A new oral antibiotic for UTI promises a significant advancement in treating urinary tract infections. Current treatments often face limitations like antibiotic resistance and side effects. This new approach aims to address these challenges by offering a more effective, safer, and potentially more convenient solution. The global burden of UTIs is substantial, impacting healthcare systems…
Author: Jonatan Bergnaum
Understanding Your PSA Results A Comprehensive Guide
Understanding your PSA results is crucial for prostate health. This comprehensive guide delves into what a PSA test is, how results are interpreted, and the factors that can influence them. We’ll cover everything from normal ranges and potential causes of elevated PSA to the relationship between PSA levels and prostate cancer risk, as well as…
Short Arc Quad Exercise A Deep Dive
Short arc quad exercise is a targeted movement designed to strengthen and sculpt your quads. This exercise, often used in rehabilitation and strength training, focuses on controlled movements to maximize muscle activation. We’ll explore its variations, benefits, proper form, and safety considerations to ensure you get the most out of this powerful exercise. This comprehensive…
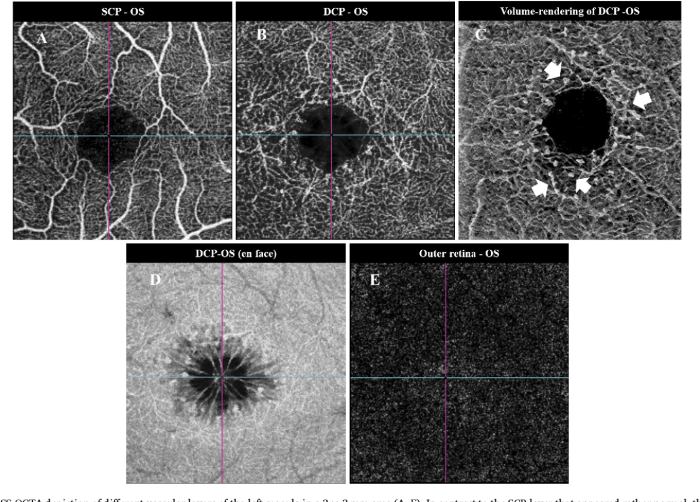
Macular Telangiectasia Type Two A Comprehensive Guide
Macular telangiectasia type two (MT2) is a chronic eye condition that affects the macula, the central part of the retina responsible for sharp, central vision. This guide delves into the intricacies of MT2, exploring its characteristics, causes, diagnosis, management strategies, and the impact it has on patients’ lives. We’ll cover everything from the early stages…
High Blood Pressure and PCOS A Deep Dive
High blood pressure and PCOS: understanding the connection is crucial for women’s health. High blood pressure, or hypertension, is a condition where the force of blood against your artery walls is consistently too high. Polycystic ovary syndrome (PCOS) is a hormonal disorder that affects women of reproductive age, often leading to irregular periods, excess hair…
Paxlovid Mouth What to Do
Paxlovid mouth what to do? This guide explores the potential oral side effects of Paxlovid, offering practical strategies for managing discomfort, and highlighting the crucial role of professional interventions and patient self-care. Many users experience oral issues while taking Paxlovid, ranging from dry mouth and sores to more severe complications. Understanding the potential problems, along…
Charmayne Andersons Asthma Journey A Personal Account
Charmayne anderson my personal journey with asthma – Charmayne Anderson’s My Personal Journey with Asthma takes readers on a deeply personal exploration of living with this chronic condition. From the initial diagnosis to the daily challenges and triumphs, Charmayne shares her experiences with honesty and vulnerability. This journey is not just about managing symptoms; it’s…
Does Drinking Water Help You Lose Weight?
Does drinking water help you lose weight? This intriguing question delves into the surprising ways hydration can influence your body’s metabolism, appetite, and overall calorie intake. We’ll explore the science behind how water impacts your body’s functions and whether it can truly be a key player in your weight loss journey. From boosting metabolism to…
Physical Therapy for Pectus Excavatum A Deep Dive
Physical therapy for pectus excavatum provides a vital pathway to managing this condition, offering a blend of exercises and techniques to address both the physical and emotional aspects of the condition. It’s a crucial component in the overall treatment plan, helping individuals regain strength, improve posture, and enhance breathing capacity. This comprehensive guide delves into…
The Benefits of Red Clover A Comprehensive Guide
The benefits of red clover extend far beyond its charming name. This comprehensive guide delves into the fascinating world of red clover, exploring its historical uses, nutritional profile, potential health benefits, and even its culinary applications. We’ll uncover the secrets of this versatile plant, from its botanical classification to its role in various industries. From…