Weeping eczema overview and more delves into the complexities of this skin condition, offering a comprehensive understanding of its causes, symptoms, and management. We’ll explore everything from the underlying triggers to effective treatments and preventive strategies. Prepare to gain valuable insights into this common yet often challenging skin issue. This comprehensive guide covers the full…
Author: Carlos Schuster
Taking Lexapro First Week Insights
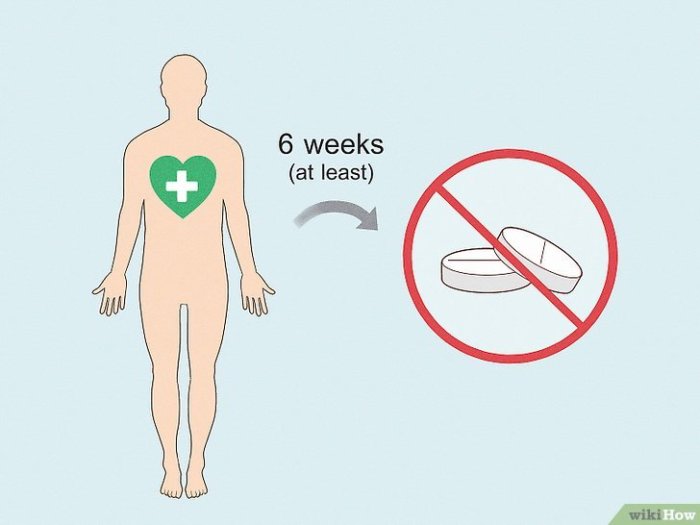
Taking lexapro what to expect in the first week – Taking Lexapro: What to Expect in the First Week? This journey into the first week of Lexapro use delves into potential side effects, possible benefits, and crucial considerations. We’ll explore common symptoms, potential improvements, and vital precautions to navigate this initial phase effectively. Prepare for…
Does Walking Build Muscle? A Deep Dive
Does walking build muscle? The answer isn’t a simple yes or no. Walking, a low-impact exercise accessible to most, can indeed contribute to muscle development, but the extent depends on several factors. This exploration delves into the relationship between walking and muscle building, examining various walking styles and intensities, and comparing them to other forms…
Does Birth Control Stop Ovulation? The Truth Revealed
Does birth control stop ovulation? This question is central to understanding how these methods work. We’ll explore the intricate hormonal mechanisms behind ovulation, how various birth control types interfere with this process, and examine the effectiveness and potential side effects of different approaches. From the common pill to more modern methods, we’ll delve into the…
How Food Allergy is Treated A Comprehensive Guide
How food allergy is treated is a multifaceted approach encompassing avoidance strategies, medical interventions, dietary management, and emergency preparedness. This guide delves into the complexities of food allergies, exploring the various ways individuals can effectively manage their condition and maintain a healthy lifestyle. From understanding the causes and symptoms to exploring the latest advancements in…
Sebaceous Hyperplasia Causes, Symptoms, and Treatments
Sebaceous hyperplasia causes symptoms and treatments are explored in detail. This comprehensive guide dives into the causes, symptoms, and various treatment options for sebaceous hyperplasia, a common skin condition. We’ll examine the underlying reasons for its development, the visible signs it presents, and the different approaches to managing it. Understanding this condition empowers individuals to…
The Benefits of Rutin Supplements A Deep Dive
The benefits of rutin supplements are gaining traction in health circles. This comprehensive exploration delves into the potential advantages of incorporating rutin into your daily regimen. We’ll examine its sources, forms, dosages, and potential health benefits, while also addressing potential risks and side effects. Rutin, a naturally occurring flavonoid, is found in various fruits and…
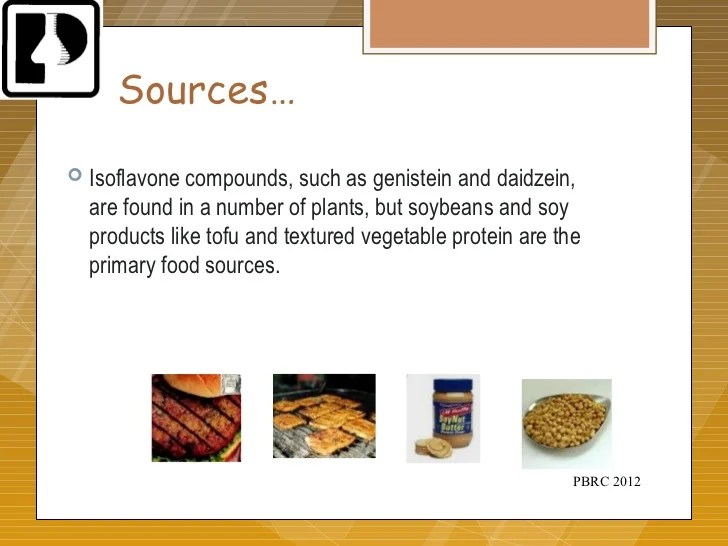
Isoflavones Benefits Side Effects, Dosage, and Interactions
Isoflavones benefits side effects dosage and interactions are a complex topic, but understanding the nuances can be key to harnessing their potential. These plant compounds, found in various foods, are gaining attention for their potential health benefits. However, it’s crucial to consider the potential side effects, appropriate dosage, and possible interactions with other substances. This…
Sun Sensitivity During Chemotherapy A Comprehensive Guide
Sun sensitivity during chemotherapy sets the stage for a crucial discussion about managing this common side effect. Understanding the mechanisms behind this sensitivity, recognizing the symptoms, and implementing preventative strategies are all key to navigating this challenging time. This comprehensive guide will cover everything from the science behind sun sensitivity to practical tips for managing…
Is White Bread Bad for You? A Deep Dive
Is white bread bad for you? This question delves into the nutritional profile, potential health risks, and even the cultural context surrounding this seemingly simple food. We’ll explore the nutritional breakdown, examining carbohydrates, protein, and vitamins, and comparing it to whole-wheat alternatives. We’ll also discuss the glycemic index, potential weight gain concerns, and digestive health…