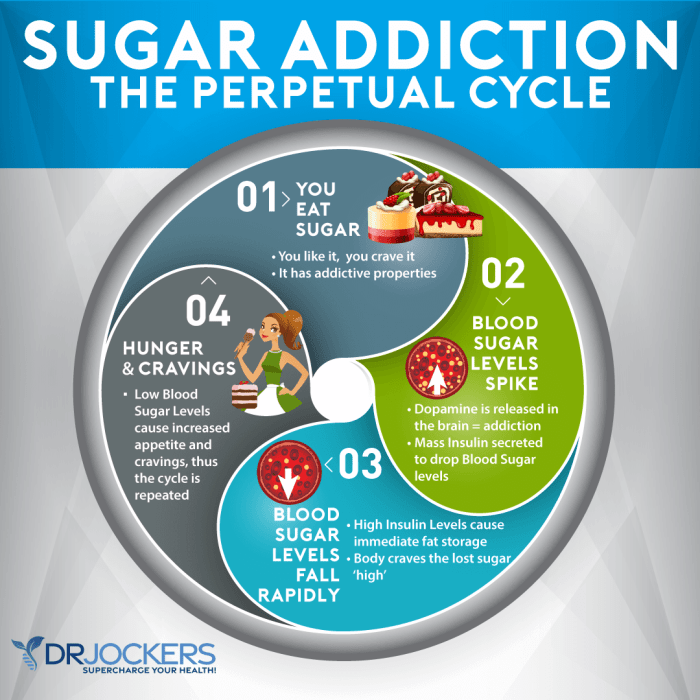
What happens if you eat too much sugar? This exploration delves into the immediate and long-term effects of excessive sugar consumption, from energy crashes to chronic health risks. We’ll uncover the science behind sugar’s impact on your body, providing actionable insights to make informed choices about your diet. From the initial spike in blood sugar…
Author: Herman Swift
Ways to Stop Sugar Cravings A Comprehensive Guide
Ways to stop sugar cravings – it’s a common struggle, but it doesn’t have to be a lifelong battle. This guide dives deep into understanding the root causes of these intense desires, from the science behind them to practical strategies for breaking free. We’ll explore everything from dietary adjustments and lifestyle changes to behavioral techniques…
Study Links Sleep Pattern to Successful Aging
Study links this sleep pattern to successful aging, revealing a fascinating connection between slumber and healthy aging. This research delves into a specific sleep pattern, exploring its characteristics, correlations with successful aging, and potential mechanisms. Understanding this sleep pattern could lead to valuable interventions for promoting healthy aging and well-being in older adults. The study…
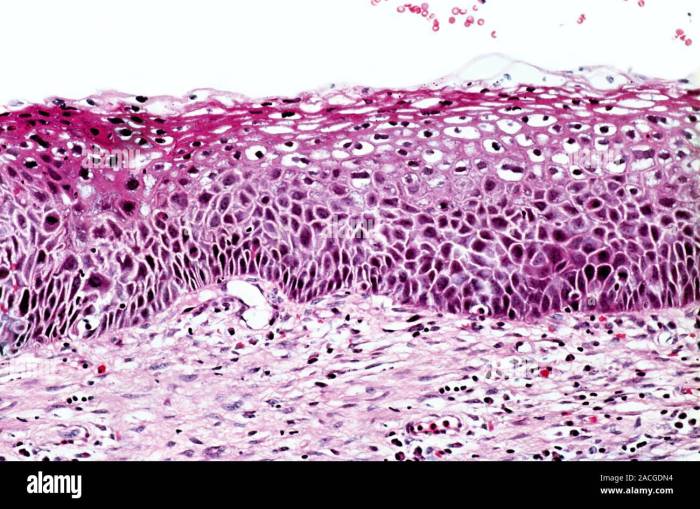
What is Cervical Intraepithelial Neoplasia? A Deep Dive
What is cervical intraepithelial neoplasia (CIN)? This condition, often linked to HPV, represents abnormal cell growth on the cervix. Understanding its various grades, from CIN 1 to CIN 3, is crucial for early detection and effective management. This blog post delves into the specifics of CIN, exploring its causes, diagnosis, treatment options, and preventative strategies….
