Tea tree oil for hair is a natural remedy gaining popularity for its potential benefits. This in-depth guide explores the properties, benefits, and usage of tea tree oil in hair care, examining its historical context, chemical composition, and potential effects on hair follicles. We’ll delve into how it can address various hair concerns and compare…
Author: Anastacio Bogisich
How Long Does COVID Live on Surfaces? A Deep Dive
How long does COVID live on surfaces? This question is crucial for understanding transmission and taking necessary precautions. Different surfaces, environmental factors, and initial viral loads all play a role in the virus’s lifespan. We’ll explore the science behind COVID’s survival, from common household materials to cleaning methods, providing clear insights into its persistence and…
Missed Open Enrollment Period Your Options
Missed open enrollment period? Don’t panic! Understanding the consequences and exploring your options is key to securing the right insurance coverage. This guide delves into the implications of missing the open enrollment period for various insurance types, like health, dental, and vision, and provides a roadmap for navigating the process to get coverage, including special…
Why Do I Sweat So Easily? Understanding the Causes
Why do I sweat so easily? This question plagues many, leading to discomfort and concern. Understanding the underlying reasons for excessive sweating is crucial for finding relief and improving overall well-being. This comprehensive guide explores the medical conditions, lifestyle factors, and physiological mechanisms that contribute to excessive perspiration, providing insights into diagnosis, treatment, and prevention…
Topamax Topiramate for Weight Loss A Comprehensive Guide
Topamax topiramate for weight loss is a controversial topic, and understanding its potential benefits and risks is crucial. This guide delves into the science behind Topamax’s effect on weight, examining clinical trials, patient experiences, and medical professional recommendations. We’ll explore the mechanisms of action, dosage, potential side effects, and compare Topamax to other weight loss…
Night Leg Cramps Understanding and Relief
Leg cramps at night can be incredibly disruptive, jolting you awake with sudden, sharp pain. This post dives deep into understanding these nocturnal muscle spasms, exploring the possible causes, risk factors, and effective home remedies. We’ll also look at when it’s time to seek medical attention for persistent or severe leg cramps. Night leg cramps…
What are Coxsackievirus Infections A Deep Dive
What are coxsackievirus infections? They’re a group of viruses that can cause a range of illnesses, from mild to severe. Understanding these viruses, their different types, how they spread, and the symptoms they cause is key to effective prevention and treatment. This exploration delves into the various aspects of coxsackievirus infections, from their global distribution…
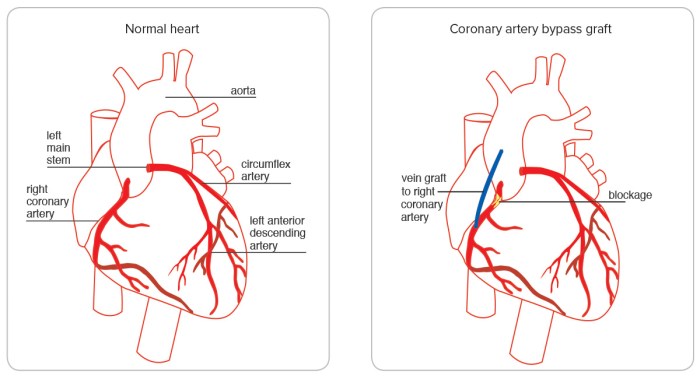
What is Quadruple Bypass Heart Surgery? A Deep Dive
What is quadruple bypass heart surgery? This procedure involves rerouting blood flow around blocked coronary arteries in the heart. It’s a significant surgical intervention, often chosen when other treatments aren’t sufficient. Understanding the details, from the reasons for the surgery to the potential long-term effects, is crucial for anyone considering or learning about this complex…
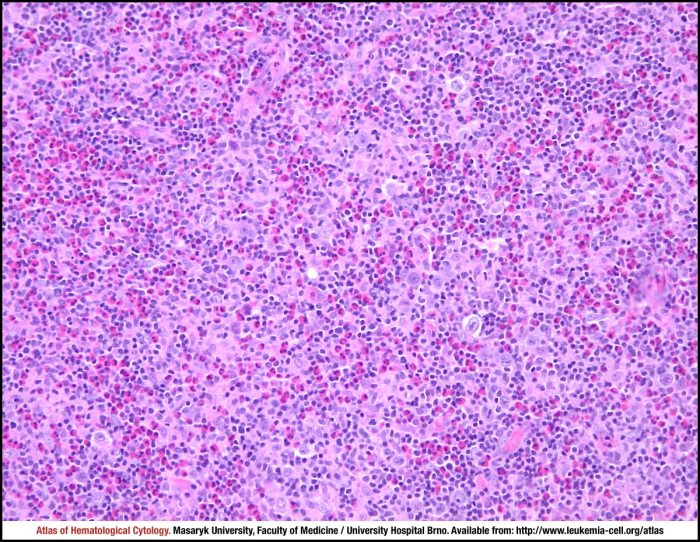
Mixed Cellularity Hodgkin Lymphoma A Deep Dive
Mixed cellularity hodgkins lymphoma – Mixed cellularity Hodgkin lymphoma (MCHL) is a type of blood cancer that requires careful understanding. It’s characterized by the presence of specific abnormal cells, called Reed-Sternberg cells, and other unique histological features. Diagnosing and treating MCHL involves a multifaceted approach, encompassing various diagnostic procedures, treatment strategies, and considerations of prognosis…
Diagnosis and Testing for HER2-Positive Breast Cancer
Diagnosis and testing for her2 positive breast cancer – Diagnosis and testing for HER2-positive breast cancer is crucial for effective treatment. This comprehensive guide delves into the specifics of identifying this aggressive form of breast cancer, from understanding the role of the HER2 protein to the various diagnostic tests used. We’ll explore the nuances of…