dietary records allow for greater personalization of dietary plans and monitoring of their effectiveness.
Nutritional Considerations for Specific Populations
Managing diabetes requires a personalized approach, recognizing that nutritional needs vary based on factors like age, life stage, and co-existing health conditions. This section delves into specific nutritional considerations for different populations living with diabetes, ensuring a tailored and effective dietary strategy.Understanding the unique nutritional needs of various populations is crucial for successful diabetes management. A personalized approach to nutrition, taking into account individual circumstances, ensures optimal health outcomes.
Looking to manage diabetes and shed some pounds? Good nutrition is key, but incorporating exercise is just as important. A great way to add strength training to your routine is using resistance bands. Learning how to use resistance bands effectively can be a game-changer for your overall fitness, and in turn, your diabetes management. Check out this helpful guide on how to use resistance bands for some tips and tricks.
By focusing on both healthy eating and targeted exercises like those achievable with resistance bands, you’ll be well on your way to achieving your weight loss goals and better controlling your diabetes.
Nutritional Needs of Pregnant Women with Diabetes
Pregnant women with diabetes require careful dietary planning to support both their health and the developing fetus. A balanced diet rich in essential nutrients, while managing carbohydrate intake, is paramount. Adequate protein, fiber, vitamins, and minerals are essential for healthy fetal development and maternal well-being. Monitoring blood glucose levels and adjusting dietary intake accordingly are vital to prevent complications.
Nutritional counseling from a registered dietitian specializing in diabetes management is highly recommended during pregnancy.
Dietary Requirements for Children and Adolescents with Diabetes
Children and adolescents with diabetes need a balanced diet that supports growth and development while managing blood glucose levels. Portion control and consistent meal timing are crucial. Educating children and adolescents about healthy food choices and diabetes management is essential for long-term success. Dietary adjustments need to be made to accommodate the changing nutritional needs during growth spurts and active lifestyles.
Dietary Needs as People Age with Diabetes
Dietary needs change as individuals age. The metabolism slows, and physical activity levels often decrease. Maintaining a healthy weight, managing blood glucose levels, and addressing potential nutrient deficiencies become crucial. Calorie needs may decrease, but essential nutrients, including protein, fiber, and vitamins, remain vital. Regular consultation with a healthcare professional is recommended for tailored dietary guidance.
Diabetes-Friendly Recipes for Various Dietary Preferences
A diverse range of diabetes-friendly recipes can accommodate various dietary preferences. Examples include:
- Lean protein sources: Grilled chicken breast, fish, tofu, lentils, and beans are excellent choices for controlling blood sugar levels.
- Complex carbohydrates: Brown rice, quinoa, whole-wheat pasta, and starchy vegetables are beneficial for sustained energy.
- Healthy fats: Avocados, nuts, seeds, and olive oil contribute to overall health.
- Fruits and vegetables: A wide variety of colorful fruits and vegetables are packed with essential vitamins and minerals.
Adapting Meal Plans for Allergies or Intolerances
Modifying meal plans to accommodate specific allergies or intolerances is possible. For example, gluten-free alternatives are available for individuals with celiac disease or gluten sensitivity. Substituting ingredients or adapting recipes can easily accommodate these needs.
Nutritional Guidelines for Different Age Groups with Diabetes
| Age Group | Key Nutritional Considerations ||—|—|| Children (0-12) | Portion control, consistent meal timing, balanced macronutrients || Adolescents (13-19) | Adequate protein, calcium, and iron, managing growth spurts || Adults (20-64) | Portion control, balanced macronutrients, managing weight || Seniors (65+) | Nutrient-dense foods, adequate protein, managing calorie needs |
Modifying Recipes for Dietary Restrictions
Modifying recipes for vegetarian, vegan, or gluten-free diets is achievable. For instance, replacing meat with tofu or lentils, using gluten-free grains, and selecting suitable dairy alternatives are all viable options. Substituting ingredients and adjusting recipes are key to accommodating these dietary restrictions.