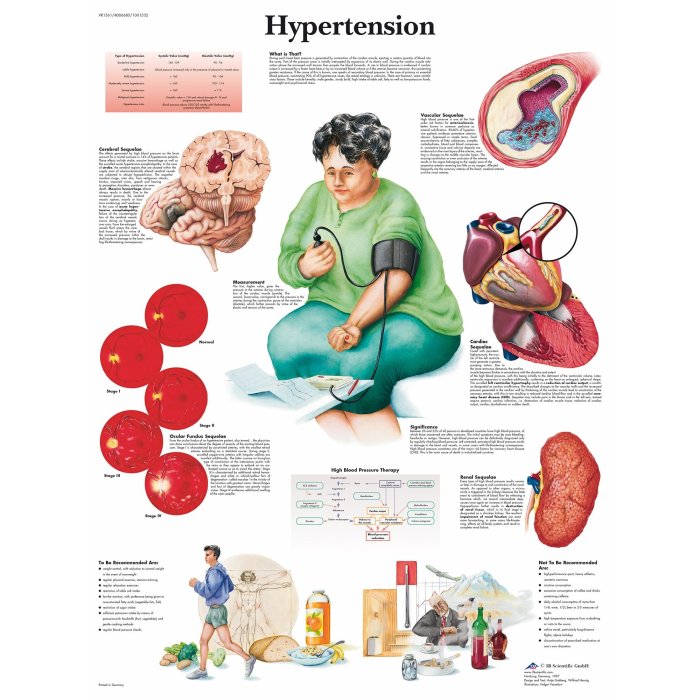
All About Hypertension Diagnosis A Comprehensive Guide
All about hypertension diagnosis: Understanding high blood pressure is crucial for maintaining good health. This in-depth guide explores the complexities of diagnosing hypertension, from initial evaluation to specialized testing and considerations for specific populations. We’ll delve into the different methods, from clinical assessments to lab tests, and provide a clear picture of the diagnostic process….
How to Use Mouthwash Your Oral Care Guide
How to use mouthwash effectively is crucial for optimal oral health. This guide delves into the world of mouthwash, exploring different types, proper technique, and the optimal frequency and duration for use. From understanding the various mouthwash formulations to incorporating them into your daily oral hygiene routine, we’ll cover everything you need to know. Mouthwash…
Does the Liver Regenerate? A Deep Dive
Does the liver regenerate? Absolutely! This fascinating organ possesses an incredible capacity for self-repair, a process crucial for its function and vital for human health. We’ll explore the intricate cellular mechanisms, the impact of various factors, and the clinical significance of this remarkable ability. From the molecular level to the broader implications for medicine, this…
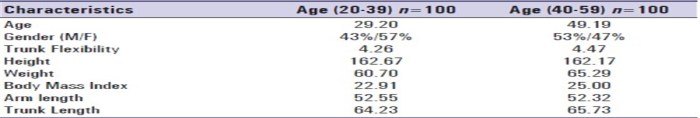
Functional Reach Test in Physical Therapy A Comprehensive Guide
The functional reach test in physical therapy sets the stage for understanding a crucial assessment tool for evaluating functional mobility. This test is used to measure the distance a person can reach forward from a standing position, providing valuable insights into balance and potential risks of falls. Understanding the test’s purpose, administration, interpretation, and limitations…
Best Time to Drink Coffee for Heart Health
Best time to drink coffee for heart health sets the stage for this exploration, delving into the fascinating interplay between our morning brew and cardiovascular well-being. We’ll uncover the potential impact of coffee consumption at different times of the day on your heart health, examining how factors like blood pressure, heart rate, and individual responses…
Metastatic Breast Cancer Resources A Guide
Metastatic breast cancer resources provides a comprehensive overview of this challenging disease, from understanding the stages and symptoms to navigating treatment options and accessing crucial support systems. This guide delves into the specifics of metastatic breast cancer, offering valuable insights for patients, healthcare professionals, and anyone seeking reliable information. It’s a journey through the complexities…