Sliced deli meats listeria outbreak has recently garnered significant attention, highlighting the critical need for enhanced food safety protocols. This post delves into the complexities of this issue, exploring the historical context of listeria outbreaks, focusing on the specific risks associated with deli meats, and analyzing the steps taken by regulatory agencies during an investigation….
Author: Ceasar Ritchie
FDA Approves Dissolvable Birth Control Pill
FDA approves dissolvable birth control pill, opening a new chapter in women’s reproductive health. This innovative pill promises a more convenient and potentially more effective way to prevent pregnancy, but what are the implications for patients, healthcare, and society as a whole? We’ll explore the details of this FDA approval, delving into the benefits, challenges,…
What Happens to My Body Right After I Die?
What happens to my body right after I die? This exploration delves into the immediate physiological shifts, cellular processes, and external manifestations that mark the transition from life to death. We’ll examine the cascade of events, from the cessation of brain function to the visible signs of rigor mortis, livor mortis, and algor mortis. The…
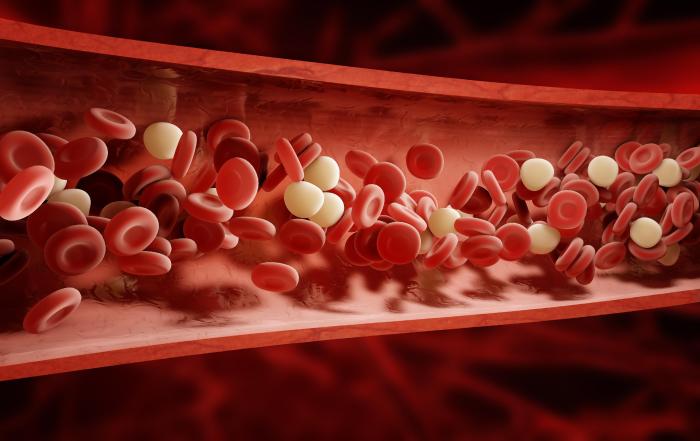
Blood Glucose Test Strips Levels and Process Explained
Blood glucose test strips levels and process are crucial for managing blood sugar. This exploration dives into the world of these strips, from their function and various types to understanding the results and managing fluctuations. We’ll cover the process, typical levels, and factors influencing blood sugar, ultimately providing a comprehensive guide for effective monitoring. This…
The Lowdown on Jiaogulan A Deep Dive
The lowdown on jiaogulan: Unveiling this ancient herb’s potential health benefits, from its botanical origins to its potential uses in modern wellness. This comprehensive guide explores the rich history, nutritional profile, and potential health benefits of jiaogulan, delving into scientific research and highlighting its unique properties compared to similar herbs. Prepare to learn about its…
The Benefits of Carnosine A Deep Dive
The benefits of carnosine, a naturally occurring compound, are increasingly recognized for its potential impact on muscle function, cellular health, and even neurological well-being. This exploration delves into the science behind carnosine, examining its various roles and potential applications. We’ll uncover how carnosine impacts everything from athletic performance to the aging process. Carnosine, a dipeptide…
Hip Labrum Surgery Is It the Right Treatment?
Hip labrum surgery is it the right treatment? This exploration delves into the complexities of hip labrum tears, examining the various treatment options, from conservative methods to surgical interventions. We’ll explore the causes, symptoms, and diagnostic procedures, providing a comprehensive overview of the factors that influence treatment decisions. Understanding the nuances of hip labrum tears…
Causes of Numbness and Tingling A Deep Dive
Causes of numbness and tingling can range from seemingly minor issues to more serious underlying conditions. This exploration delves into the various factors that can lead to these sensations, from common vitamin deficiencies to more complex neurological problems. Understanding these causes is crucial for proper diagnosis and treatment. We’ll examine everything from peripheral neuropathy, a…
Knee Pain Straightening Leg Trouble
Pain in back of knee when straightening leg can be a debilitating issue, impacting daily activities and quality of life. This comprehensive guide delves into the possible causes, associated symptoms, risk factors, diagnostic procedures, treatment options, self-care measures, and when to seek professional help for this specific knee discomfort. Understanding the various anatomical structures in…
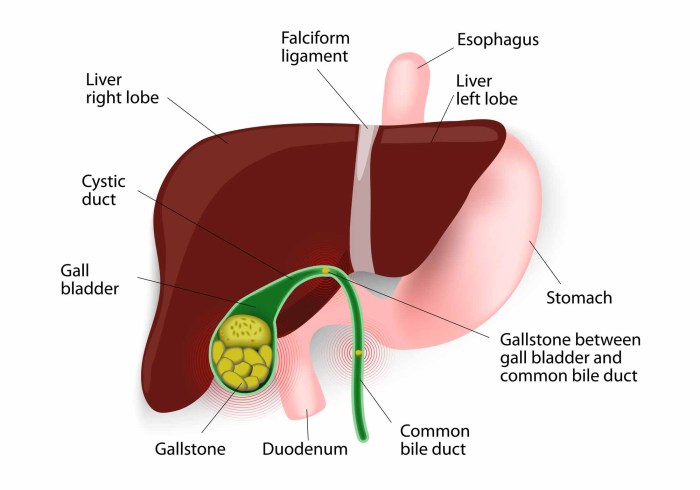
Gallbladder Disease Causes and Risk Factors
Gallbladder disease causes and risk factors are multifaceted, encompassing lifestyle choices, genetics, and underlying medical conditions. Understanding these elements is crucial for proactive health management. This exploration delves into the interplay of diet, obesity, family history, and other influences that contribute to gallbladder issues. We’ll examine the role of various factors in increasing your risk…