Losing weight gluten free can be a rewarding journey, but it’s crucial to approach it with the right knowledge and strategies. This guide provides a comprehensive overview, exploring the potential benefits and common pitfalls of a gluten-free diet for weight management. We’ll delve into meal planning, practical strategies, and important considerations to ensure a sustainable…
Author: Jonatan Bergnaum
How to Stick to New Year Resolutions
How to stick to new year resolutions is a common struggle, but it doesn’t have to be a lost cause. This guide dives deep into the psychology behind resolutions, providing practical strategies to set realistic goals, build lasting habits, and overcome inevitable challenges. We’ll explore everything from understanding the common pitfalls to maintaining motivation throughout…
Can Ambien Affect Your Memory?
Can ambien affect your memory? This exploration delves into the potential impact of Ambien on various types of memory, from the fleeting moments of short-term recall to the lasting imprints of long-term memories. We’ll examine how this sleep aid might affect cognitive functions, the severity and duration of any memory impairment, and the underlying mechanisms…
The p53 Gene Its Crucial Role in Cancer
The p53 gene its role in cancer – The p53 gene, its role in cancer, is a pivotal area of research, exploring the gene’s intricate function in normal cellular processes and its dramatic impact on cancer development and progression. This gene acts as a crucial guardian, ensuring cellular health and preventing uncontrolled cell growth. Understanding…
Tour the Digestive System A Journey Inside
Tour the digestive system, a fascinating journey through the complex machinery of your body! This exploration dives into the intricate process of breaking down food, highlighting the vital roles of each organ from mouth to anus. We’ll uncover the amazing chemical and mechanical processes that transform a meal into usable energy, and explore the fascinating…
Fat vs Water-Soluble Vitamins A Deep Dive
Fat vs water soluble vitamins are crucial for our health, playing distinct roles in the body. Understanding their differences in absorption, storage, and function is key to maintaining optimal well-being. This exploration delves into the unique characteristics of each type, examining their absorption mechanisms, storage capacities, and dietary sources. We’ll also explore potential interactions and…
Am I Eligible for COBRA Health Insurance?
Am I eligible for COBRA health insurance? Navigating the complexities of COBRA can be daunting, especially after a job change or a reduction in work hours. This guide delves into the key factors that determine eligibility, exploring everything from the specific situations that trigger COBRA to the associated costs and the process of applying. We’ll…
Major Depressive Disorder Medications A Comprehensive Guide
Major depressive disorder medications are a crucial aspect of treatment for those struggling with this condition. This guide delves into the various types of medications used, exploring their mechanisms of action, effectiveness, and potential side effects. We’ll also examine factors influencing medication selection, patient adherence strategies, and emerging treatment directions. Get a deeper understanding of…
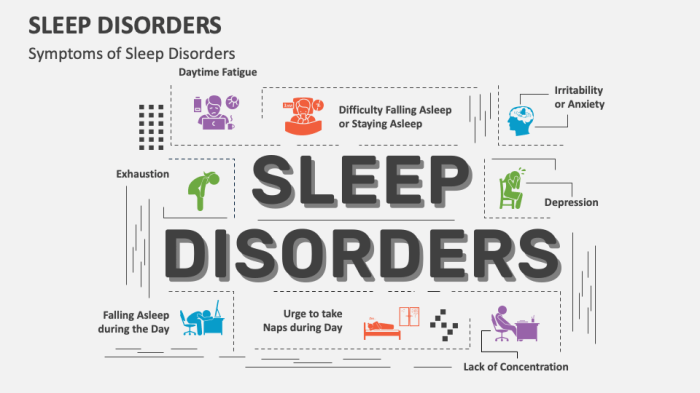
Types of Sleep Disorders A Deep Dive
Types of sleep disorders affect millions worldwide, disrupting not only individual well-being but also impacting society as a whole. From the common struggles of insomnia to the more complex conditions like sleep apnea, understanding the different types and their underlying causes is crucial for effective management and treatment. This exploration delves into the various sleep…
Steroid Injections Chronic Back Pain A Deep Dive
Steroid injections chronic back pain are a potential treatment option, but understanding the specifics is crucial. This in-depth look explores the mechanics, efficacy, procedures, patient considerations, and alternatives to help you make informed decisions. We’ll cover everything from the different injection types and their mechanisms of action to the potential risks and long-term management strategies….