What is a small stroke? This in-depth exploration delves into the intricacies of this often-overlooked medical condition, highlighting its defining characteristics, potential causes, diagnostic procedures, and treatment options. We’ll examine the subtle signs and symptoms, distinguish it from a TIA, and explore the long-term effects and recovery strategies. From the initial definition and medical terminology…
Author: Jonatan Bergnaum
How Does a Caffeine Nap Work?
How does a caffeine nap work? This intriguing question delves into the science behind the seemingly paradoxical practice of combining caffeine with a short sleep. We’ll explore the ideal timing, the physiological effects of caffeine, and the factors influencing nap quality. From understanding how caffeine interacts with your body to maximizing the benefits of this…
What Stage of Dementia is Sundowning?
What stage of dementia is sundowning? This perplexing phenomenon, characterized by a worsening of behavioral and cognitive issues during the late afternoon and evening hours, affects individuals with dementia in various ways. Understanding the link between sundowning and the progression of dementia is crucial for caregivers and medical professionals alike. This exploration delves into the…
Peppermint Uses Dosage & More
Peppermint uses dosage and more! From culinary delights to potential health benefits, this comprehensive guide explores the fascinating world of peppermint. We’ll delve into its botanical origins, historical uses, and a wide range of applications, from aromatherapy to skincare. Understanding the proper dosage and potential side effects is crucial for safe and effective use. This…
What are the Highest Paying Physician Careers?
What are the highest paying physician careers? This question sparks curiosity among aspiring doctors and seasoned medical professionals alike. Earning potential in medicine varies significantly, depending on a multitude of factors. Specialization, experience, and location all play crucial roles in shaping a physician’s income. This exploration delves into the factors that influence physician compensation, highlighting…
Four Skin Conditions That Make Your Feet Itch
Four skin conditions that make your feet itch can be incredibly frustrating. Understanding the underlying causes and symptoms is key to finding relief. This guide explores athlete’s foot, eczema, psoriasis, and other fungal infections, providing detailed information about each condition, including symptoms, causes, treatments, and preventative measures. We’ll also discuss home remedies and when to…
Can Coconut Oil Cause Yeast Infections?
Can coconut oil cause yeast infections? This question is frequently asked, and the answer isn’t as straightforward as some might claim. Coconut oil, with its purported health benefits, has sparked interest as a potential remedy for various ailments, including yeast infections. However, the scientific evidence surrounding its efficacy and potential side effects needs careful consideration….
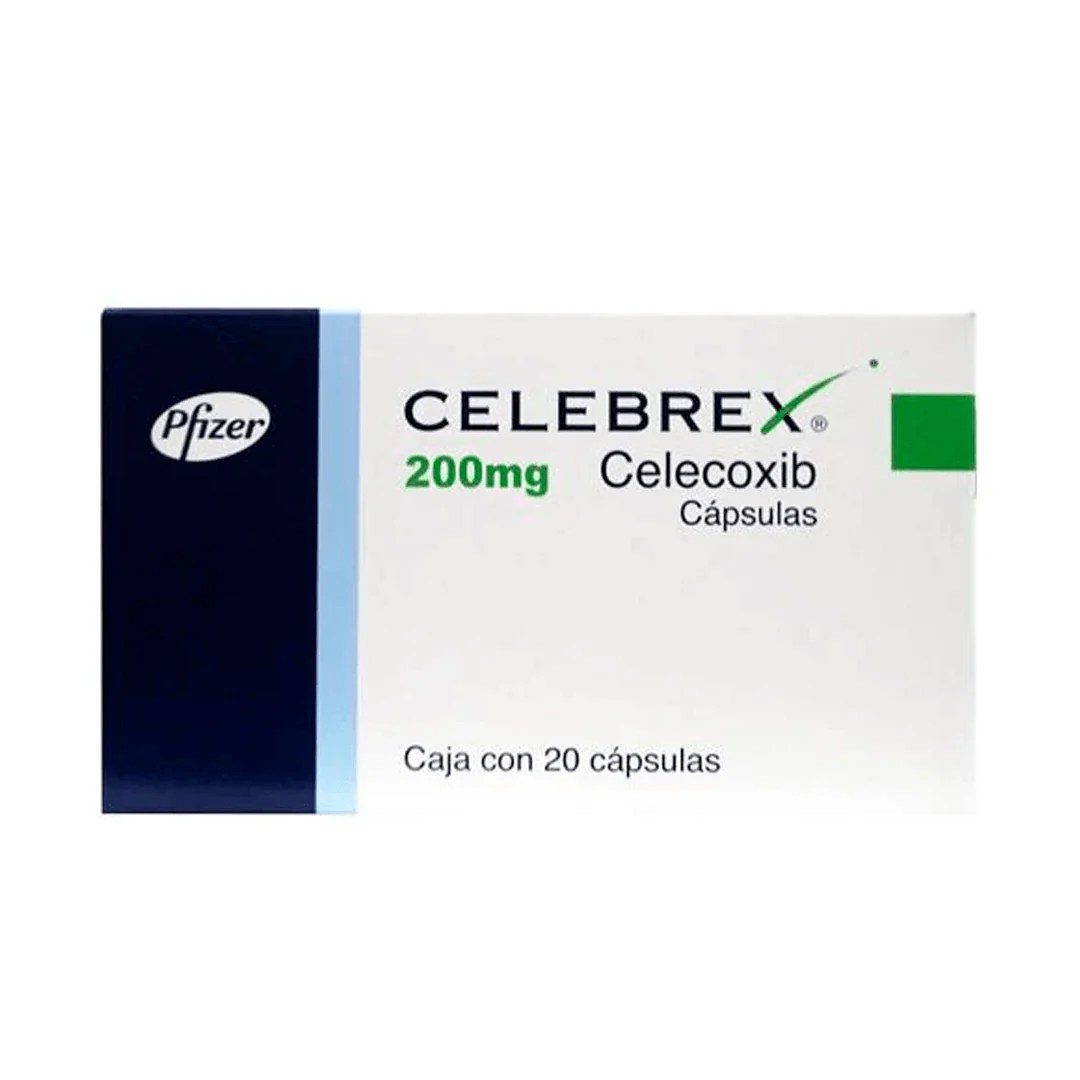
Celebrex vs Ibuprofen Which Pain Reliever?
Celebrex vs ibuprofen how to decide which you should use – Celebrex vs ibuprofen: how to decide which you should use. Choosing between these common pain relievers can be tricky. Both ibuprofen and celecoxib are effective, but they work differently in the body and have varying side effects. This guide will walk you through the…
Can You Get the Flu in the Summer?
Can you get the flu in the summer? While flu season is typically associated with winter, the possibility of contracting influenza during warmer months exists. Understanding the factors that influence flu transmission, and recognizing the potential symptoms, is crucial for staying healthy throughout the year. This article delves into the complexities of summer influenza, examining…
How to Cure Dry Eyes A Comprehensive Guide
How to cure dry eyes? This comprehensive guide dives deep into understanding, diagnosing, and treating dry eye syndrome. We’ll explore the various causes, symptoms, and stages of this common condition, and equip you with effective treatment options, from over-the-counter remedies to lifestyle changes. From understanding the intricate tear production process to exploring preventative measures and…