Exercises for ankylosing spondylitis are crucial for managing this chronic inflammatory condition. This guide delves into the types of exercises, routines, and considerations needed to effectively incorporate movement into your life with AS. We’ll explore everything from personalized programs to lifestyle integration and how exercise impacts your overall well-being. Understanding the specific needs of those…
Author: Jett Raynor
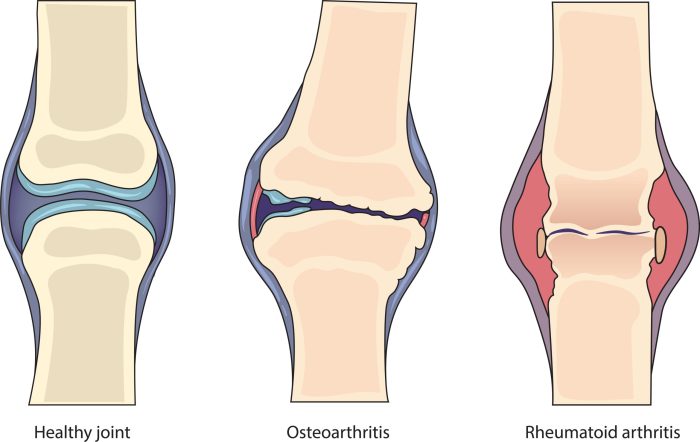
Rheumatoid Arthritis vs Arthritis A Deep Dive
Rheumatoid arthritis vs arthritis: Understanding the differences between these conditions is crucial for effective management and treatment. This comprehensive overview explores the nuances of rheumatoid arthritis (RA), contrasting it with general arthritis, to provide a clearer picture of these often-confused ailments. We’ll delve into their causes, symptoms, diagnostic processes, and treatment options, offering a practical…
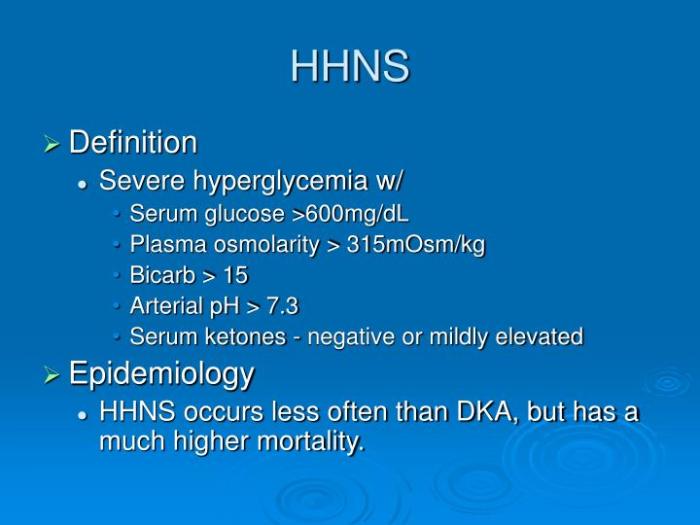
Hyperglycemic Hyperosmolar Nonketotic Syndrome A Deep Dive
Hyperglycemic hyperosmolar nonketotic syndrome (HHNS) is a serious complication of diabetes, characterized by extremely high blood sugar levels without the presence of ketones. This often occurs in individuals with type 2 diabetes, particularly those who aren’t managing their blood sugar well. Understanding the underlying mechanisms, symptoms, and management strategies is crucial for anyone at risk….
Identifying Insect Bites and Stings A Comprehensive Guide
Identifying insect bites and stings is crucial for prompt and appropriate treatment. This guide delves into the differences between bites and stings, explores common symptoms, and details assessment procedures, first aid, prevention, and specific insect types. From recognizing the subtle variations in bite marks to understanding potential allergic reactions, this comprehensive resource will equip you…
Why Do I Keep Getting Sick? The Truth
Why do I keep getting sick? This persistent illness can be frustrating, and understanding the underlying causes is key to regaining your well-being. This post delves into potential reasons, from lifestyle choices to underlying health conditions, environmental factors, and nutritional deficiencies. We’ll explore how each element impacts your immune system, offering insights and solutions for…
Proton Pump Inhibitors What They Do & How They Work
Proton pump inhibitors what they do and how they work – Proton pump inhibitors (PPIs) what they do and how they work are crucial for understanding their impact on digestion and overall health. These medications, commonly prescribed for conditions like heartburn and ulcers, exert their effects by targeting the proton pumps in the stomach lining….
High Heeled Shoes Bad for the Body?
High heeled shoes bad for the body? This exploration delves into the often-overlooked impact of these fashionable footwear choices on our physical well-being. From altering foot structure to affecting knee alignment and potentially causing injuries, we’ll examine the science behind the style. Understanding the potential consequences can empower us to make informed decisions about our…
Stoma Problems Recognizing the Signs
Signs of a problem with your stoma can range from mild discomfort to serious complications. Understanding these signs is crucial for managing your stoma effectively and maintaining your well-being. This guide delves into potential issues, their severity, and the importance of seeking timely medical attention. Identifying the specific signs and symptoms associated with your type…
What are Squamous Cells A Comprehensive Guide
What are squamous cells? These flat, scale-like cells play crucial roles throughout the body, from lining our respiratory tracts to protecting our skin. Understanding their diverse functions, locations, and potential abnormalities is key to grasping their significance in health and disease. This in-depth look at squamous cells will cover their defining characteristics, highlighting their structural…
Magnesium L-Threonate vs Glycinate A Deep Dive
Magnesium l threonate vs magnesium glycinate – Magnesium L-Threonate vs Magnesium Glycinate: Unveiling the best magnesium supplement for your needs. Choosing the right magnesium form can significantly impact your health and well-being. This comprehensive guide explores the nuances of two popular magnesium supplements: Magnesium L-Threonate and Magnesium Glycinate. We’ll delve into their chemical structures, absorption…