Diagnosis and testing for her2 positive breast cancer – Diagnosis and testing for HER2-positive breast cancer is crucial for effective treatment. This comprehensive guide delves into the specifics of identifying this aggressive form of breast cancer, from understanding the role of the HER2 protein to the various diagnostic tests used. We’ll explore the nuances of immunohistochemistry (IHC) and fluorescence in situ hybridization (FISH), comparing their strengths and weaknesses.
The importance of accurate testing for personalized medicine and tailored treatment strategies will also be highlighted.
The article details the diagnostic process, outlining the steps involved in performing IHC and FISH tests. It also explains how to interpret the results, covering different HER2 status classifications and the significance of accurate testing in determining the most effective treatment approach. Further, we’ll examine factors that may impact the accuracy of the tests, such as tumor heterogeneity, and how these factors can influence the interpretation of results.
Introduction to HER2-Positive Breast Cancer
HER2-positive breast cancer is a subtype of breast cancer characterized by the overexpression or abnormal amplification of the HER2 protein. This protein plays a crucial role in cell growth and survival, and its heightened presence in these cancers leads to accelerated cell division and tumor growth. Understanding the specifics of HER2-positive breast cancer is vital for effective diagnosis and treatment.
Its prevalence, characteristics, and the various types are critical to personalized care plans.The HER2 protein, when functioning normally, helps cells grow and divide. However, in HER2-positive breast cancer, the HER2 protein is either overproduced or present in excessive amounts. This leads to uncontrolled cell growth, resulting in the formation of a tumor. This over-activation of the HER2 pathway is a key driver of the aggressive behavior of this type of cancer.
HER2 Protein’s Role in Cancer Development
The HER2 protein is part of a family of growth factor receptors. Normally, these receptors bind to growth factors, triggering signals that tell cells to grow and divide. In HER2-positive breast cancer, the HER2 protein is either overexpressed or amplified, resulting in an overabundance of these signals. This leads to excessive cell growth and division, and ultimately, tumor formation.
Types of HER2-Positive Breast Cancer and Their Distinctions
Different types of HER2-positive breast cancer may present with varied characteristics. While the fundamental mechanism (HER2 overexpression) remains consistent, the specific genetic alterations and clinical presentations can differ. This is why a precise diagnosis and understanding of the specific subtype are crucial for effective treatment.
| Cancer Type | Characteristics | Prevalence |
|---|---|---|
| HER2-Enriched Breast Cancer | This subtype demonstrates a higher HER2 expression level compared to other breast cancer subtypes, but may not meet the criteria for HER2-positive breast cancer in all cases. Often, other genetic alterations are present alongside the HER2 overexpression. | Prevalence varies; studies are ongoing to precisely determine its prevalence within the HER2-positive category. |
| HER2-Positive Breast Cancer (Traditional Definition) | This subtype exhibits a significant increase in HER2 protein expression, often exceeding a certain threshold, and frequently involves HER2 gene amplification. This category is typically defined by a specific threshold for HER2 expression and/or amplification. | Represents a substantial proportion of HER2-positive breast cancers. |
| HER2-Positive Breast Cancer with Triple-Negative Features | This type of cancer presents with the characteristics of both HER2-positive breast cancer and triple-negative breast cancer. This means the cancer cells lack the estrogen receptor, progesterone receptor, and the HER2 protein isn’t absent but might have other characteristics like triple-negative. | Prevalence is not precisely established, but it is considered a less common subtype. |
Diagnostic Tests for HER2-Positive Breast Cancer
Understanding the presence of HER2 amplification is crucial for selecting the most effective treatment plan for breast cancer. Accurate diagnosis is the first step in this process, and several tests are used to detect HER2 overexpression or amplification. These tests help determine the appropriate treatment strategies, such as targeted therapies.
Standard Diagnostic Methods for HER2 Amplification
The standard methods for detecting HER2 amplification in breast cancer samples involve immunohistochemistry (IHC) and fluorescence in situ hybridization (FISH). These techniques evaluate the expression and presence of the HER2 protein and genes, respectively.
