How hyperkalemia is diagnosed involves a multifaceted approach, starting with a thorough patient history and physical examination. This comprehensive guide details the key steps, from initial assessment to advanced laboratory testing and imaging techniques. Understanding the nuances of each stage is crucial for accurate diagnosis and effective treatment. The diagnostic process for hyperkalemia begins with…
Author: Jett Raynor
How Depression Is Diagnosed A Comprehensive Guide
How depression is diagnosed is a multifaceted process, requiring careful consideration of various factors. From understanding the core symptoms and diagnostic criteria to the crucial role of the clinician and cultural sensitivities, this exploration delves into the complexities of accurately identifying depression. We’ll examine the historical evolution of diagnostic methods, exploring the strengths and weaknesses…
Total Knee Replacement Rehab A Guide
Rehabilitation protocol after a total knee replacement is crucial for a successful recovery. This guide breaks down the process into distinct phases, from the initial weeks to long-term considerations. Understanding the exercises, activities, and important aspects of recovery can help you achieve optimal results and minimize potential complications. This protocol covers everything from the early…
Protein Weight Gain or Loss Your Ultimate Guide
Protein weight gain or loss is a complex topic, but understanding the role of protein in your body is key to achieving your fitness goals. This comprehensive guide delves into the science behind protein’s impact on weight management, from building muscle to shedding fat. We’ll explore different protein sources, optimal intake strategies, and potential health…
Tips for Coping with MS A Comprehensive Guide
Tips for coping with MS is a crucial resource for navigating the challenges of living with Multiple Sclerosis. This guide delves into practical strategies for managing symptoms, improving well-being, and fostering a positive outlook. We’ll explore lifestyle adjustments, emotional coping mechanisms, and essential communication techniques to empower individuals living with MS. From understanding the different…
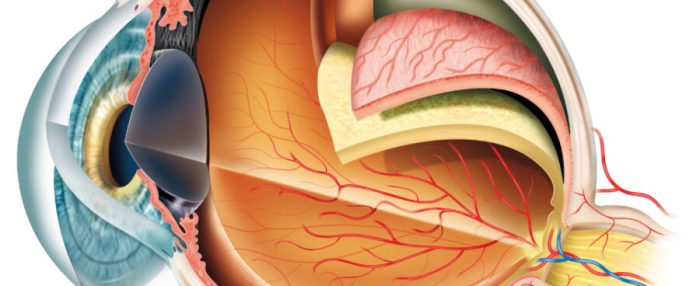
Eye Injections for AMD A Comprehensive Guide
Eye injections for AMD offer a potential lifeline for those struggling with age-related macular degeneration. This guide delves into the intricacies of these treatments, exploring the different types of AMD, the medications used in eye injections, and the procedures involved. We’ll also discuss the potential benefits, risks, and post-injection care. Understanding the specifics of eye…
What is Palliative Care A Comprehensive Guide
What is palliative care? It’s a specialized approach to care that focuses on improving the quality of life for people facing serious illnesses. Unlike curative care, which aims to cure disease, palliative care aims to provide comfort and support, both for the patient and their loved ones. This comprehensive guide explores the various aspects of…
How to Uncover a Doctors Medical Malpractice History
How to uncover a doctors medical malpractice history – How to uncover a doctor’s medical malpractice history is a complex process, demanding careful research and understanding of legal boundaries. This exploration delves into the intricate world of medical malpractice, examining the crucial steps needed to investigate a doctor’s past actions. It’s vital to approach this…
Are At-Home COVID Tests Accurate Enough?
Are at home covid tests accurate enough – Are at-home COVID tests accurate enough? This question has been a source of much debate and concern as at-home testing has become increasingly prevalent. Factors like test type, proper usage, and individual circumstances can significantly impact accuracy. This exploration dives deep into the accuracy of these convenient…
Can Allergies Cause Body Aches?
Can allergies cause body aches? This question delves into the fascinating connection between allergic reactions and the often-misunderstood discomfort of body aches. Understanding the intricate mechanisms behind this link is key to recognizing and managing these symptoms effectively. From the initial triggers to the physiological responses, this exploration unravels the mysteries surrounding allergic body aches,…