What is the most common cancer in the US? This crucial question delves into the leading causes of cancer, highlighting the factors that influence its prevalence. We’ll explore the key statistics, examining incidence rates, mortality figures, and the role of demographics, lifestyle choices, and environmental factors in shaping these trends. Understanding the most common cancer…
Author: Jett Raynor
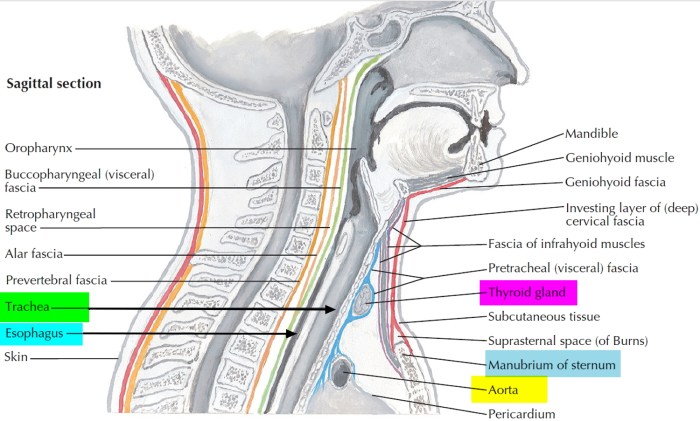
Trachea Function and Conditions and Diagram A Deep Dive
Trachea function and conditions and diagram provides a comprehensive overview of the windpipe, its crucial role in respiration, and the various conditions that can affect it. We’ll explore its intricate structure, examining how air travels through it, its impact on the overall respiratory system, and the diseases that can impact this vital part of our…
Should I Take Claritin, Zyrtec, or Allegra?
Should i take claritin zyrtec or allegra – Should I take Claritin, Zyrtec, or Allegra? This question plagues many allergy sufferers. Each of these popular antihistamines tackles allergy symptoms differently, and understanding their nuances is key to choosing the right one for you. This guide delves into the specifics of each medication, considering factors like…
Pasta Dishes for Low Cholesterol Diet
Pasta dishes for low cholesterol diet are a delicious way to enjoy pasta without compromising your health goals. This guide explores various pasta types, sauces, and ingredient combinations, ensuring your pasta meals are both satisfying and cholesterol-conscious. We’ll delve into portion control, recipe ideas, and visual examples to create a comprehensive approach to low-cholesterol pasta…
How to Keep Kidneys Healthy A Guide
How to keep kidneys healthy is a crucial aspect of overall well-being. Your kidneys are vital organs responsible for filtering waste and maintaining fluid balance in your body. This guide dives deep into the essential aspects of kidney health, offering practical advice and actionable steps you can take today. We’ll explore dietary recommendations, hydration strategies,…
Black Pepper Allergy Symptoms Diagnosis & Avoidance
Black pepper allergy symptoms diagnosis and what to avoid is a crucial topic for those susceptible to this often-overlooked food sensitivity. Understanding the range of symptoms, from mild discomfort to life-threatening reactions, is vital for early detection and effective management. This exploration delves into the complexities of identifying triggers, navigating the diagnostic process, and implementing…
Dysphoric Mood Warning Signs Coping Strategies
Dysphoric mood warning signs and how to cope is a crucial guide for understanding and managing emotional distress. This comprehensive resource delves into the nuances of dysphoric moods, from recognizing the initial signs to developing effective coping mechanisms and seeking professional help. We’ll explore various types of dysphoric moods, their triggers, and a range of…
Exercises for Ankylosing Spondylitis A Guide
Exercises for ankylosing spondylitis are crucial for managing this chronic inflammatory condition. This guide delves into the types of exercises, routines, and considerations needed to effectively incorporate movement into your life with AS. We’ll explore everything from personalized programs to lifestyle integration and how exercise impacts your overall well-being. Understanding the specific needs of those…
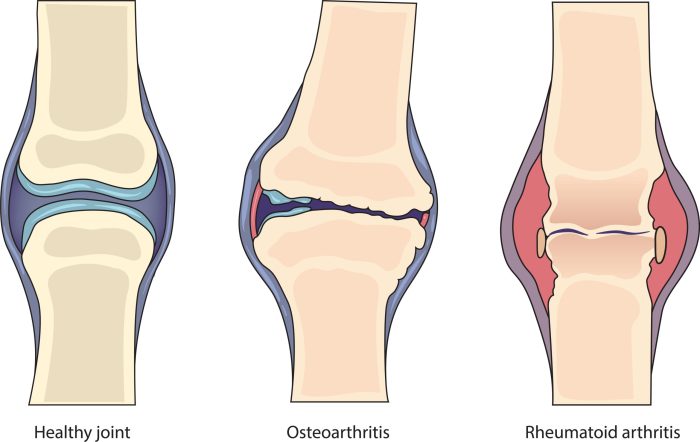
Rheumatoid Arthritis vs Arthritis A Deep Dive
Rheumatoid arthritis vs arthritis: Understanding the differences between these conditions is crucial for effective management and treatment. This comprehensive overview explores the nuances of rheumatoid arthritis (RA), contrasting it with general arthritis, to provide a clearer picture of these often-confused ailments. We’ll delve into their causes, symptoms, diagnostic processes, and treatment options, offering a practical…
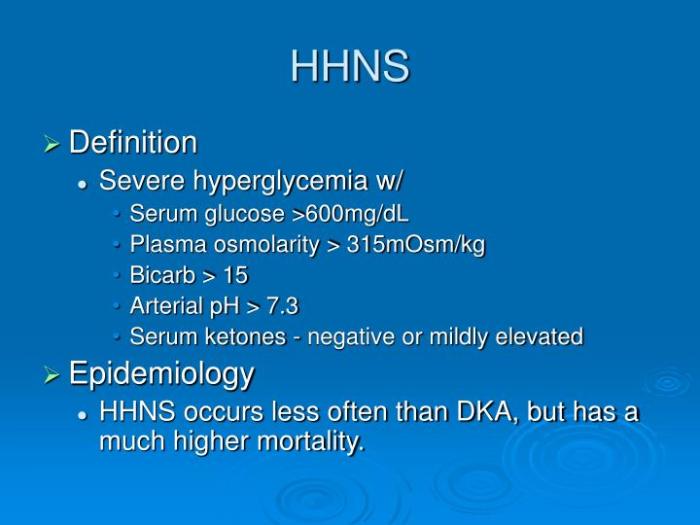
Hyperglycemic Hyperosmolar Nonketotic Syndrome A Deep Dive
Hyperglycemic hyperosmolar nonketotic syndrome (HHNS) is a serious complication of diabetes, characterized by extremely high blood sugar levels without the presence of ketones. This often occurs in individuals with type 2 diabetes, particularly those who aren’t managing their blood sugar well. Understanding the underlying mechanisms, symptoms, and management strategies is crucial for anyone at risk….