Delsym vs robitussin how do they differ – Delsym vs Robitussin: how do they differ? This in-depth look explores the nuances between these common cough medications, delving into their active ingredients, dosages, potential side effects, and formulations. We’ll also examine their efficacy, cost, and appropriate usage for various situations, including children. Understanding these differences can…
Author: Carlos Schuster
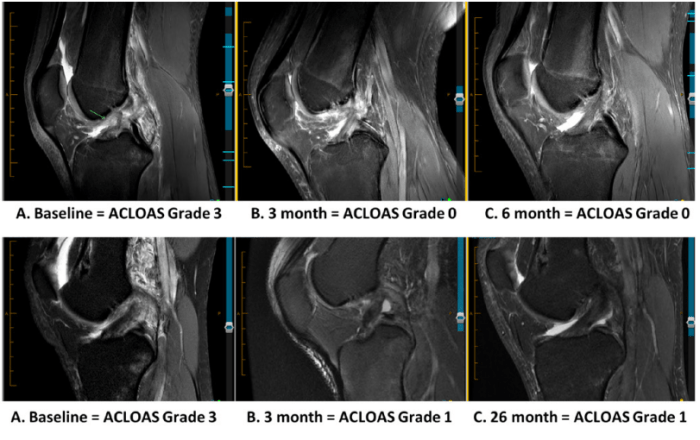
ACL Tears After Surgery A Comprehensive Guide
ACL tears after surgery present a unique challenge, requiring careful consideration of the recovery process. This guide delves into the complexities of ACL reconstruction, from surgical techniques to potential complications and the crucial role of post-surgical rehabilitation. Understanding the nuances of this journey is key to successful outcomes. Anterior cruciate ligament (ACL) tears are a…
Lung Cancer with EGFR Mutation A Comprehensive Guide
Lung cancer with an EGFR mutation is a specific type of lung cancer driven by abnormal growth signals. This condition requires a nuanced understanding of the EGFR protein’s role in healthy lung cells, how mutations disrupt this function, and the diverse mutations themselves. Understanding the different types of EGFR mutations, along with their prevalence and…
Self-Insured Health Insurance A Deep Dive
What is self insured health insurance and how is it regulated – What is self-insured health insurance and how is it regulated? This exploration delves into the intricacies of self-funded healthcare plans, examining their unique characteristics, funding models, regulatory landscape, and risk management strategies. Understanding these nuances is crucial for businesses and individuals considering this…
OTC Migraine & Tension Headaches Your Guide
OTC medications migraine tension are a common first line of defense against those pesky headaches. This guide delves into various over-the-counter options, from understanding their mechanisms of action to potential side effects and crucial safety precautions. We’ll also explore alternative and complementary treatments, self-management strategies, and specific considerations for different populations. Let’s navigate this world…
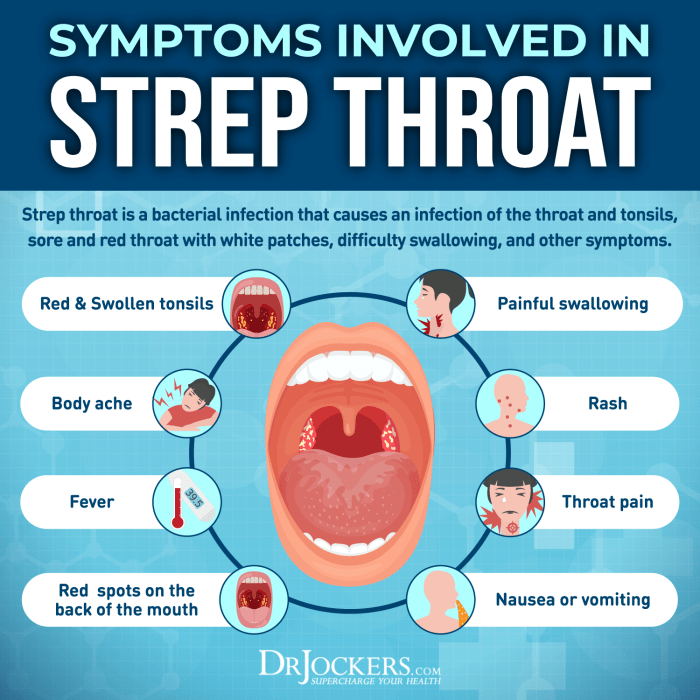
Feeling of Something Stuck in Throat Causes & Solutions
Feeling of something stuck in throat can be incredibly uncomfortable and worrisome. This blog post dives deep into the possible causes, from everyday irritants to more serious medical conditions. We’ll explore potential triggers, diagnostic considerations, management strategies, and preventive measures to help you understand this common issue. From anxiety to specific foods, a variety of…
How Much Vitamin C Per Day Your Daily Dose Guide
How much vitamin C per day do you actually need? This guide dives deep into the daily recommended intake, exploring the factors that influence your personal requirements. We’ll uncover the differences between RDA and UL, and provide a clear, easy-to-understand table summarizing recommended daily allowances for various age groups and genders. Plus, discover the amazing…
Learn About Insurance Codes to Avoid Billing Errors
Learn about insurance codes to avoid billing errors is crucial for anyone involved in healthcare, whether you’re a patient, a provider, or an administrator. Understanding these codes ensures accurate billing, prevents costly errors, and ultimately protects everyone’s financial well-being. Incorrect coding can lead to claim rejections, delayed payments, and significant financial burdens for patients. This…
Can Antibiotics Cause Yeast Infections? Intor
Can antibiotics cause yeast infections intor? This is a common concern for people taking antibiotics, as these powerful drugs can disrupt the delicate balance of bacteria in the body. Understanding how antibiotics work and their potential impact on the gut microbiome is crucial in navigating this issue. This post will delve into the mechanisms by…
Herpes Rash on Body Understanding the Signs
Herpes rash on body can be a confusing and sometimes distressing condition. It’s important to understand the different types of herpes that can cause a rash, the typical locations on the body, and the various symptoms. This guide will explore the causes, symptoms, diagnosis, treatment, prevention, and potential complications associated with herpes rashes. This comprehensive…