Immunohistochemistry (IHC)
IHC is a common and relatively quick method to assess HER2 protein expression. A tissue sample is stained with an antibody that specifically binds to the HER2 protein. The intensity and distribution of the staining are then evaluated under a microscope. This method provides a visual representation of HER2 protein levels. High HER2 expression is often associated with a higher likelihood of response to targeted therapies.
Fluorescence In Situ Hybridization (FISH), Diagnosis and testing for her2 positive breast cancer
FISH is a more precise technique that directly examines the HER2 gene copy number within the cells. Fluorescent probes bind to specific regions of the HER2 gene. The number of fluorescent signals (representing HER2 gene copies) is then counted. The ratio of HER2 to reference genes is crucial in determining the presence of HER2 amplification. This allows for a more quantitative assessment of the HER2 gene status compared to IHC.
Comparison of IHC and FISH
Both IHC and FISH are used to detect HER2 amplification, but they differ in their approach and provide different levels of detail. IHC assesses protein expression, while FISH directly measures gene copy number. The choice between IHC and FISH depends on the specific situation and the resources available.
Table Comparing IHC and FISH
| Feature | IHC | FISH |
|---|---|---|
| Method | Antibody staining of HER2 protein | Fluorescent probes to HER2 gene |
| Measurement | Protein expression level (visual) | Gene copy number (quantitative) |
| Sensitivity | Moderately sensitive; may miss some cases of low-level amplification | High sensitivity; can detect low-level amplification |
| Specificity | Moderately specific; may give false-positive results in some cases | High specificity; less prone to false-positive results |
| Cost | Generally lower | Generally higher |
| Turnaround Time | Usually faster | Usually longer |
IHC and FISH play a vital role in diagnosing HER2-positive breast cancer. Understanding the strengths and weaknesses of each technique is crucial for selecting the appropriate test for individual cases.
Testing Procedures and Interpretation
Understanding how HER2-positive breast cancer is diagnosed is crucial for personalized treatment. Accurate identification of HER2 status is vital for selecting the most effective therapies and improving patient outcomes. This section delves into the specifics of the testing procedures, including the steps involved and the interpretation of the results.
Immunohistochemistry (IHC) Testing
IHC is a common initial test for HER2 status. It uses antibodies to detect the presence and amount of HER2 protein in breast cancer cells. The test analyzes tissue samples from the tumor, looking for overexpression of the HER2 protein. The staining intensity and distribution of the HER2 protein are key factors in determining the HER2 status.
Fluorescence in situ Hybridization (FISH) Testing
FISH is often used to confirm or clarify results from IHC tests, especially if the IHC results are equivocal. It examines the number of HER2 genes within the cells. FISH analyzes the number of copies of the HER2 gene in the cells, looking for amplification, which is an increase in the number of copies. This is an important distinction in determining if HER2 is amplified or not.
HER2 Status Classifications
Different HER2 status classifications exist based on the results of IHC and FISH tests. These classifications guide treatment decisions.
Getting a diagnosis for HER2-positive breast cancer often involves a battery of tests, like biopsies and genetic screenings. Understanding the various treatment options, including the different types of prescription and OTC drugs prescription and otc drugs that might be involved, is crucial for navigating this journey. Ultimately, the specific course of diagnosis and testing for HER2-positive breast cancer will vary based on individual factors.
- HER2-negative: This classification indicates that the HER2 protein is not overexpressed, and the number of copies of the HER2 gene is normal. Treatment approaches may not include targeted therapies specific to HER2.
- HER2-equivocal: This intermediate classification arises when the IHC results are unclear or inconclusive. A FISH test is usually required to confirm the status.
- HER2-positive: This classification signifies that the HER2 protein is overexpressed, and the number of copies of the HER2 gene is amplified. Treatment strategies often involve targeted therapies, such as trastuzumab, to specifically target the HER2 protein and its signaling pathways. A common example of a patient with HER2-positive breast cancer might be a 45-year-old woman who, following a biopsy, showed HER2 overexpression, prompting further testing and targeted treatment.
