What is a pathogen? This exploration delves into the fascinating world of disease-causing organisms, from the microscopic to the complex. We’ll unravel the mysteries behind these tiny invaders, examining their structures, functions, and the intricate ways they interact with their hosts. Understanding pathogens is crucial for comprehending human health and developing effective strategies to combat…
Author: Anastacio Bogisich
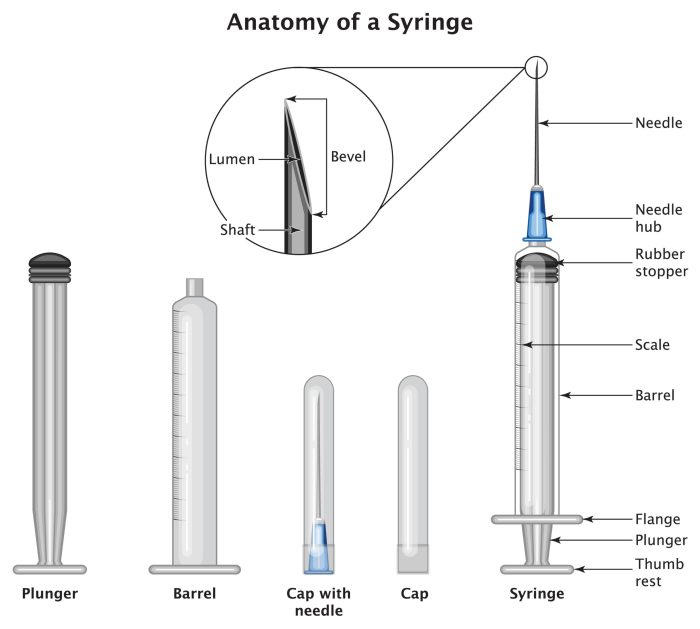
How to Select the Correct Needle Size for an Injection A Comprehensive Guide
How to select the correct needle size for an injection is crucial for patient safety. Using the wrong size can lead to complications, from discomfort to serious health risks. This comprehensive guide will delve into the factors influencing needle size selection, the methods for determining the appropriate gauge, and the essential safety precautions to follow….
My Familys Asthma Journey A Personal Account
My family s journey with asthma – My family’s journey with asthma sets the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail and brimming with personal experiences. We delve into the initial diagnosis, the challenges faced, and the ways we adapted our lives to manage this…
Parkinsons Disease Impact on Relationships
Impact of parkinsons disease on relationships – Impact of Parkinson’s disease on relationships is a multifaceted issue affecting communication, emotional well-being, daily activities, intimacy, finances, decision-making, social support, and expectations. This exploration delves into the profound ways this neurodegenerative disease reshapes interactions within various types of relationships, from spousal and familial bonds to friendships. This…
Why Do I Have Itchy Eyes? Explained
Why do I have itchy eyes? This common problem can be frustrating, impacting daily life and comfort. From pesky allergies to more serious conditions, understanding the causes behind itchy eyes is key to finding relief. This guide delves into the various potential triggers, symptoms, and treatments, helping you pinpoint the source of your discomfort and…
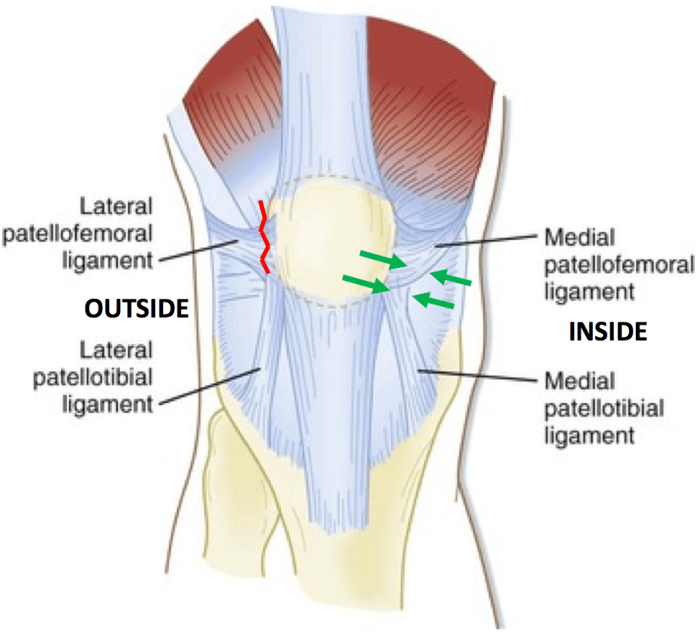
