Treating ear infections in adults is a crucial aspect of healthcare. This guide delves into the various types, causes, and symptoms of ear infections in adults, offering a detailed overview of diagnosis, treatment options, and preventive measures. Understanding the unique needs of different adult populations, like pregnant women or the elderly, is also emphasized. From…
Author: Jaiden Mayer
Cervix in Early Pregnancy A Deep Dive
Cervix in early pregnancy plays a crucial role in the healthy development of a pregnancy. This deep dive explores the fascinating physiological changes the cervix undergoes during the first trimester, influenced by hormones, and how these changes can affect the entire pregnancy journey. We’ll examine cervical length monitoring, mucus characteristics, and potential risks, along with…
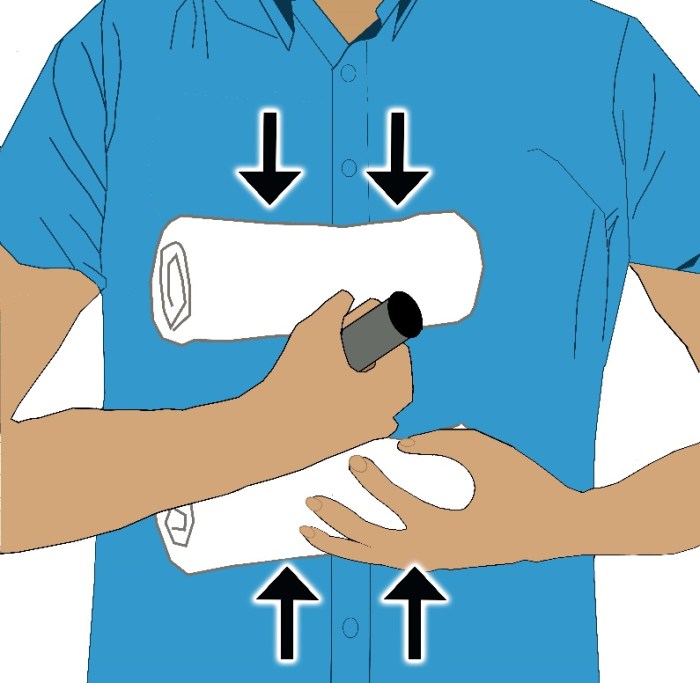
How to Treat an Impaled Object A Guide
How to treat an impaled object is a critical skill to possess. This guide will walk you through the essential steps for initial assessment, stabilization, first aid, and transport, ensuring the best possible outcome for the injured person. From recognizing potential dangers to understanding specific scenarios, this comprehensive approach will empower you to handle this…
De Novo Metastatic Breast Cancer A Deep Dive
De novo metastatic breast cancer presents a unique challenge, representing breast cancer that spreads to other parts of the body from the start, without any prior evidence of local or regional spread. This contrasts with other forms of metastatic breast cancer, and understanding its distinct characteristics, risk factors, diagnostic procedures, and treatment options is crucial…
Where to Find Free Condoms A Comprehensive Guide
Where to find free condoms? This guide dives deep into the resources available to ensure everyone has access to essential preventative measures. We’ll explore community centers, health clinics, universities, and government initiatives, alongside online resources and crucial safety considerations. This isn’t just about condoms; it’s about empowering individuals and communities with the knowledge and tools…
