The benefits of sea buckthorn are truly remarkable. This versatile fruit, known for its rich nutritional profile and diverse applications, has been used for centuries in various cultures. From boosting your immune system to promoting radiant skin, sea buckthorn offers a multitude of potential health advantages. This comprehensive guide delves into the fascinating world of…
Author: Deontae Botsford
Conjugated Linoleic Acid Weight Loss A Deep Dive
Conjugated linoleic acid weight loss is a popular topic, but understanding the science behind it is key. This post explores the potential benefits, drawbacks, and considerations surrounding CLA supplementation for weight management. We’ll delve into the science, examine different types of CLA, and look at how diet and exercise play a crucial role in achieving…
Ozempic Novo Nordisk High Prices A Deep Dive
Ozempic Novo Nordisk high prices are a significant concern, prompting questions about affordability and accessibility. This blog post delves into the complexities surrounding this issue, examining the medication’s purpose, production costs, public perception, and potential solutions. From Novo Nordisk’s role in production to the impact on healthcare systems, we’ll explore the multifaceted factors driving these…
How to Reset Circadian Rhythm Your Guide to Better Sleep
How to reset circadian rhythm? This guide delves into the fascinating world of your internal clock, exploring the science behind sleep and the practical steps you can take to regulate your body’s natural sleep-wake cycle. From understanding the fundamental biological process to practical lifestyle changes, we’ll equip you with the knowledge and strategies to reclaim…
Flu Shot While Sick What to Expect
What will happen if i get a flu shot while im sick – What will happen if I get a flu shot while I’m sick? This post dives into the potential effects of receiving a flu shot when you’re already experiencing flu-like symptoms. We’ll explore how your body’s immune response might be impacted, examine the…
Nasal Congestion Symptoms, Causes, and Treatment
Nasal congestion symptoms causes and treatment – Nasal congestion symptoms, causes, and treatment: Understanding this common ailment is crucial for effective management. From the intricate workings of your nasal passages to the various triggers and remedies, this comprehensive guide delves into the world of stuffy noses. We’ll explore the anatomy, common symptoms, potential causes, and…
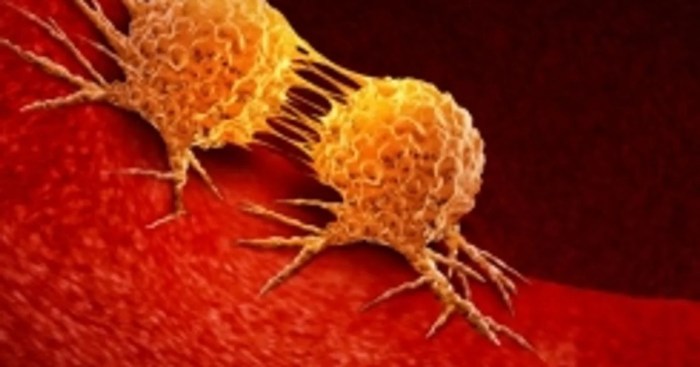
What is a Carcinogen Understanding the Dangers
What is a carcinogen? It’s a substance that can cause cancer. This exploration delves into the science behind these harmful compounds, from their various classifications to the long-term health effects they can trigger. We’ll uncover the mechanisms by which carcinogens damage DNA, examine the sources of exposure, and discuss strategies for prevention and mitigation. Understanding…
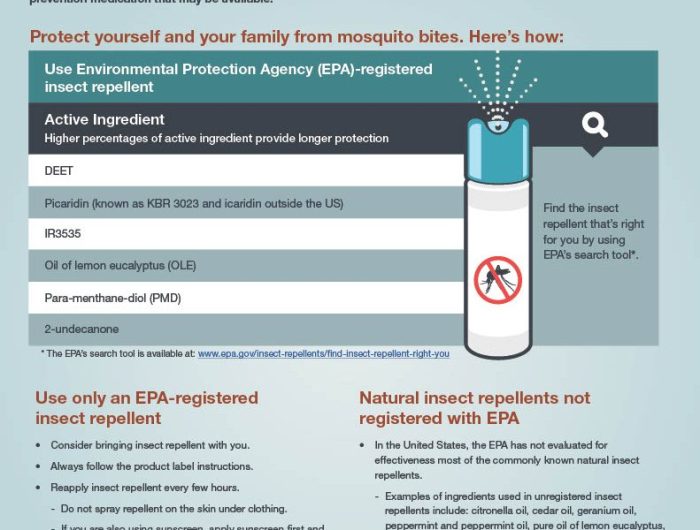
How to Prevent Mosquito Bites A Comprehensive Guide
How to prevent mosquito bites is a crucial topic for anyone spending time outdoors. Mosquitoes are more than just a nuisance; they can transmit serious diseases. This guide delves into the science behind mosquito behavior, their breeding habits, and effective prevention strategies. We’ll cover everything from identifying mosquito habitats to personal protection and community-wide control…
After Injury Inflammation A Deep Dive
After an injury inflammation – After injury inflammation is a crucial part of the healing process. This insightful exploration delves into the complexities of inflammation following an injury, from its fundamental role in tissue repair to the potential complications of prolonged or excessive inflammation. We’ll uncover the cellular mechanisms driving this response, discuss various types…
Skin Pain in Psoriasis A Deep Dive
Skin pain in psoriasis is a significant concern for many sufferers, impacting their daily lives and overall well-being. This detailed exploration delves into the various types of pain, their mechanisms, and the factors that exacerbate them. We’ll also examine the profound impact on daily routines, mental health, and social interactions. Further, we’ll discuss diagnosis, management…