What medications cause sundowning symptoms? This exploration delves into the often-overlooked connection between prescription drugs and the distressing phenomenon of sundowning. Sundowning, characterized by a decline in cognitive function and behavioral changes, typically occurring in the late afternoon or evening, can significantly impact individuals and their caregivers. While various factors contribute to sundowning, understanding the…
Author: Deontae Botsford
EPA PFAS Limits Drinking Water Safety
EPA PFAS limits drinking water, setting standards for a crucial aspect of public health. PFAS, or per- and polyfluoroalkyl substances, are a group of man-made chemicals found in various products and potentially in our water sources. These chemicals can persist in the environment and potentially pose health risks if present in drinking water above certain…
When to Take a Pregnancy Test with PCOS
When to take a pregnancy test if you have PCOS sets the stage for understanding the unique challenges and opportunities in trying to conceive. Navigating irregular cycles and symptoms can make timing a pregnancy test crucial. This guide dives deep into understanding PCOS, its impact on ovulation, and how to effectively predict and interpret those…
Safe OTC Pain Relievers During Pregnancy
Safe OTC pain relievers to take while pregnant are crucial for managing discomfort during pregnancy. Each trimester brings unique aches and pains, from morning sickness to backaches and headaches. Choosing the right, safe over-the-counter medication is vital for both your well-being and the health of your developing baby. This guide will explore the different types…
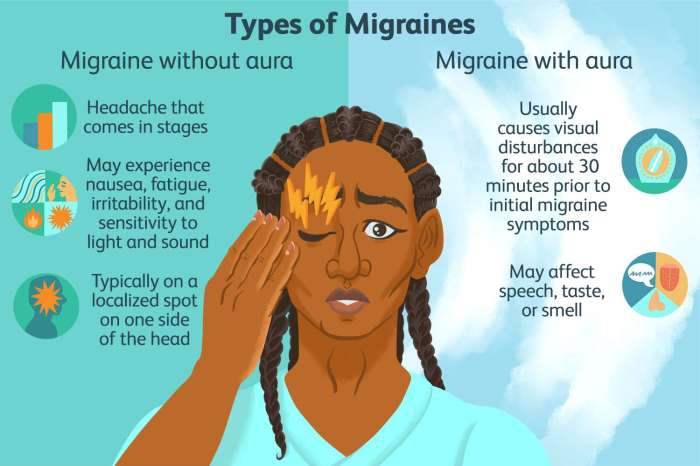
Episodic Migraine Prevention Medications A Guide
Episodic migraine prevention medications are a crucial aspect of managing these debilitating headaches. This guide delves into the various types of preventative treatments, their mechanisms of action, effectiveness, potential side effects, and important considerations for patient selection. We’ll explore everything from CGRP inhibitors to beta-blockers, providing a comprehensive overview to help you understand the best…
How Much Water is Too Much? A Deep Dive
How much water is too much? This seemingly simple question delves into a complex interplay of physiology, individual needs, and potential risks. Understanding the optimal hydration levels for different people is crucial for maintaining good health, but exceeding those levels can lead to a condition known as water intoxication. This exploration examines the nuances of…
What Does Anger Do to Your Body? Impacts & Management
What does anger do to your body? This sets the stage for a fascinating exploration of the immediate and long-term effects of anger on our physical well-being. From the initial physiological responses like a racing heart to the potential for long-term health consequences, we’ll delve into the intricate relationship between anger and the human body….
Side Effects of Statins A Comprehensive Guide
Side effects of statins can range from mild discomfort to serious health concerns. This comprehensive guide delves into the potential side effects of statins, exploring everything from common issues like muscle pain to less frequent but potentially severe complications. We’ll cover the science behind these effects, discuss factors that influence their occurrence, and provide practical…
What is a Wet Dream and What Does it Mean?
What is a wet dream and what does it mean? This exploration delves into the fascinating world of nocturnal emissions, examining the physiological processes, cultural interpretations, and modern perspectives surrounding this often-discussed but sometimes misunderstood phenomenon. We’ll uncover the science behind these dreams, trace their symbolic meanings across cultures, and address common concerns and misconceptions….
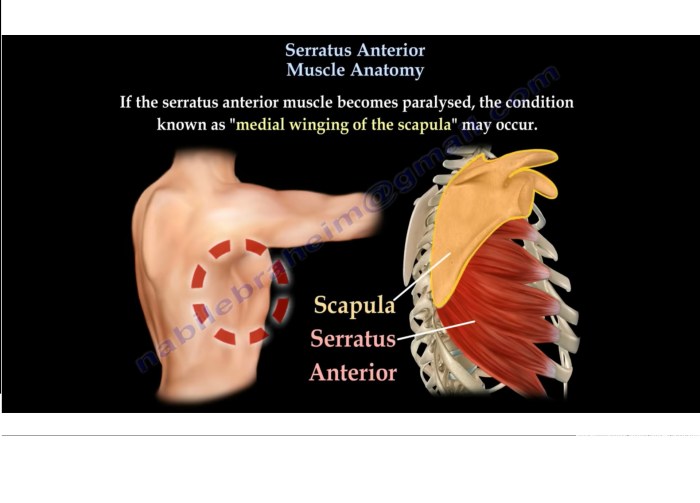
Serratus Anterior Muscle Anatomy A Deep Dive
Serratus anterior muscle anatomy is crucial for understanding upper body movement. This detailed exploration delves into the muscle’s location, function, and intricate relationships with surrounding structures. We’ll examine its origin and insertion points, fiber arrangement, innervation, and blood supply, ultimately connecting these elements to its vital role in actions like pushing, reaching, and protraction. Prepare…