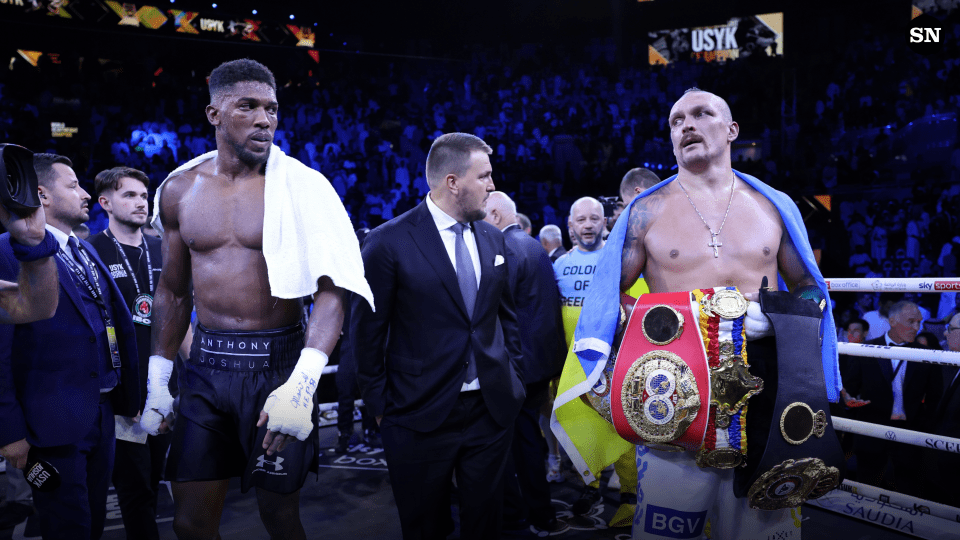
Anthony Wilsons Type 2 Diabetes Journey
Anthony wilson my journey with type 2 diabetes – Anthony Wilson’s journey with type 2 diabetes sets the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail and brimming with originality. He chronicles his experience from initial diagnosis to lifestyle adjustments, medical treatments, and the emotional and…
Start Exercising for Obesity Treatment A Guide
Start exercising for obesity treatment is crucial for a healthier lifestyle. This comprehensive guide dives deep into the physiological benefits of exercise for weight management, exploring various exercise types and personalized plans. We’ll uncover how exercise impacts metabolism and calorie expenditure, and how to seamlessly integrate it with a balanced diet. Beyond weight loss, we’ll…
Teflon Flu Understanding Polymer Fume Fever
Teflon flu polymer fume fever – Teflon flu, or polymer fume fever, is a respiratory illness often affecting workers handling Teflon. This potentially debilitating condition arises from inhaling fumes released during Teflon processing. Understanding its causes, symptoms, and preventative measures is crucial for occupational safety. This post delves into the intricacies of this often-overlooked health…
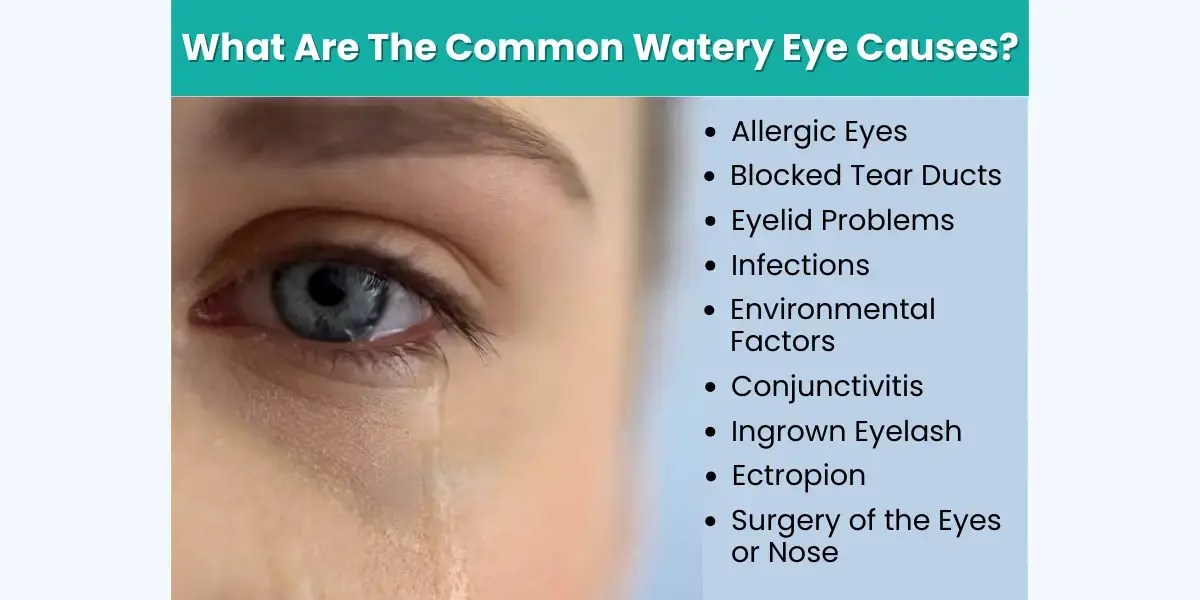
What Causes Watery Eyes? A Comprehensive Guide
What causes watery eyes? This insightful exploration delves into the myriad reasons behind those persistent, uncomfortable tears. From common allergies and infections to underlying medical conditions and environmental factors, we’ll uncover the root causes and provide a comprehensive understanding of this prevalent eye issue. This detailed guide will explore potential triggers, symptoms, diagnostic procedures, treatment…
Can Allergies Cause Loss of Taste and Smell?
Can allergies cause loss of taste and smell? This intriguing question delves into the complex interplay between our immune system and sensory perception. Allergies, triggered by our bodies’ overreaction to harmless substances, can manifest in a wide range of symptoms, from the familiar runny nose to more subtle effects like changes in taste and smell….