What is a medical spa? It’s more than just a fancy spa; it’s a blend of advanced medical procedures and luxurious relaxation. This unique space offers a wide range of services, from aesthetic enhancements to non-invasive treatments, all overseen by licensed medical professionals. Delving deeper, we’ll explore the specifics, comparing them to traditional spas, examining…
Author: Lonzo Howell
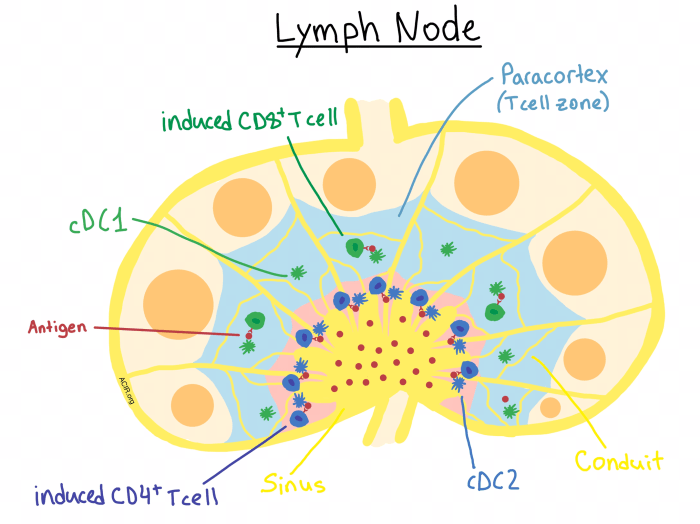
Understanding the Purpose of Lymph Nodes A Deep Dive
Understanding the purpose of lymph nodes sets the stage for this enthralling narrative, offering readers a glimpse into the intricate network of these vital structures within the human body. This exploration delves into the anatomical structure of lymph nodes, revealing their role in maintaining a healthy immune system. We’ll examine how these tiny filters work…
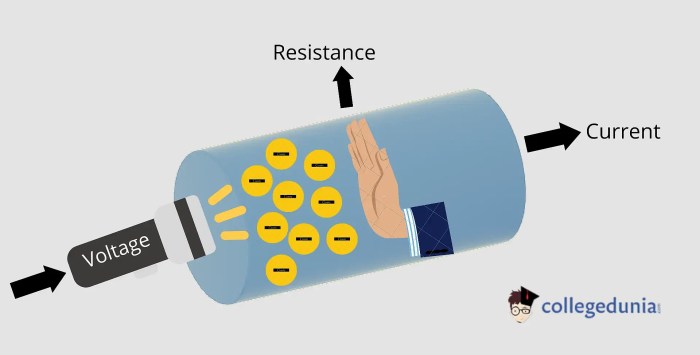
How to Use Resistance Bands Your Fitness Guide
How to use resistance bands? This guide dives deep into the world of resistance band workouts, revealing the secrets to unlocking your fitness potential. We’ll explore different band types, from color-coded to loop bands, and their varying strengths. You’ll discover a range of exercises, from beginner basics to advanced techniques, and learn how to tailor…
Saline Spray Snoring Allergies A Deep Dive
Saline spray snoring allergies: This comprehensive guide explores the connection between nasal saline sprays, snoring, and allergies. We’ll examine how these sprays can potentially alleviate both snoring and allergy symptoms, and discuss the various factors influencing their effectiveness, from lifestyle choices to underlying medical conditions. From understanding the different mechanisms to comparing various spray types,…
Facts about Corticosteroids Steroids A Deep Dive
Facts about corticosteroids steroids are essential for understanding these powerful medications. From their historical development to their diverse medical applications, potential side effects, and alternative treatments, this comprehensive guide delves into the intricacies of corticosteroids. We’ll explore their chemical structure, mechanism of action, and various administration methods, equipping you with crucial knowledge about these often-used…
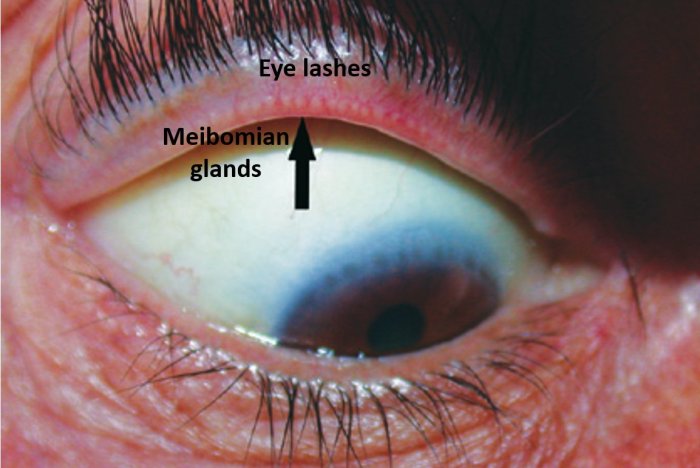
Bug Bite on Eyelid A Comprehensive Guide
Bug bite on eyelid: A frustrating and sometimes painful experience. This comprehensive guide delves into the intricacies of identifying, treating, and preventing these irritating bites around the delicate eye area. We’ll explore the various insects that might be the culprit, how to differentiate between a simple bite and more serious reactions, and what first-aid steps…
The Benefits of Saw Palmetto A Comprehensive Guide
The benefits of saw palmetto, a plant with a rich history of traditional use, are increasingly recognized in modern medicine. This comprehensive guide delves into the potential advantages of saw palmetto, exploring its effects on prostate health, hair growth, cardiovascular function, and even cognitive abilities. We’ll examine the science behind these claims, discuss potential side…
Ask an Expert HIV Support Groups
Ask an expert HIV support groups sets the stage for a deep dive into the crucial world of support for those living with HIV. We’ll explore the different types of groups, from online forums to in-person meetings, and examine the vital role of members and facilitators. This journey delves into finding the right support, addressing…
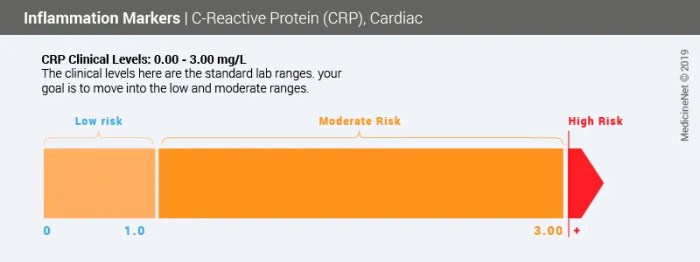
What is the CRP Test? Understanding C-Reactive Protein
What is the c reactive protein crp test – What is the C-reactive protein (CRP) test? This blood test measures inflammation levels in your body, offering valuable insights into your overall health. Understanding CRP levels is crucial for diagnosing various conditions and assessing your risk of future health problems. This comprehensive guide delves into the…
What to Know About Limonene A Deep Dive
What to know about limonene? This comprehensive guide delves into the fascinating world of this versatile compound, exploring its chemical makeup, natural sources, and diverse applications. From citrus fruits to cleaning products, limonene’s presence is surprisingly widespread. We’ll uncover its properties, uses, safety considerations, environmental impact, and more, providing a complete picture of this remarkable…