How to pick a soap to wash your face is a crucial step in skincare. Different skin types, soap ingredients, and even the formulation itself all play a vital role in achieving healthy, radiant skin. This guide will walk you through everything you need to know, from understanding your skin type to selecting the right…
Author: Carlos Schuster
Bone Modifying Drugs for Cancer with Bone Metastases A Comprehensive Guide
Bone modifying drugs for cancer with bone metastases are crucial in managing the debilitating effects of this condition. These drugs work by targeting the complex interactions between cancer and bone tissue, offering a targeted approach to alleviate pain, reduce bone loss, and potentially improve patient outcomes. Understanding their mechanisms of action, various types, and potential…
List of Starchy Vegetables A Deep Dive
Kicking off with a list of starchy vegetables, this post delves into the fascinating world of these nutrient-rich foods. From potatoes and sweet potatoes to corn and cassava, we’ll explore their nutritional value, culinary uses, and even their environmental impact. Get ready to discover the diverse ways these staples contribute to a healthy and balanced…
Yoga Stretches for Flexibility Your Guide
Yoga stretches for flexibility are a fantastic way to increase your range of motion and improve your overall well-being. This comprehensive guide explores various yoga poses, from fundamental stretches to advanced techniques, to help you achieve greater flexibility. We’ll delve into different types of yoga, safety considerations, and methods to maintain your newfound flexibility. Whether…
What Cold Fingers Mean A Deep Dive
What cold fingers mean goes beyond simple chill. This exploration delves into the diverse factors that can cause those icy extremities, from underlying medical conditions to environmental triggers and even lifestyle choices. Understanding the potential causes of cold fingers is crucial for recognizing potential problems and taking appropriate steps to maintain your well-being. We’ll examine…
Benefits of Black Tea A Deep Dive
Benefits of black tea is a captivating journey into the world of this beloved beverage. From its rich history and diverse preparation methods to its potential health benefits and sensory experience, we’ll explore the multifaceted nature of black tea. Discover why this classic drink is more than just a comforting ritual; it may hold surprising…
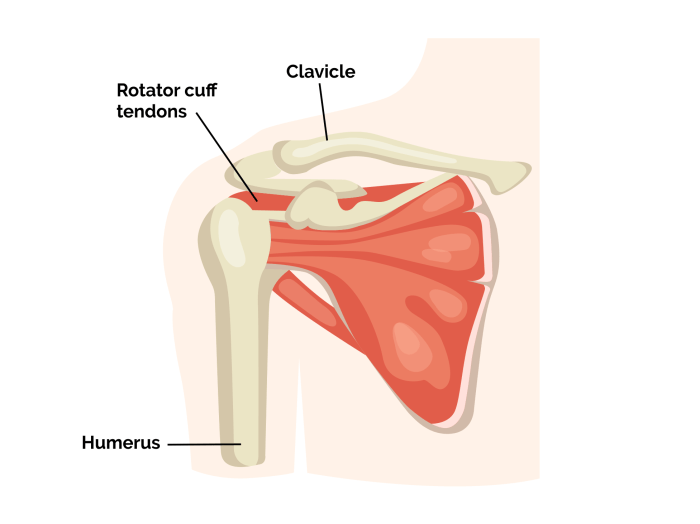
Rotator Cuff Tear Surgery A Comprehensive Guide
Rotator cuff tear surgery is a significant procedure that addresses a common shoulder ailment. Understanding the different types of tears, the diagnostic process, surgical techniques, and the crucial role of rehabilitation is essential for anyone considering this option. This comprehensive guide will delve into the intricacies of rotator cuff tear surgery, exploring everything from the…
Finding the Best Doctor for Elderly Mother
Finding the best doctor for elderly mother is a crucial decision that demands careful consideration. It’s not just about finding someone who’s qualified, but about finding a doctor who understands and respects the unique needs of aging individuals. This involves looking at various factors, from location and insurance coverage to the doctor’s experience with elderly…
How Much Muscle Can You Gain in a Month?
How much muscle can you gain in a month? The answer isn’t a simple number, as it hinges on various factors like your genetics, training intensity, nutrition, and recovery. This exploration delves into the science behind muscle growth, offering practical strategies for maximizing your potential in a month, while also acknowledging realistic limitations. We’ll unpack…
How Herbs Affect Thyroid Disease
How herbs can affect thyroid disease is a complex and fascinating area of study. Thyroid function is crucial for many bodily processes, and imbalances can lead to a range of symptoms. Understanding how certain herbs might interact with the thyroid gland, whether positively or negatively, is essential for anyone considering using them to support their…