Are smoothies good for you? This exploration delves into the nutritional value, health benefits, potential drawbacks, and more. We’ll examine the ingredients, preparation methods, and how smoothies fit into a balanced lifestyle. From the vitamins and minerals packed into various fruits and vegetables, to the potential pitfalls of excessive consumption, this guide will equip you…
Author: Deontae Botsford
What Exercise Burns the Most Calories? Unveiling the Truth
What exercise burns the most calories? This question fuels countless fitness journeys, and the answer isn’t as straightforward as you might think. Different activities tap into various energy systems, leading to varying calorie burn rates. This exploration delves into the science behind calorie expenditure, from the basics of various exercises to the impact of individual…
Is Beef Jerky Healthy? A Deep Dive
Is beef jerky healthy? This question sparks a fascinating exploration into the nutritional landscape of this popular snack. We’ll delve into the nutritional profile, scrutinize processing methods, and weigh the potential health benefits against the risks. From the protein content to the sodium load, we’ll cover everything you need to know to make an informed…
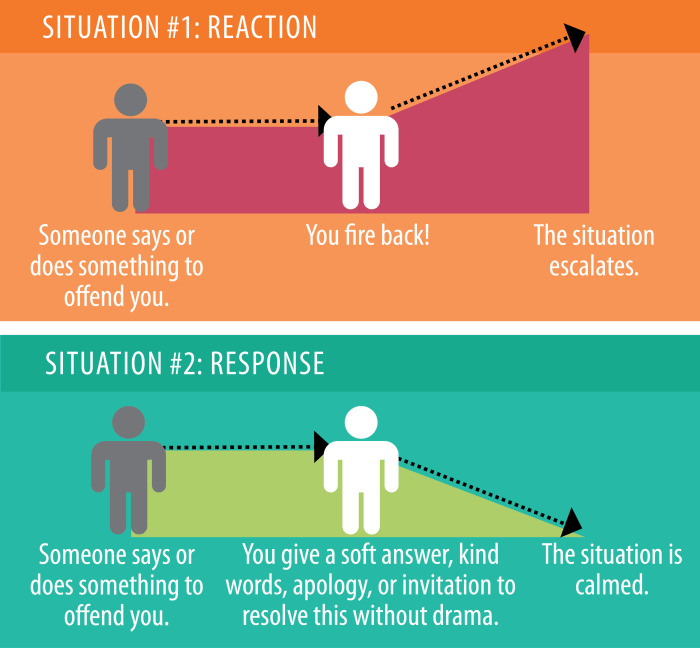
Responding to Confabulation in Dementia A Guide
Responding to confabulation in dementia is a crucial aspect of caregiving. This guide dives deep into understanding confabulation in dementia, from its definition and triggers to effective response strategies and communication techniques. We’ll explore how to identify confabulation, differentiate it from other cognitive impairments, and create supportive environments to help manage these episodes. This comprehensive…
ACL Surgery Making Your Decision
ACL surgery making a decision is a crucial juncture, often fraught with anxiety and uncertainty. This exploration delves into the multifaceted considerations surrounding this choice, from understanding the nuances of the injury itself to weighing surgical versus non-surgical options. We’ll navigate the decision-making process, examining the various factors that contribute to the best possible outcome…
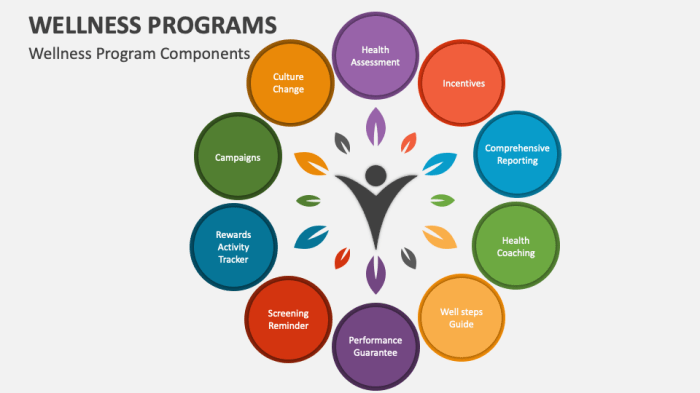
Health Benefits Jamu Drink A Deep Dive
Health benefits jamu drink, a traditional Indonesian herbal beverage, opens a fascinating window into the rich tapestry of natural remedies. From its historical roots in Southeast Asian cultures to its potential modern applications, jamu offers a unique perspective on holistic wellness. This exploration will delve into the diverse types of jamu drinks, their potent ingredients,…
What is CMV Cytomegalovirus? A Comprehensive Guide
What is CMV cytomegalovirus? This comprehensive guide delves into the world of cytomegalovirus (CMV), exploring its characteristics, transmission, diagnosis, treatment, prevention, complications, and impact on specific populations. We’ll uncover the intricacies of this common virus, providing a clear and accessible overview for anyone seeking information. From its basic structure and lifecycle to its effects on…
Side Effects of Diabetes A Comprehensive Guide
Side effects of diabetes can range from the immediate discomfort of high or low blood sugar to the long-term complications that affect various organs. This comprehensive guide delves into the complexities of these effects, exploring the differences between types of diabetes and the factors that influence their manifestation. Understanding these side effects is crucial for…
Are Cold Showers Good for You? A Deep Dive
Are cold showers good for you? This question sparks intense debate, as proponents tout numerous health benefits. From boosting cardiovascular health to potentially aiding muscle recovery, the allure of cold water therapy is undeniable. However, are there potential risks and side effects to consider? Let’s explore the science and the experiences behind this invigorating practice….
Can Allergy Medicines Really Stop Working?
Can allergy medicines really stop working? This intriguing question delves into the fascinating world of how our bodies react to these crucial medications. We’ll explore the mechanisms behind how allergy medications work, the factors that can impact their effectiveness, and even the potential for developing resistance over time. From understanding different types of allergy medications…