Tirzepatide Zepbound reduces blood pressure, a promising development in managing hypertension. This innovative medication, a dual GIP and GLP-1 receptor agonist, offers a novel approach to blood pressure regulation, potentially impacting not just blood pressure but also metabolic health and weight management. Early clinical trials are exploring its efficacy and safety profile, comparing it to…
Author: Lonzo Howell
Massage Therapy Helps Relieve Pain A Deep Dive
Massage therapy helps relieve pain, offering a holistic approach to managing discomfort. This exploration delves into various massage techniques, their physiological effects, and the types of pain they can address. We’ll examine specific muscle groups and areas often targeted for relief, along with a comparative analysis of different massage styles. Beyond the basics, we’ll investigate…
Types of Sleep Apnea A Deep Dive
Types of sleep apnea encompass a spectrum of breathing disorders that disrupt restful sleep. These conditions, ranging from the well-known obstructive sleep apnea to less common variations, can significantly impact overall health and well-being. Understanding the different types, their causes, symptoms, and treatment options is crucial for effective management and improved quality of life. This…
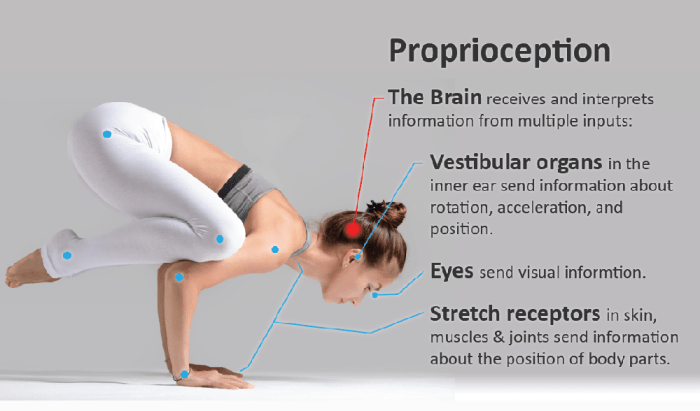
Proprioception in Multiple Sclerosis A Deep Dive
Proprioception in multiple sclerosis lays bare the intricate relationship between the nervous system and our sense of body awareness. This complex topic explores how multiple sclerosis impacts our ability to perceive our body’s position and movement, leading to a cascade of effects on daily activities. We’ll delve into the neurological underpinnings of proprioception, the specific…
How to Become a Pathologist A Comprehensive Guide
How to become a pathologist? This in-depth guide explores the path to this crucial medical career. From the necessary education and skills to training, certifications, and career opportunities, we’ll cover everything you need to know to embark on this rewarding journey. We’ll delve into the specifics of medical degrees, essential soft skills, and the technologies…
Treatment of Colon Cancer A Comprehensive Guide
Treatment of colon cancer is a multifaceted journey, demanding a deep understanding of the disease’s stages, diverse treatment approaches, and individualized care plans. This exploration delves into the various strategies, from surgical interventions to innovative therapies, providing a comprehensive overview of the complexities involved. We’ll examine the different types of colon cancer, the diverse range…
What are Food Deserts? A Deep Dive
What are food deserts? They’re areas where access to affordable, healthy food is limited, often due to a lack of grocery stores or supermarkets. This lack of access has profound effects on the health and well-being of communities, and understanding the complexities of food deserts is crucial to finding solutions. This exploration delves into the…
VLDL Understanding Very Low Density Lipoprotein
Very low density lipoprotein vldl – Very low density lipoprotein (VLDL) plays a crucial role in transporting lipids throughout the body. This essential component of lipid metabolism is synthesized in the liver and carries triglycerides to various tissues. Understanding its structure, metabolism, and potential implications for health is vital for anyone interested in maintaining a…
Robitussin vs Mucinex A Detailed Comparison
Robitussin vs mucinex how do they compare – Robitussin vs Mucinex: how do they compare? This in-depth look dives into the world of cough medicine, exploring the nuances of these popular over-the-counter options. We’ll examine their active ingredients, formulations, potential side effects, and ultimately, which might be the better choice for your specific needs. Get…
Why Do We Get Hiccups? Explained
Why do we get hiccups? This seemingly simple question delves into a fascinating interplay of nerves, muscles, and even historical beliefs. From the intricate pathways in our brainstem to the involuntary contractions of our diaphragm, understanding hiccups reveals a surprising complexity beneath this common, often annoying, experience. We’ll explore the neurological basis, the physiological mechanisms,…