Metastatic breast cancer care team: navigating the complexities of treatment and support for those facing this challenging journey. This guide delves into the intricate roles, responsibilities, and collaborations within a comprehensive care team, highlighting the importance of effective communication and patient-centered approaches. From defining the various disciplines represented, such as oncologists, surgeons, and nurses, to…
Author: Deontae Botsford
Avocado Oil vs Olive Oil A Culinary Showdown
Avocado oil vs olive oil – a debate that’s been raging in kitchens worldwide! Both are incredibly versatile cooking oils, but which one reigns supreme? This deep dive explores their flavor profiles, nutritional value, culinary applications, sustainability, and cost, to help you decide which oil best fits your needs. From the smooth, buttery texture of…
CPAP Gas Causes, Treatment, and Safety
The causes and treatment of CPAP gas are crucial for optimal sleep apnea therapy. Understanding the different gases used, potential issues, and effective solutions is essential for patient comfort and well-being. This comprehensive guide explores the complexities of CPAP gas delivery, from defining the various gases to addressing common problems and safety considerations. This article…
Autism Test for Adults Your Guide
Autism test for adults is a crucial step for understanding and navigating the complexities of autism spectrum disorder (ASD) in adulthood. Accurate diagnosis empowers individuals to access appropriate support and resources, leading to improved well-being and quality of life. However, the process can be challenging, with various assessment methods, considerations for co-occurring conditions, and the…
Signs of Autism in Girls Understanding the Differences
Signs of autism in girls often go unnoticed, presenting in ways that differ from the typical picture portrayed in many sources. This insightful look delves into the unique characteristics of autism in girls, exploring the challenges in identification and the common misconceptions surrounding their experiences. We’ll examine how social cues, sensory processing, and emotional regulation…
Foods to Help Gain Weight A Comprehensive Guide
Foods to help gain weight are more than just calorie-dense options; they’re the building blocks for a healthy, positive transformation. This guide delves into the nutritional value of various foods, highlighting the importance of macronutrients like protein, carbohydrates, and healthy fats for muscle growth and overall well-being. We’ll explore calorie-dense foods, safe strategies for weight…
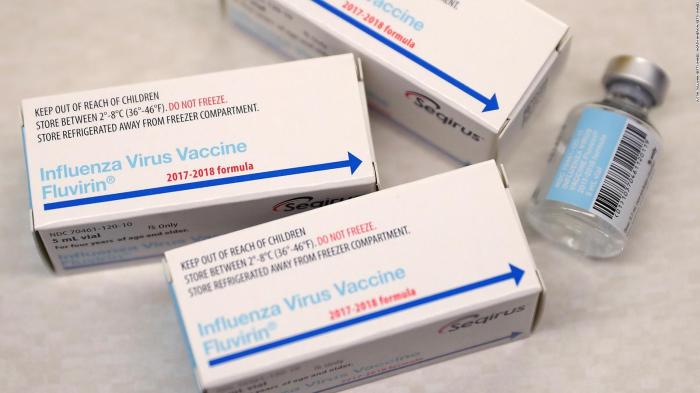
Preservative-Free Flu Vaccine A Deep Dive
Preservative free flu vaccine – Preservative-free flu vaccine is a significant advancement in immunization, offering a potentially safer alternative to traditional flu shots. This exploration delves into the history, safety, manufacturing, and public health implications of this evolving approach to influenza prevention. We’ll examine the reasons behind the shift towards preservative-free options and compare them…
Types of Asthma Doctors Finding the Best Fit
Types of asthma doctors and choosing the best one sets the stage for navigating the complexities of asthma care. Understanding the different types of asthma, from allergic to exercise-induced, is crucial. This exploration delves into the roles of pulmonologists, allergists, and general practitioners, providing insights into their expertise and how they collaborate to ensure optimal…
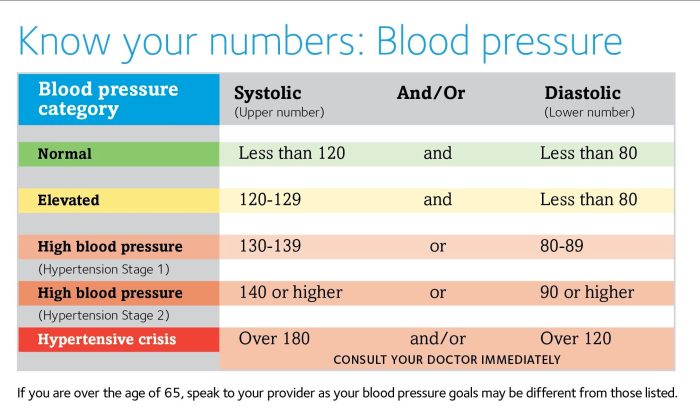
Normal Blood Pressure Fluctuations Throughout the Day
Normal blood pressure fluctuations throughout the day are a natural part of human physiology. These variations are driven by a complex interplay of internal and external factors, from the simple act of standing to the intricate dance of our autonomic nervous system. Understanding these fluctuations is key to recognizing healthy patterns and identifying potential issues….
Best Time of Day for Kefir & Gut Health
Best time of day drink kefir gut health is a crucial aspect for maximizing its potential benefits. Understanding the ideal time to consume kefir, alongside the impact of meal timing and individual factors, is key to optimizing its effects on gut health. From its probiotic-rich nature to its role in digestion, kefir offers a compelling…