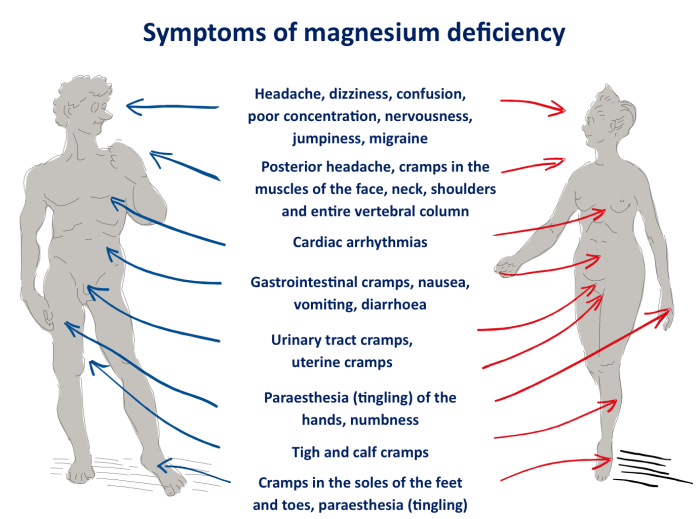
What vitamin deficiency causes muscle cramps? This comprehensive guide delves into the fascinating connection between essential vitamins and those painful muscle spasms. We’ll explore the various vitamins crucial for muscle function, and how their deficiency can trigger cramps. Understanding the specific roles of vitamins like calcium, magnesium, potassium, and vitamin D, along with their impact…
Author: Herman Swift
Green Grapes vs Red Grapes A Deep Dive
Green grapes vs red grapes – a seemingly simple comparison, but a world of flavor, nutrition, and cultural significance awaits exploration. From their vibrant colors to their distinct tastes, and even their surprising culinary uses, these two grape varieties offer a fascinating study in botanical diversity. This deep dive will uncover the differences in their…
Can Lysine Help Heal Cold Sores?
Can lysine help to heal cold sores? This question sparks intrigue, delving into the potential of this amino acid to combat the pesky herpes simplex virus. We’ll explore the science behind lysine’s role, compare it to other treatments, and weigh the potential benefits and risks of supplementation. Understanding the evidence is key to making informed…
Do Allergy Shots Really Work? A Comprehensive Guide
Do allergy shots really work? This in-depth exploration delves into the effectiveness, potential side effects, and alternatives to allergy shots. We’ll examine the science behind how these treatments work, discuss factors that influence success, and weigh them against other allergy management options. Understanding the mechanisms of allergy shots, the types available, and their typical timelines…
Lymphoscintigraphy Technique Sentinel Node Biopsy
Lymphoscintigraphy technique sentinel node biopsy provides a non-invasive way to identify the sentinel lymph nodes, crucial in cancer staging and treatment planning. This technique uses a radioactive tracer to map the lymphatic drainage pathway, highlighting the sentinel lymph nodes, which are the first lymph nodes to receive drainage from a tumor. Understanding the procedure, from…
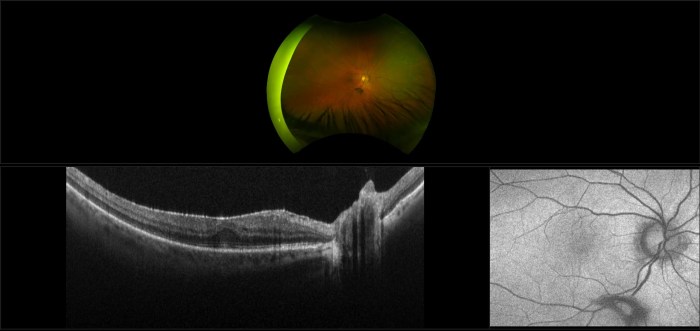
Epiretinal Membrane Retinal Scar Tissue A Deep Dive
Epiretinal membrane retinal scar tissue forms a delicate yet significant threat to vision. This intricate web of scar tissue, often developing on the retina, can lead to a range of visual disturbances. Understanding its formation, diagnosis, and treatment options is crucial for effective management and preserving sight. This post will explore the specifics of this…
Plant Polyphenols Slow Aging Study Unveiling Secrets
Plant polyphenols slow aging study investigates the potential of these compounds to combat the aging process. From flavonoids to phenolic acids, various types of plant polyphenols exhibit diverse biological roles within plants, hinting at their potential health benefits. This study delves into the mechanisms of aging, exploring how oxidative stress and cellular damage contribute to…
The Cortisol Weight Loss Controversy Debunked?
The cortisol weight loss controversy rages on. Is cortisol truly the villain in our weight struggles, or is there more to the story? This deep dive explores the complex relationship between cortisol, stress, and weight management, examining the science behind the claims and dissecting the differing perspectives on this often-misunderstood hormone. From the physiological mechanisms…
What to Do If You Are Sexually Assaulted A Guide
What to do if you are sexually assaulted? This guide provides crucial information on immediate steps, seeking support, navigating legal processes, and long-term healing. Understanding your rights and resources is essential in the aftermath of such a traumatic experience. The following sections detail how to respond to a sexual assault, from the initial reactions to…
Understanding Atonic Seizures What You Need to Know
What are atonic seizures? These are a type of seizure characterized by a sudden loss of muscle tone, leading to a brief period of falling or collapsing. Understanding their causes, symptoms, and treatment is crucial for those affected and their loved ones. This comprehensive guide delves into the intricacies of atonic seizures, providing valuable insights…