Running for weight loss is a fantastic way to shed those extra pounds and improve your overall health. This comprehensive guide dives into the science behind running’s effectiveness, outlining various running types, essential training plans, and crucial nutrition and hydration strategies. We’ll explore the gear you need, how to monitor your progress, and how to…
Author: Carlos Schuster
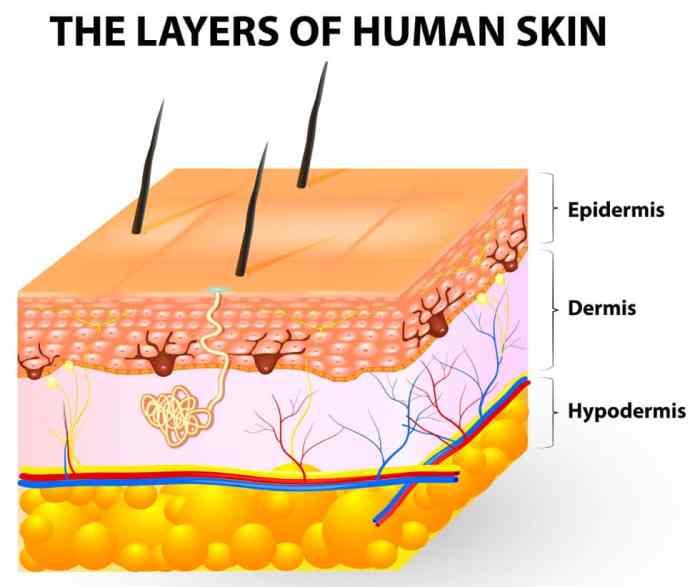
What are Skin Tag Patches? A Comprehensive Guide
What are skin tag patches? They’re small, adhesive plasters designed to cover and potentially resolve skin tags. This comprehensive guide explores various types, application methods, ingredients, effectiveness, safety precautions, and comparisons to other removal methods. We’ll delve into the science behind these patches, offering a clear picture of their benefits and drawbacks. Learn everything you…
Disc Extrusion, Protrusion, and Sequestration A Deep Dive
Disc extrusion protrusion and sequestration – Disc extrusion, protrusion, and sequestration are common spinal conditions. This comprehensive guide delves into the intricacies of each, from defining the terms to exploring treatment options and long-term outcomes. Understanding the anatomical location, causes, symptoms, and management strategies is crucial for anyone seeking information about these spinal issues. The…
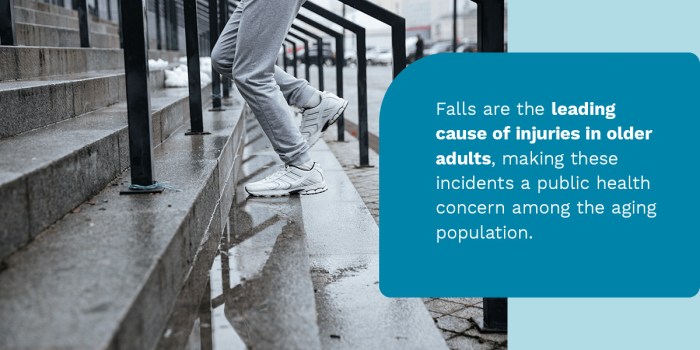
Preventing Falls in Older Adults (USPSTF)
Prevent fall risk in older adults uspstf guidelines offer crucial insights into reducing the significant threat of falls among seniors. Understanding the recommendations from the US Preventive Services Task Force (USPSTF) is essential for healthcare professionals and caregivers to proactively address this public health concern. Falls can lead to serious injuries, impacting both physical and…
Acting Out Dreams Dementia & Parkinsons Link
Acting out dreams predicts later dementia parkinsons – Acting out dreams predicts later dementia and Parkinson’s, a fascinating and potentially crucial link emerging from recent research. This phenomenon, where individuals physically act out their dreams during sleep, may serve as an early indicator of these neurodegenerative diseases. Understanding the types of dream enactment behaviors, their…
Acute Trauma vs Chronic Trauma Understanding the Differences
Acute trauma vs chronic trauma: This exploration delves into the distinct impacts of sudden, intense experiences versus ongoing, pervasive stress. Understanding these differences is crucial for providing appropriate support and treatment. We’ll examine the physiological and psychological responses, the developmental effects, and the various treatment approaches. Acute trauma often stems from a single, shocking event…
Are Yeast Infections Contagious? A Deep Dive
Are yeast infections contagious? This question is crucial for understanding how these common infections spread and how to protect yourself. Yeast infections, often characterized by uncomfortable symptoms, can affect various parts of the body. Understanding the transmission mechanisms and contagiousness factors is key to preventing infections and managing them effectively. This in-depth look at yeast…
How to Increase Lung Capacity Your Guide
How to increase lung capacity is a journey to better respiratory health, opening doors to enhanced athletic performance and overall well-being. Understanding the factors influencing lung capacity, from breathing techniques to lifestyle choices, is key to unlocking your body’s full potential. This guide delves into various aspects, from the science behind breathing exercises to the…
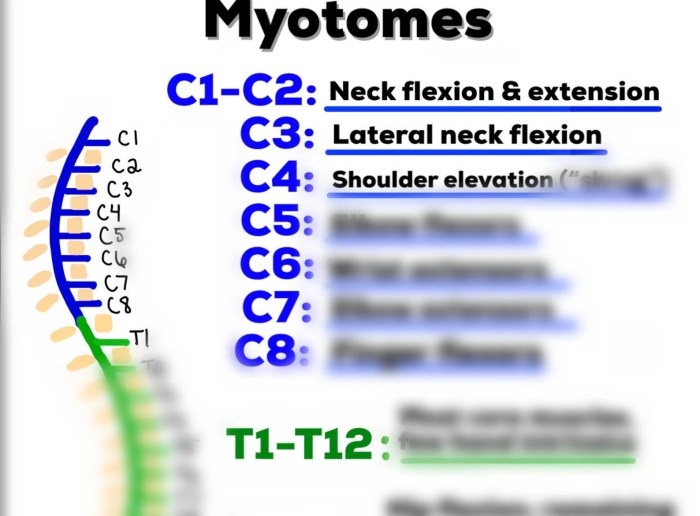
What is a Myotome A Deep Dive
What is a myotome? It’s a crucial concept in understanding how our muscles are controlled by the nervous system. Imagine a specific group of muscles, all working together, coordinated by a particular segment of the spinal cord. That’s essentially a myotome. This isn’t just an academic curiosity; myotome assessment plays a vital role in diagnosing…
What Are the First Signs of the Flu?
What are the first signs of the flu sets the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail and brimming with originality from the outset. Understanding the early indicators of influenza is crucial for prompt action and effective management. This comprehensive guide delves into the initial…