Why do I have a summer cold? This common ailment often strikes during the warmer months, leaving us feeling miserable. Understanding the causes and triggers is key to preventing and managing these summer illnesses. This post dives into the world of summer colds, exploring viral culprits, environmental factors, personal influences, prevention strategies, and when to…
Author: Anastacio Bogisich
Information and History About Vaccination and Vaccines A Deep Dive
Information and history about vaccination and vaccines sets the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail and brimming with originality from the outset. We’ll journey through time, examining the groundbreaking scientific advancements, the societal impact, and the ongoing challenges and opportunities in the field of…
Pregnant with No Insurance What Now?
Pregnant with no maternity insurance what now – Pregnant with no maternity insurance? What now? This is a critical situation, and facing it alone can feel overwhelming. This guide will explore the challenges, financial resources, healthcare options, and legal considerations pregnant individuals without insurance may encounter. We’ll delve into the complexities of navigating this journey,…
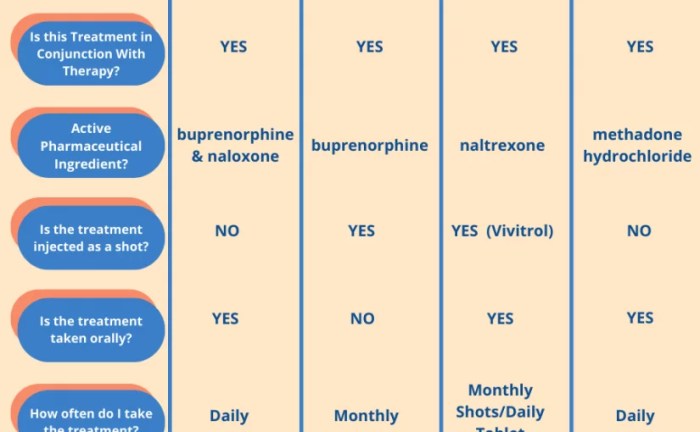
Suboxone vs Methadone How Do They Differ?
Suboxone vs methadone how do they differ? This critical comparison delves into the nuances of opioid substitution therapies (OSTs), examining the distinct mechanisms, administration methods, potential side effects, and ultimately, the suitability of each treatment for individual patients. Understanding the differences is key to making informed decisions about managing opioid use disorder. Opioid substitution therapies,…
Smell and Brain Health A Deep Dive
Smell and brain health are deeply intertwined. Our sense of smell, often overlooked, plays a crucial role in memory, mood, and cognitive function. This exploration delves into the fascinating neural pathways connecting the nose to the brain, uncovering how smells can trigger powerful memories, influence our emotional states, and even impact our overall well-being. We’ll…
Symbicort An Inhaled Asthma Treatment
Symbicort an inhaled asthma treatment for asthma – Symbicort, an inhaled asthma treatment for asthma, is a widely used medication for managing asthma symptoms. This comprehensive guide delves into the specifics of Symbicort, from its active ingredients and mechanism of action to its effectiveness, dosage, potential side effects, and interactions with other medications. We’ll also…
Crohns Flare Hospital Visit Guide
Crohns flare when to go to the hospital – Crohn’s flare when to go to the hospital? This guide dives deep into understanding Crohn’s flare-ups, helping you assess severity and know when urgent medical attention is necessary. We’ll explore common symptoms, escalating indicators, and situations demanding immediate hospital intervention, empowering you to make informed decisions…
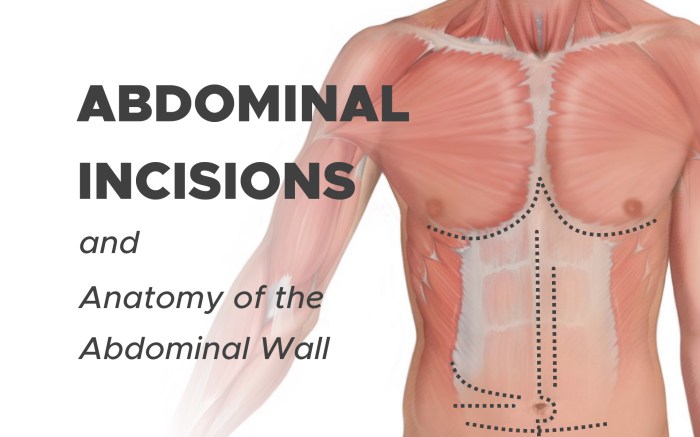
Abdominal Swelling and Bloating Understanding the Causes
Abdominal swelling and bloating can be uncomfortable and frustrating. This comprehensive guide explores the various aspects of this common issue, from defining the symptoms to understanding potential causes, diagnostic procedures, and effective treatment options. We’ll delve into the physiological mechanisms behind the distention, differentiate between types of swelling, and discuss the role of different organs…
Top Causes of Death for Ages 15-24
Top causes of death for ages 15 24 – Top causes of death for ages 15-24 is a critical issue, demanding our attention. This exploration delves into the leading factors contributing to mortality in this demographic, examining global and regional trends. Understanding these trends is essential for public health initiatives, highlighting the various contributing factors…
Eczema and COVID Vaccine A Deep Dive
Eczema and COVID vaccine: This post explores the complex relationship between eczema and the body’s response to COVID-19 vaccines. We’ll delve into potential links between eczema, the immune system, and vaccine reactions. Understanding this interplay is crucial for both individuals with eczema and healthcare professionals. The research examines potential correlations between eczema, vaccination rates, and…