Nutritional Needs for Individuals with Diabetes and Other Health Conditions
Individuals with diabetes who also have other health conditions require a comprehensive approach to nutrition. For example, individuals with kidney disease may need to limit their protein intake. Working closely with a registered dietitian who understands both conditions is crucial for creating a safe and effective meal plan. This ensures the nutritional needs of all conditions are met.
Practical Tips and Strategies
Diabetes management through nutrition goes beyond just choosing the right foods; it involves a holistic approach to grocery shopping, meal preparation, and mindful eating. This section provides actionable strategies to effectively manage blood sugar levels and achieve lasting weight loss. By understanding these practical tips, you can take control of your diabetes journey and lead a healthier life.Effective diabetes management requires a proactive and personalized approach.
Strategies for grocery shopping, meal preparation, and mindful eating, along with careful monitoring of blood sugar responses, can significantly improve overall health and well-being.
Grocery Shopping Strategies for Diabetes Management
Proper grocery shopping is crucial for maintaining a healthy diet. Planning your meals in advance helps you avoid impulse purchases and stick to your nutrition plan. Creating a shopping list based on your meal plan and incorporating non-processed, whole foods is recommended. Prioritize fresh fruits, vegetables, lean proteins, and whole grains. Limit processed foods, sugary drinks, and excessive amounts of unhealthy fats.
Understanding portion sizes and selecting appropriate servings is equally important.
Meal Preparation Techniques for Diabetes Management
Meal preparation plays a vital role in diabetes management. Pre-planning your meals and snacks ensures you have healthy options readily available, minimizing the risk of making unhealthy choices. Batch cooking meals and prepping ingredients for the week can be helpful time-savers. Utilizing healthy cooking methods, such as baking, grilling, or steaming, helps retain nutrients and reduces added fats.
Portion control is key during meal preparation to maintain consistent blood sugar levels.
Strategies for Managing Blood Sugar Spikes and Dips
Blood sugar fluctuations can be challenging to manage. Monitoring blood sugar levels before, during, and after meals helps identify patterns and triggers. A consistent meal schedule and appropriate portion sizes contribute to more stable blood sugar levels. If blood sugar spikes occur, consider adjusting the carbohydrate intake or incorporating physical activity. If blood sugar dips occur, have a readily available snack containing protein and carbohydrates.
The Importance of Portion Control and Mindful Eating
Portion control is essential for maintaining stable blood sugar levels. Using smaller plates and measuring food portions can help control the amount of food consumed. Mindful eating involves paying attention to your body’s hunger and fullness cues. Eating slowly and savoring each bite can enhance satiety and help prevent overeating. This approach encourages a more balanced and controlled eating experience.
The Role of Hydration in Diabetes Management
Staying adequately hydrated is vital for overall health, and particularly for managing diabetes. Drinking plenty of water throughout the day helps maintain healthy blood sugar levels and supports overall metabolic function. Limit sugary drinks and focus on water, unsweetened tea, or low-sugar options.
Resources for Finding Support and Educational Materials on Diabetes Nutrition
Numerous resources are available to support your diabetes nutrition journey. Your healthcare provider can recommend reputable diabetes education programs and support groups. Online resources, such as websites and apps, offer valuable information and tools. Connecting with other individuals managing diabetes can provide emotional support and practical advice.
Common Food Triggers for Blood Sugar Fluctuations
| Food Category | Common Examples | Potential Impact ||—|—|—|| Sugary Drinks | Soda, Juice, Sweetened Tea | Significant blood sugar spikes || Processed Foods | White Bread, Pastries, Fast Food | Rapid increase in blood sugar || Refined Carbohydrates | White Rice, White Pasta, Bagels | Blood sugar spikes || High-Fat Foods | Fried Foods, Fatty Meats | Can impact blood sugar levels, but often less dramatic than simple carbs |
Reading Food Labels Effectively for Diabetes Management
Understanding food labels is crucial for making informed choices. Pay close attention to serving sizes, carbohydrate content, and added sugars. Choose foods with lower sugar and refined carbohydrate content. Reading labels enables you to make appropriate dietary choices.
Mindful Eating and its Role in Managing Blood Sugar Levels
Mindful eating involves paying attention to your body’s internal cues related to hunger and fullness. This approach encourages a more balanced and controlled eating experience. Eating slowly and savoring each bite can enhance satiety and prevent overeating. Being present during meals, without distractions, can improve your understanding of your body’s hunger and fullness signals. This awareness allows you to make informed choices that support healthy blood sugar levels.