Significance of Accurate HER2 Testing
Accurate HER2 testing is crucial in tailoring treatment plans for HER2-positive breast cancer. Treatments that specifically target HER2, like trastuzumab, are often very effective for this subtype of cancer. In contrast, unnecessary use of these expensive treatments in patients without HER2 amplification could lead to adverse effects and cost overruns.
Navigating the diagnosis and testing for HER2-positive breast cancer can be overwhelming. One often overlooked aspect of treatment, however, is managing potential side effects like diarrhea. Fortunately, there are various over-the-counter and prescription medications available for diarrhea relief, which can significantly improve quality of life during treatment. For a comprehensive overview of these options, check out this helpful resource on diarrhea relief otc and prescription medications.
Ultimately, understanding these options can help patients better manage the entire treatment process for HER2-positive breast cancer.
Accurate HER2 testing is vital for selecting the appropriate treatment strategies.
Step-by-Step Procedure for HER2 Testing
- A tissue sample (biopsy) of the breast tumor is collected.
- The tissue sample is processed for IHC analysis. Antibodies specific to HER2 are applied to the tissue, and the staining pattern is observed under a microscope.
- The IHC results are interpreted based on staining intensity and distribution. If the results are equivocal, a FISH test is performed.
- The FISH test analyzes the number of HER2 gene copies within the cells.
- The results of both IHC and FISH tests are combined to determine the HER2 status (negative, equivocal, or positive).
Factors Affecting Test Results

Navigating the world of HER2-positive breast cancer diagnosis often involves understanding the nuances of testing. While the procedures are generally reliable, several factors can influence the accuracy and interpretation of HER2 test results. Understanding these potential variables is crucial for both patients and healthcare professionals to make informed decisions.Accurate HER2 testing is paramount in determining the most effective treatment strategy for patients with HER2-positive breast cancer.
Factors impacting the test results, such as tumor heterogeneity, processing artifacts, and technician experience, can significantly affect the interpretation of the results. These variables need careful consideration to avoid misdiagnosis and ensure appropriate treatment planning.
Tumor Heterogeneity
Tumor samples, unfortunately, aren’t always uniform. Some breast tumors display heterogeneity, meaning different areas of the same tumor may have varying levels of HER2 expression. A sample taken from one area might show different HER2 status compared to another region of the same tumor. This inherent variability in tumor structure can lead to inaccurate results if the tested area doesn’t reflect the overall HER2 status of the tumor.
For instance, a biopsy sample might show a low HER2 expression, while the rest of the tumor has a higher expression. This would result in a potentially misleading result, impacting treatment decisions.
Processing Artifacts
The way the tumor sample is handled during the testing process can introduce artifacts that affect the test results. These artifacts can include improper sample fixation, inadequate tissue preparation, or contamination during the testing procedure. Such issues can artificially elevate or lower the HER2 protein levels, thus giving a misleading result. For example, a sample exposed to excessive heat or improper fixation solutions might falsely show a high HER2 level.
Careful adherence to standardized procedures is crucial to minimize such artifacts.
Technician Experience
The skill and experience of the technician performing the HER2 test play a significant role in its accuracy. Differences in experience and training can lead to variations in the quality of the test, impacting the reliability of the results. Experienced technicians are more adept at identifying and avoiding potential artifacts during the testing procedure. This ultimately leads to more accurate and reliable test results.
