Lower back pain after sleeping is a common complaint, affecting countless individuals. This detailed exploration delves into the multifaceted causes, from poor sleep posture to underlying medical conditions. We’ll uncover the symptoms, diagnostic processes, and effective treatment options, providing you with actionable strategies for prevention and self-care. Understanding the nuances of this prevalent issue is…
Author: Herman Swift
Does Watermelon Trigger Migraines? A Deep Dive
Does watermelon trigger migraines? This intriguing question delves into the potential connection between this refreshing summer fruit and the debilitating headaches of migraines. We’ll explore the nutritional profile of watermelon, the characteristics of migraines, and the scientific understanding of food-related triggers, examining potential mechanisms and individual sensitivities. The discussion will also touch upon how watermelon…
Niacin Overdose Risks Explained
Risks of too much niacin can be serious, affecting your health in various ways. Understanding the potential dangers of excessive niacin intake is crucial for maintaining optimal well-being. This comprehensive guide delves into the various forms of niacin, its role in the body, and the risks associated with consuming too much. We’ll explore potential symptoms,…
How Long Does Valium Take to Work?
How long does it take Valium to work? This question is crucial for anyone considering or currently taking this medication. Valium, or diazepam, is a powerful benzodiazepine used to treat anxiety, muscle spasms, and seizures. Understanding the factors influencing its onset of action is key to managing expectations and ensuring optimal results. Different factors like…
Your Rights to Your Medical Records Under HIPAA
Your rights to your medical records under HIPAA are crucial for maintaining control over your health information. This guide delves into the specifics, exploring your ability to access, amend, and understand the disclosure of your medical records, along with your rights in the event of a security breach. Understanding these rights empowers you to navigate…
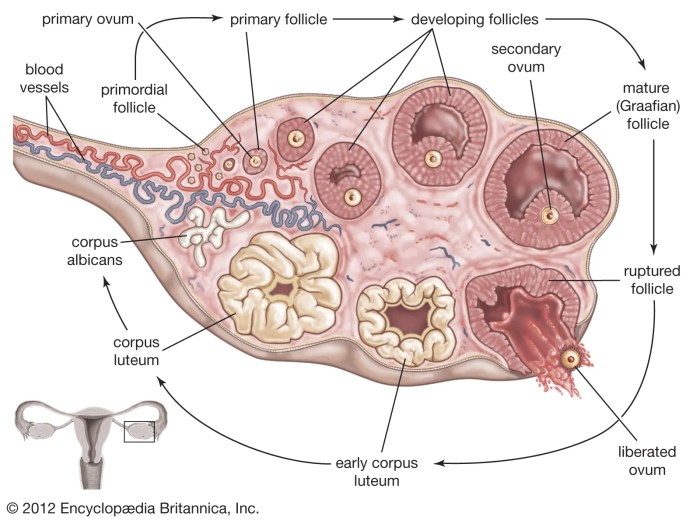
Things to Know About Your Ovaries and Ovulation
Things to know about your ovaries and ovulation: Dive deep into the fascinating world of female reproductive health. This comprehensive guide explores the intricate workings of your ovaries, the crucial ovulation process, and the overall menstrual cycle. From understanding ovarian anatomy to recognizing potential health concerns and fertility, you’ll gain valuable insights into your body’s…
Fertility When Are Your Most Fertile Days?
Fertility when are your most fertile days – Fertility: When are your most fertile days? Understanding your menstrual cycle and fertile window is key to optimizing your chances of conception. This comprehensive guide explores everything from the intricacies of your monthly cycle to the various methods for pinpointing your fertile days, including the calendar method,…
Three Things to Do with Expired Condoms
Three things to do with expired condoms: Proper disposal, understanding the risks of use, and exploring safe alternatives. This post dives into the crucial aspects of handling expired condoms, from safe disposal methods to the potential risks and ethical considerations. We’ll also explore alternative contraceptive options and the environmental impact of improper disposal. Expired condoms,…
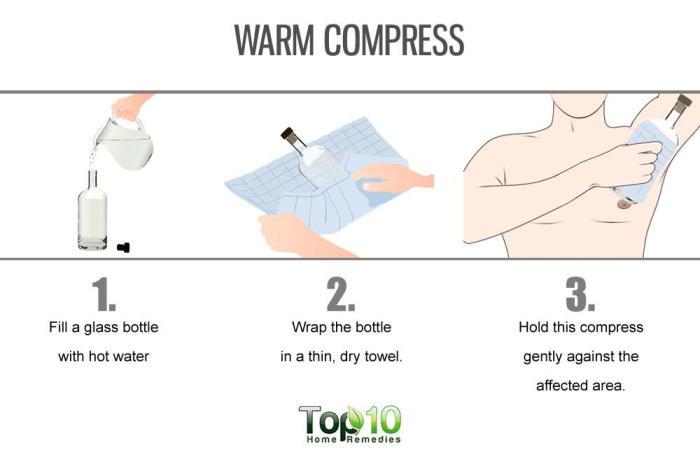
Hidradenitis Suppurativa Home Remedies A Guide
Hidradenitis suppurativa home remedies offer a potential path toward managing this chronic skin condition. This guide explores various approaches, from natural ingredients to lifestyle changes, to provide a comprehensive overview. We’ll delve into potential benefits and drawbacks, along with essential considerations before trying any home remedy. Understanding the nuances of Hidradenitis Suppurativa (HS) is crucial…
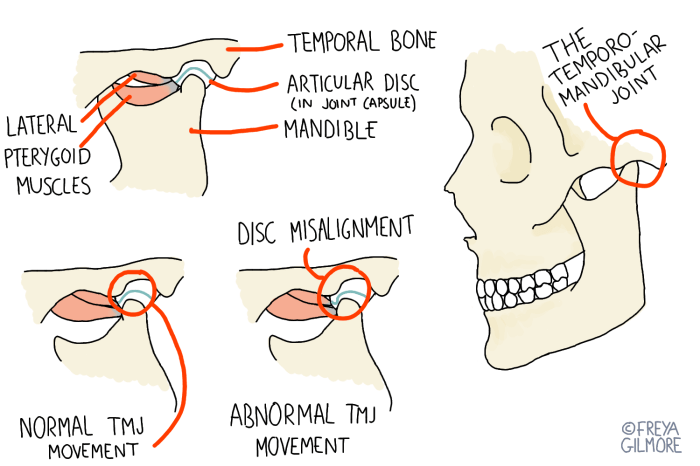
What is TMJ Disorder? A Deep Dive
What is TMJ disorder? This comprehensive guide delves into the complexities of temporomandibular joint (TMJ) disorders, exploring everything from their intricate anatomy to effective treatment options. Understanding the structure and function of the TMJ is crucial to grasping the various types of TMJ disorders and their associated symptoms. We’ll also explore the causes, diagnosis, and…