Dietary Supplements and Medications
Navigating the world of diabetes management can feel overwhelming. Understanding the potential benefits and risks of dietary supplements, alongside the role of medications, is crucial for effective self-care. This section explores these critical components, emphasizing the importance of professional guidance and responsible use.Dietary supplements, while sometimes touted as miracle cures, are not a substitute for a balanced diet and regular exercise.
Many claim to improve blood sugar control, but their effectiveness varies significantly. Some supplements might have beneficial effects, while others could interact negatively with diabetes medications, potentially leading to adverse health consequences.
Potential Benefits and Risks of Dietary Supplements
Dietary supplements are products intended to supplement a person’s diet. They may contain vitamins, minerals, herbs, or other substances. While some supplements might offer potential benefits for managing diabetes, such as improving insulin sensitivity or reducing inflammation, it’s important to approach them cautiously. Potential risks include interactions with medications, insufficient scientific evidence for their effectiveness, and even potential toxicity in high doses.
Always consult a healthcare professional before adding any supplements to your routine.
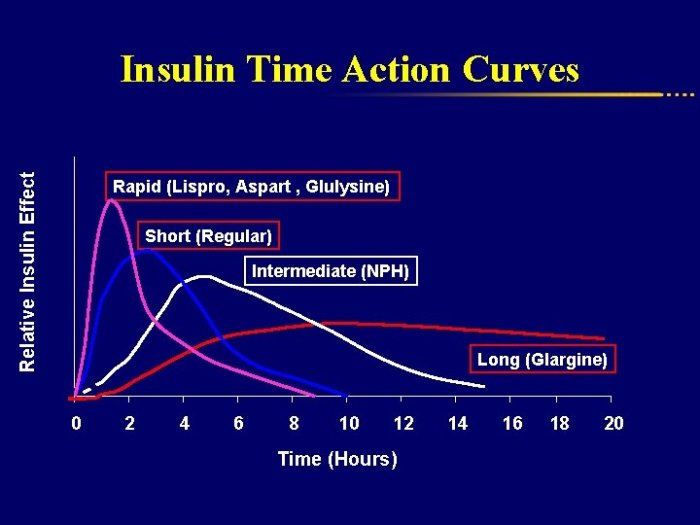
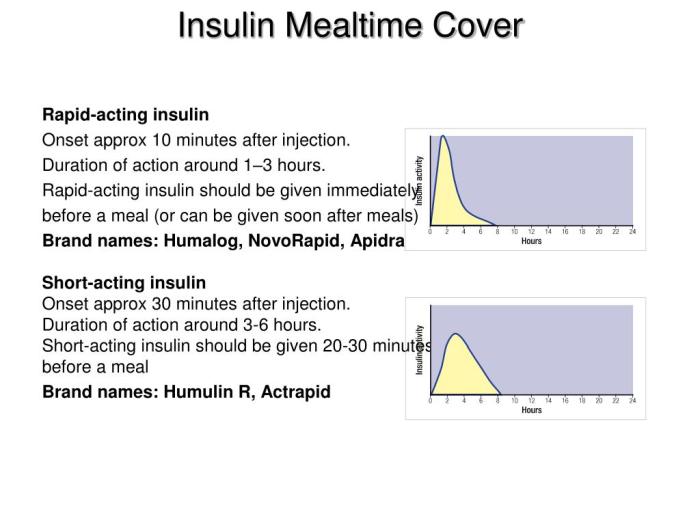
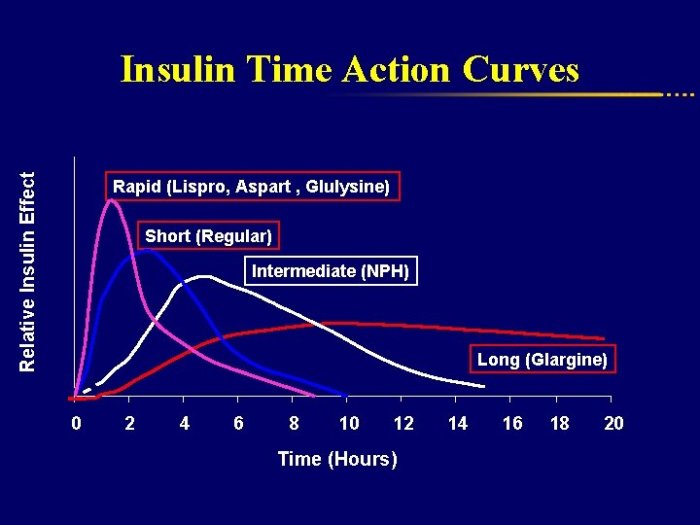
Role of Medications in Conjunction with Nutritional Interventions
Medications are an integral part of diabetes management for many individuals. They work in conjunction with nutritional interventions, such as dietary changes and exercise, to control blood sugar levels. Medications can target various aspects of glucose metabolism, helping to lower blood sugar and reduce the risk of long-term complications. Different medications have different mechanisms of action and side effects, making personalized approaches crucial.
