How to brush your teeth effectively is crucial for maintaining good oral health. This guide dives deep into the essential steps, from selecting the right tools to mastering the perfect technique. Proper brushing prevents plaque buildup, gum disease, and cavities, leading to a healthier, more confident smile. We’ll explore various techniques for different needs, from…
Author: admin
Fear of Getting Sick A Deep Dive
Fear of getting sick sets the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail and brimming with originality from the outset. This fear, often rooted in psychological factors, can manifest in a variety of ways, impacting everything from daily routines to social interactions. We’ll explore the…
Vitamins to Avoid with Blood Pressure
Vitamins to avoid with blood pressure are crucial for managing hypertension. Certain vitamins, while generally beneficial, can sometimes elevate blood pressure in susceptible individuals. Understanding which vitamins might be problematic, and how to navigate these nuances safely, is key to maintaining cardiovascular health. A balanced diet, coupled with informed decisions about vitamin intake, is essential…
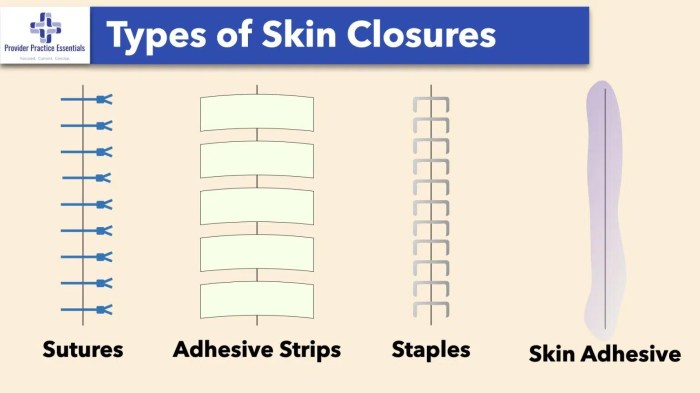
Incision Closed Sutures, Staples, Glue
Incision closed sutures staples glue are critical considerations in surgical procedures. This comprehensive guide delves into the diverse world of surgical closure methods, comparing sutures, staples, and surgical glue in detail. We’ll explore the advantages and disadvantages of each, examining various types of sutures, staple placements, and surgical glue applications. From the initial preparation to…
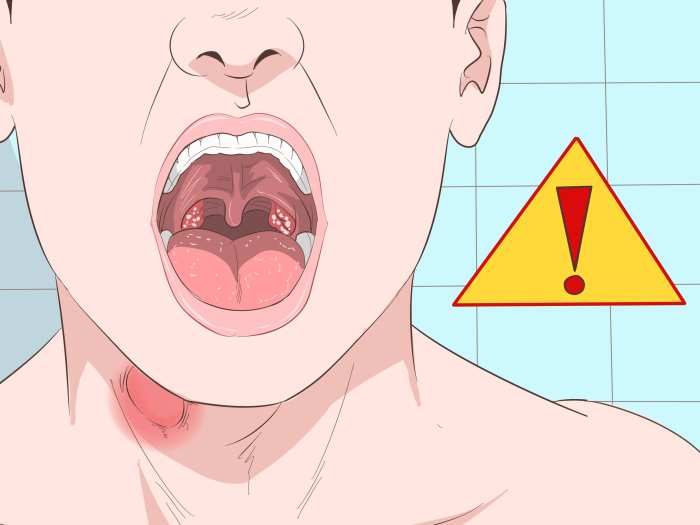
Oral Thrush Home Remedies A Guide
Oral thrush home remedies offer a range of potential solutions for managing this common oral infection. Understanding the causes, symptoms, and various treatment approaches is key to effectively addressing oral thrush at home. This guide explores a variety of natural and practical methods, from dietary changes to oral hygiene practices, to help alleviate symptoms and…
Ask an Expert Self-Diagnosing Atopic Dermatitis
Ask an expert self diagnose atopic dermatitis. This comprehensive guide delves into the intricacies of atopic dermatitis (AD), providing a crucial understanding of its symptoms, triggers, and the limitations of self-diagnosis. We’ll explore the crucial difference between self-assessment and a professional diagnosis, equipping you with the knowledge to make informed decisions about your health. From…
How Long Live Without Food Survival Limits
How long live without food? This question delves into the fascinating, and often grim, realities of human survival in the face of starvation. Our bodies are remarkably resilient, but how long can they withstand the absence of essential nutrients? This exploration examines the complex interplay of physiology, factors influencing survival, consequences of prolonged fasting, and…
How Long Does Ibuprofen Last?
How long does ibuprofen last? This question is crucial for anyone who’s used this common pain reliever. Understanding its duration of action, from absorption to metabolism, is key to getting the most effective relief and avoiding potential side effects. Different factors influence how long ibuprofen stays in your system, impacting everything from the dosage to…
Sore Throat No Fever Causes & Treatment
Sore throat no fever causes and treatment is a common ailment that can be frustrating and concerning. Understanding the potential triggers, from viral infections to environmental irritants, is key to effective management. This comprehensive guide will delve into the various possible causes, symptoms, and treatment options for a sore throat without a fever, empowering you…
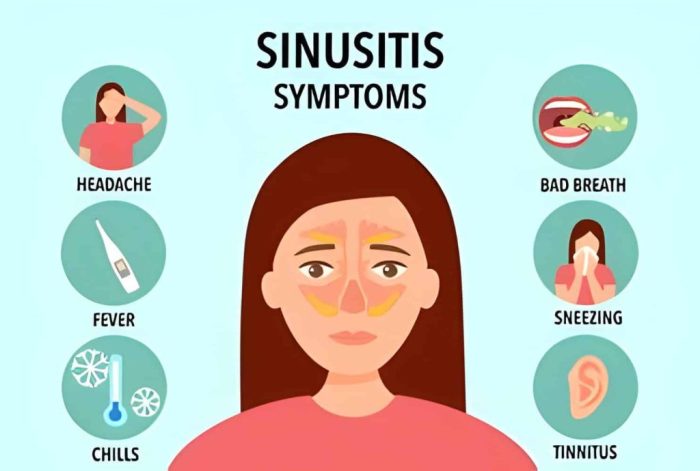
Are Sinus Infections Contagious? Understanding the Risks
Are sinus infections contagious? This question delves into the fascinating world of transmission, exploring how these common ailments spread and how you can protect yourself. We’ll examine the different types of sinus infections, the various ways they might be transmitted, and the crucial period when someone with a sinus infection is most likely to spread…