Table of Factors Affecting HER2 Testing Results
| Factor | Impact on Results | Example |
|---|---|---|
| Tumor Heterogeneity | Can lead to inaccurate results if the tested area does not represent the entire tumor’s HER2 status. | A biopsy sample from a low HER2 expression area might misrepresent the overall higher HER2 expression in the tumor. |
| Processing Artifacts | Improper sample handling can introduce errors, artificially elevating or lowering HER2 protein levels. | Improper fixation solutions might falsely increase HER2 levels. |
| Technician Experience | Variations in technician training and experience can affect the quality of the test and reliability of the results. | An inexperienced technician might miss subtle indicators of HER2 overexpression, potentially leading to an incorrect diagnosis. |
Treatment Implications of HER2 Status
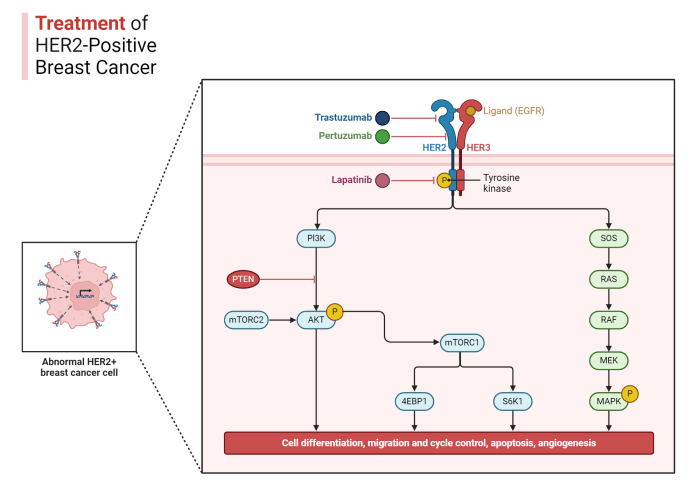
Knowing your HER2 status is crucial in determining the most effective treatment plan for breast cancer. This status significantly influences the type and intensity of therapies, impacting both short-term and long-term outcomes. The specific characteristics of HER2-positive breast cancer, driven by the presence of amplified HER2 receptors, necessitate tailored strategies that target this unique pathway.HER2-positive breast cancer, compared to other types, often requires more aggressive and targeted interventions.
Accurate HER2 testing is paramount for personalized medicine approaches, enabling physicians to select treatments that maximize efficacy and minimize side effects. The availability of targeted therapies specifically designed to inhibit the HER2 protein has revolutionized the treatment landscape for HER2-positive breast cancer patients. This approach aims to specifically block the uncontrolled growth and spread of cancer cells.
Getting a diagnosis for HER2-positive breast cancer involves a series of tests, like biopsies and genetic screenings. It’s crucial to understand these tests to make informed decisions about your treatment plan. Finding the right support is vital, and learning about complementary therapies, like costochondritis physical therapy exercises , can also be beneficial during this challenging time.
Ultimately, navigating the diagnosis and testing process requires a multi-faceted approach, focusing on both medical and supportive care.
Targeted Therapies for HER2-Positive Breast Cancer
Various targeted therapies are available to specifically target the HER2 protein, preventing its over-activation and the proliferation of cancer cells. These drugs work by binding to the HER2 receptor, preventing the signal that triggers cell growth and division. The efficacy of these therapies varies depending on factors such as the stage of the cancer and the individual patient’s response.
Comparison of Treatment Approaches
The effectiveness of different treatment approaches varies significantly based on the HER2 status. Traditional chemotherapy regimens, while effective for some breast cancers, may not be as successful in HER2-positive cases. In contrast, targeted therapies specifically designed for HER2-positive tumors demonstrate a higher rate of success in controlling the disease and achieving remission. This highlights the importance of accurate HER2 testing for tailoring treatment strategies.