Patella Anatomy Function and Treatment A Deep Dive
Patella anatomy function and treatment is a comprehensive look at the kneecap’s role in movement, potential problems like pain and dislocation, and the various treatment options available. Understanding the patella’s structure, its function in the knee joint, and the different conditions affecting it is crucial for anyone seeking to improve knee health and performance. We’ll…
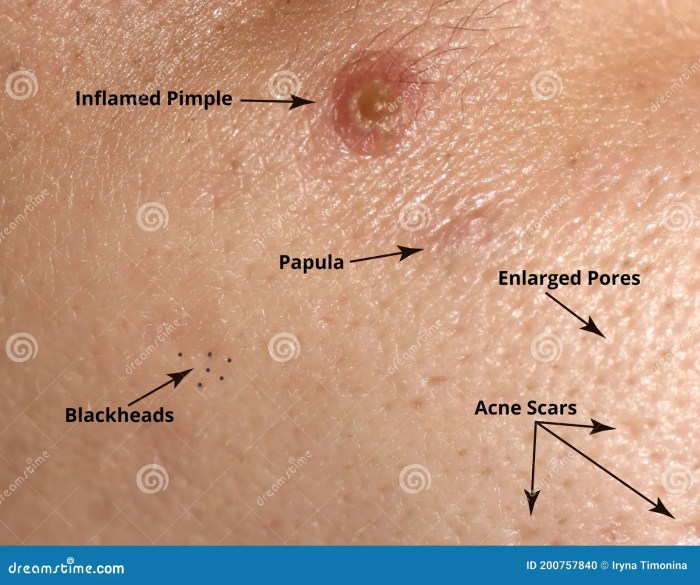
Papule Definition of an Acne Papule A Comprehensive Guide
Papule definition of an acne papule delves into the specifics of this skin condition. Understanding what constitutes an acne papule is key to effective management and treatment. This in-depth exploration covers everything from defining the papule itself to examining its causes, symptoms, and available treatments. Acne papules are small, solid bumps on the skin. They’re…
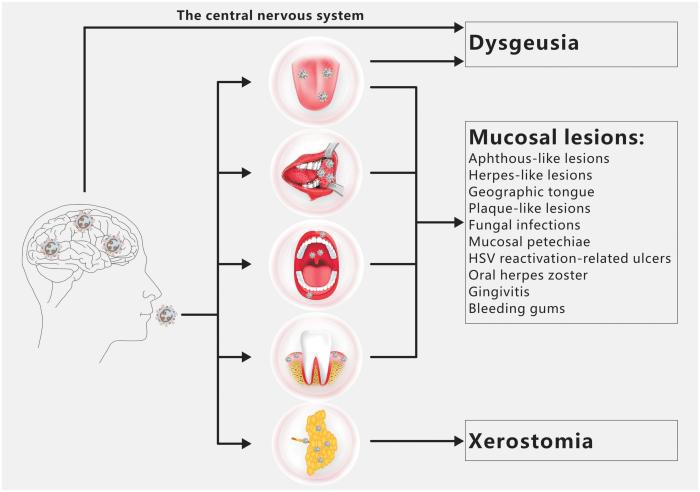
Mouth Swab Drug Test A Comprehensive Guide
Mouth swab drug tests are becoming increasingly prevalent in various settings, from employment to healthcare. This comprehensive guide delves into the specifics of this method, exploring its principles, procedures, results, legal aspects, and comparison to other testing methods. Understanding the nuances of mouth swab drug tests is crucial for both those who administer and those…
How Long Do You Have to Use CPAP?
How long do you have to use CPAP? This crucial question impacts sleep apnea sufferers, impacting their overall health and quality of life. Understanding the factors that influence CPAP treatment duration is essential for informed decision-making. This exploration delves into the various aspects of CPAP therapy, from typical usage durations to the potential long-term benefits…
What to Expect in an MRI A Comprehensive Guide
What to expect in an MRI sets the stage for a detailed look at the entire experience, from preparation to post-scan recovery. We’ll explore everything from the essential pre-scan instructions to the sensations you might feel during the procedure itself. This comprehensive guide will walk you through the steps, highlighting potential anxieties, and offering insights…