Potential Interactions Between Dietary Supplements and Diabetes Medications
Some dietary supplements can interact with diabetes medications, potentially altering their effectiveness or increasing the risk of side effects. For example, chromium supplements may enhance the effects of some oral diabetes medications, but this interaction needs careful monitoring by a healthcare professional. Conversely, certain herbal supplements might interfere with blood sugar control medications, leading to unexpected fluctuations.
Comparison of Diabetes Medications and Their Impact on Diet and Weight
Different diabetes medications affect individuals differently in terms of diet and weight. Some medications can promote weight gain, while others might help with weight loss or have a neutral impact. For instance, insulin therapy, in some cases, can lead to weight gain if not managed with a balanced diet and exercise. Metformin, another common medication, often does not cause weight gain and may even contribute to modest weight loss.
The choice of medication often considers individual patient needs, including current health conditions, and lifestyle preferences. This personalized approach ensures the medication aligns with the overall diabetes management plan.
Potential Effects of Dietary Supplements on Blood Sugar
| Dietary Supplement | Potential Effect on Blood Sugar |
|---|---|
| Cinnamon | May improve insulin sensitivity |
| Chromium | May enhance the effects of some diabetes medications |
| Gymnema Sylvestre | May inhibit the absorption of sugar |
| Alpha-lipoic acid | May improve insulin sensitivity and antioxidant properties |
| Bitter melon | May improve insulin sensitivity |
| Berberine | May improve insulin sensitivity |
| Ginger | May have modest blood sugar lowering effects |
Note
* This table provides a general overview. The actual effects of a supplement may vary depending on the individual and the specific supplement used. Consult with a healthcare professional for personalized advice.
Importance of Consulting a Healthcare Professional, Diabetes nutrition and weight loss
Before starting any new dietary supplement or changing your medication regimen, it’s essential to consult a healthcare professional. They can assess your individual needs, evaluate potential risks and benefits, and guide you towards a safe and effective approach to diabetes management. This personalized approach ensures that any supplement or medication is compatible with your overall health and diabetes management plan.
Importance of Medication Adherence and its Relation to Diabetes Management
Medication adherence, or consistently taking your prescribed medications as directed, is crucial for effective diabetes management. This consistency helps maintain stable blood sugar levels, reducing the risk of complications and improving overall well-being. Poor adherence can lead to uncontrolled blood sugar, increasing the risk of developing diabetes-related health issues.
Impact of Medications on Diet Management
Different medications impact a patient’s ability to manage their diet in varying ways. Some medications can affect appetite or cause side effects that impact eating habits. This understanding is crucial for creating a personalized diabetes management plan that accounts for medication-related influences on diet and lifestyle choices.
Final Review

In conclusion, successfully managing diabetes involves a multifaceted approach that integrates nutrition, weight management, and lifestyle choices. This comprehensive guide equips you with the knowledge and strategies to make informed decisions about your diet and overall well-being. Remember that consulting with a healthcare professional is essential for personalized advice and support. By adopting a holistic approach, you can effectively manage your diabetes and improve your quality of life.