Treatment Options Summary
| Treatment Category | Targeted Therapies | Mechanism of Action |
|---|---|---|
| HER2-Targeted Therapy | Trastuzumab (Herceptin), Pertuzumab, Lapatinib, Ado-trastuzumab emtansine (T-DM1), Neratinib | These drugs directly target the HER2 protein, blocking its activity and preventing cancer cell growth. Some therapies, like T-DM1, combine targeted therapy with chemotherapy. |
| Chemotherapy | Various agents | Chemotherapy drugs work by killing rapidly dividing cells, which includes cancer cells. The use of chemotherapy is often considered alongside targeted therapies for optimal results. |
| Hormonal Therapy | Tamoxifen, Aromatase Inhibitors | Hormonal therapy is sometimes used in conjunction with other therapies, particularly in cases where the tumor is hormone receptor-positive. |
| Radiation Therapy | Radiation beams | Radiation therapy can be used to target and destroy cancer cells in specific areas, often following surgery or in combination with other treatments. |
Importance of Early Diagnosis
Early detection of HER2-positive breast cancer is crucial for improving treatment outcomes and significantly increasing the chances of survival. Understanding the importance of early diagnosis empowers individuals to take proactive steps towards their health and potentially save their lives. By recognizing the signs and symptoms, and participating in regular screenings, individuals can significantly improve their chances of successful treatment.
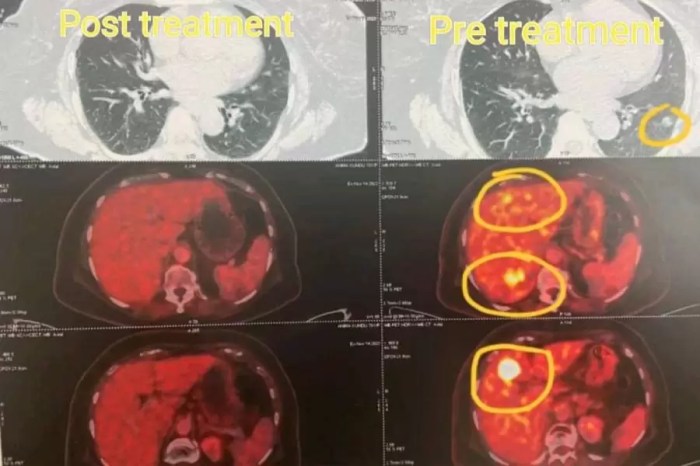
Impact on Treatment Outcomes
Early diagnosis allows for the implementation of targeted therapies, which are often more effective when the cancer is smaller and less aggressive. Treatment plans can be tailored to the specific characteristics of the tumor, leading to a higher likelihood of successful outcomes. For instance, if a patient is diagnosed with HER2-positive breast cancer at an early stage, they might benefit from less invasive treatment options compared to someone diagnosed at a later stage, potentially minimizing the physical and emotional impact of the disease.
Improved Survival Rates
Early diagnosis of HER2-positive breast cancer is directly correlated with higher survival rates. Studies consistently demonstrate that patients diagnosed with the disease at an early stage have a greater chance of long-term survival and a better quality of life. This is because the cancer has not had the opportunity to spread extensively throughout the body, making it more treatable.
For example, a patient diagnosed with early-stage HER2-positive breast cancer has a significantly higher chance of achieving long-term remission compared to someone diagnosed at a later stage.
Significance of Regular Screenings and Awareness
Regular breast cancer screenings, including mammograms, clinical breast exams, and self-exams, are vital for early detection. These screenings can help identify abnormalities that might indicate the presence of cancer, even before symptoms appear. Increased public awareness campaigns about the signs and symptoms of breast cancer and the importance of early detection play a crucial role in motivating individuals to seek prompt medical attention.
Furthermore, education about risk factors associated with HER2-positive breast cancer, such as family history, can empower individuals to take preventive measures and make informed decisions about their health.
Connection Between Early Diagnosis and Successful Treatment
The connection between early diagnosis and successful treatment in HER2-positive breast cancer is undeniable. Early detection often translates to less aggressive treatment approaches, minimizing the impact on the patient’s overall well-being. For example, a patient diagnosed with a small, localized tumor is more likely to respond positively to therapies such as surgery, radiation, or chemotherapy, potentially leading to a complete cure.
This is in contrast to a patient with advanced-stage cancer, where the spread of the disease may make complete eradication more challenging. In conclusion, early detection provides the best chance for successful treatment outcomes in HER2-positive breast cancer.
