Nausea medicine for pregnancy is a crucial aspect of prenatal care, offering pregnant women essential support during a challenging time. This comprehensive guide explores the physiological causes of morning sickness, comparing them to other potential causes of nausea. We’ll delve into various over-the-counter and prescription medications, natural remedies, and lifestyle strategies for managing nausea. Dietary…
Author: Jett Raynor
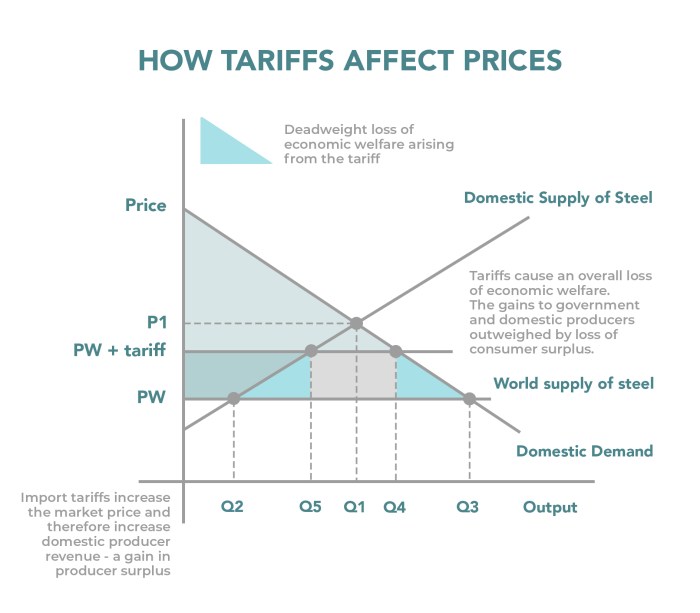
Tariffs and OTC Drugs A Global Overview
Tariffs and OTC drugs are intertwined in a complex global landscape. Understanding how tariffs impact the availability and cost of over-the-counter medications is crucial for consumers, manufacturers, and policymakers alike. This exploration delves into the historical trends, regional variations, and potential effects of tariffs on OTC drug markets worldwide. The impact on supply chains, manufacturing,…
Atopic Dermatitis vs Eczema A Deep Dive
Atopic dermatitis vs eczema – are they the same thing? This exploration delves into the similarities and differences between these skin conditions, highlighting their often-overlapping nature. We’ll uncover the historical understanding, examine the underlying causes, and explore the nuances of diagnosis and management. Understanding these distinctions is key to providing the best possible care for…
Does Birth Control Stop Your Period?
Does birth control stop your period? This is a common question for those considering or currently using birth control methods. Understanding how different types of birth control affect menstruation is key to making informed decisions. We’ll explore various methods, their impact on your cycle, and when periods might cease altogether. This detailed guide will walk…
Benefits of Drinking Hot Water A Deep Dive
Benefits of drinking hot water is a topic that has captivated cultures for centuries. From ancient traditions to modern wellness routines, the practice of consuming warm beverages holds a special place. This exploration delves into the history, health advantages, preparation methods, potential risks, cultural significance, scientific backing, and practical applications of drinking hot water. This…
Can You Overdose on Vitamins? A Deep Dive
Can you overdose on vitamins? This crucial question delves into the potential dangers of excessive vitamin intake. Vitamins are essential for bodily functions, but like any substance, too much can be detrimental. Understanding the potential for overdose, the mechanisms behind toxicity, and the symptoms involved is key to making informed choices about your health and…
Simple Steps to Increase Your Life Expectancy
Simple steps to increase your life expectancy are within reach. This guide unveils practical strategies to enhance your well-being and potentially extend your lifespan. We’ll explore dietary choices, physical activity, stress management, sleep hygiene, social connections, mindfulness, and preventative healthcare. Each section offers actionable steps you can incorporate into your daily routine. Discover the surprising…
Ask an Expert Creative Psoriasis Management
Ask an expert creative ways to manage psoriasis: This comprehensive guide delves into a wide range of strategies, from understanding the nuances of psoriasis to exploring innovative lifestyle modifications and cutting-edge treatments. We’ll explore everything from the basics of psoriasis, its diverse types, and contributing factors, to the latest in topical therapies, phototherapy, and systemic…
Foods to Ease Constipation A Guide
Foods to ease constipation are key to a healthy digestive system. Constipation, a common ailment, can be frustrating and uncomfortable. Fortunately, dietary changes can make a world of difference. This guide explores various fiber-rich foods, fruits, and vegetables that promote regularity, and even delves into other important dietary considerations for optimal bowel health. Understanding the…
How to Induce Labor A Comprehensive Guide
How to induce labor is a critical question for expectant parents facing potential delays in natural childbirth. This guide delves into the complexities of labor induction, exploring various methods, potential risks, and patient preparation. We’ll cover medical procedures, non-invasive techniques, and the factors that influence success rates. Understanding these aspects can empower parents to make…