Self collection hpv tests – Self-collection HPV tests offer a new approach to cervical cancer screening. This guide dives deep into the specifics of self-collection HPV tests, examining everything from the available kits and collection methods to the accuracy, accessibility, and ethical considerations surrounding this evolving healthcare practice. Understanding the benefits and potential drawbacks of…
Author: Ceasar Ritchie
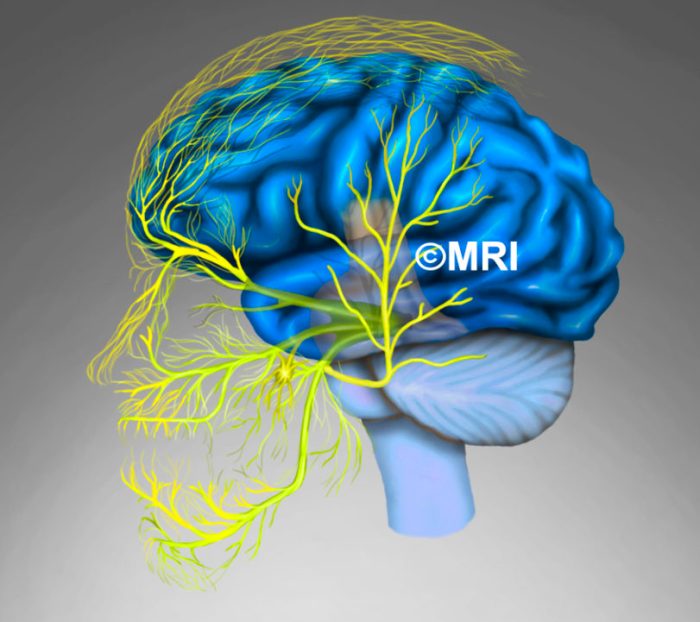
Nerve Block for Migraine A Deep Dive
Nerve block for migraine offers a potential pathway to relief from debilitating headaches. This treatment targets specific nerves believed to be contributing to migraine pain, potentially offering long-term relief or a reduction in attack frequency. Understanding the procedure, efficacy, and potential complications is crucial for informed decision-making. Let’s explore the various types of nerve blocks,…
The Best Vitamin for Fighting Inflammation Unveiling Its Power
The best vitamin for fighting inflammation is a topic of intense interest, and this exploration delves into the science behind it. Inflammation, a natural response to injury or infection, can become chronic, contributing to various health issues. Understanding which vitamins possess potent anti-inflammatory properties is crucial for maintaining well-being. This in-depth look will examine the…
Leg Strength and Brain Health A Powerful Connection
Leg strength and brain health are intricately linked. This blog post explores the fascinating relationship between the power in your lower body and the cognitive functions in your brain. We’ll delve into the physiological mechanisms, examine how specific leg exercises impact memory, attention, and executive functions, and investigate the role of blood flow and neurochemicals…
Breast Cancer Treatment Aging Study A Deep Dive
Breast cancer treatment aging study examines how age impacts the effectiveness and side effects of various therapies. This in-depth exploration considers the diverse factors influencing treatment decisions for patients of different ages, from the available treatment options today to the challenges faced by older adults. It delves into research findings, highlighting the varying responses to…
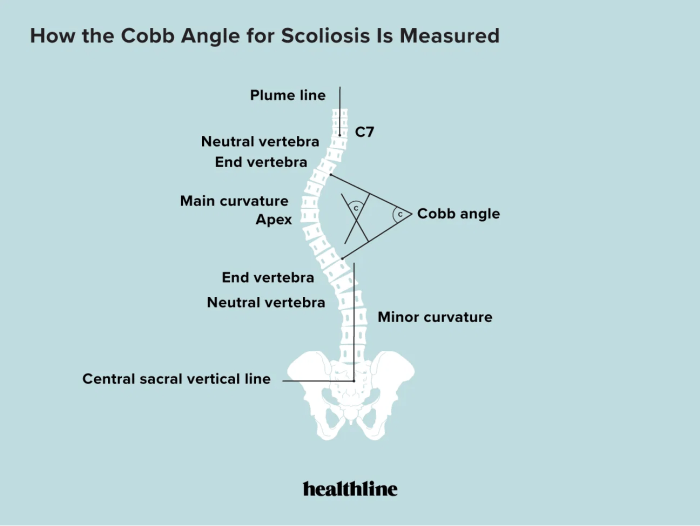
Cobbs Angle and Scoliosis A Deep Dive
Cobbs angle and scoliosis – Cobb’s angle and scoliosis are crucial concepts in understanding spinal deformities. This comprehensive exploration delves into the intricacies of Cobb’s angle, from its definition and significance in diagnosing scoliosis to its role in treatment planning and monitoring progression. We’ll explore different types of scoliosis, measurement methods, and the clinical implications…
Light Therapy Lamps for Sad A Deep Dive
Light therapy lamps for sad offer a unique approach to boosting mood, and this exploration delves into the science and practicalities behind this method. We’ll examine different lamp types, their potential benefits and risks, and how they might fit into your life. This guide will also compare light therapy to other treatment options, provide safety…
Collagen for Rheumatoid Arthritis A Deep Dive
Collagen for rheumatoid arthritis: Understanding this potential treatment option requires a deep dive into the complexities of both conditions. Rheumatoid arthritis, a chronic autoimmune disease, attacks the body’s own tissues, particularly the joints. This inflammation can lead to significant pain, stiffness, and decreased mobility. The body’s natural collagen production, crucial for joint health, may be…
Can You Have Pneumonia Without a Fever?
Can you have pneumonia without a fever? This intriguing question delves into the complexities of pneumonia diagnosis, exploring the nuances of this potentially serious respiratory illness. While fever is often a prominent symptom, there are situations where pneumonia can manifest without this telltale sign. This exploration will unpack the reasons behind this variability, providing a…
Can Allergies Cause a Fever? Understanding the Link
Can allergies cause a fever? This question delves into the intricate relationship between allergic reactions and elevated body temperature. Allergies, encompassing a spectrum of immune responses to foreign substances, often manifest as uncomfortable symptoms like sneezing, itching, and rashes. However, the connection to fever is less straightforward. While a fever is frequently associated with infections,…