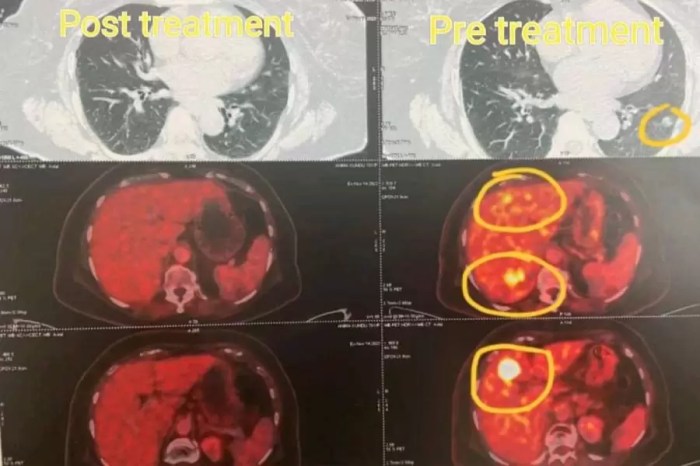
Visual Representation of HER2 Testing: Diagnosis And Testing For Her2 Positive Breast Cancer

Understanding HER2 testing is crucial for personalized breast cancer treatment. This process involves identifying whether a tumor has an amplified HER2 gene, a key factor in determining appropriate therapies. Different methods, like immunohistochemistry (IHC) and fluorescence in situ hybridization (FISH), provide valuable information about HER2 status. Visual representations of these tests can aid in understanding the results.
Immunohistochemistry (IHC) Testing
IHC is a common method for detecting HER2 overexpression. It involves staining the tumor tissue sample with an antibody that specifically binds to the HER2 protein. This staining allows pathologists to assess the level of HER2 expression in the tumor cells.
- Staining Patterns: The visual characteristics of HER2 staining under IHC are crucial for determining HER2 status. A strong, complete membrane staining of more than 30% of the tumor cells suggests HER2 positivity. Moderate membrane staining, which could range from 10-30%, or no membrane staining indicates a negative or ambiguous result. A weak membrane staining pattern is less likely to indicate HER2 positivity.
Fluorescence In Situ Hybridization (FISH) Testing
FISH is another method for assessing HER2 gene amplification. It involves using fluorescent probes that bind to the HER2 gene. This allows pathologists to visualize the number of HER2 gene copies in the tumor cells.
- Visualizing Gene Copies: Under a microscope, the fluorescent probes appear as signals around the HER2 gene. A ratio of HER2 to CEP17 centromere probes is calculated, providing insight into the HER2 gene copy number. A ratio greater than 2.0 is indicative of HER2 gene amplification and positivity. A ratio of 1.8 to 2.0 is considered an ambiguous result.
A ratio below 1.8 suggests HER2 negativity.
Visual Representation: A Hypothetical Example
Imagine a breast tissue sample stained with HER2-specific antibodies under IHC. The image would display tumor cells with varying levels of membrane staining. The intensity and distribution of the staining are crucial. Some cells may show intense staining throughout the membrane, while others might show faint or absent staining.In a FISH example, the microscopic image would show fluorescent signals (red and green) around the HER2 gene.
The intensity of these signals is critical in determining the HER2/CEP17 ratio. The image would demonstrate the relationship between the HER2 signals and the CEP17 signals. This comparison is key to determining if the HER2 gene is amplified. The ratio is calculated by counting the number of HER2 signals and the number of CEP17 signals, and the result determines the HER2 status.
Outcome Summary
In conclusion, accurate diagnosis and testing for HER2-positive breast cancer are vital for successful treatment. Early detection and understanding the role of HER2 status in treatment decisions are key to improving outcomes. This guide provides a comprehensive overview of the process, from initial diagnosis to personalized treatment options, highlighting the importance of early diagnosis and accurate testing in the fight against this aggressive form of breast cancer.