The benefits of arnica, a plant with a long history of use in traditional medicine, are now being explored through a modern lens. This comprehensive exploration delves into the various forms of arnica, its purported healing properties, and the scientific evidence behind its use. From muscle soreness to joint pain, we’ll examine how arnica might…
Author: admin
Whole Food Plant-Based Diet A Deep Dive
Whole food plant based diet – The whole food plant-based diet sets the stage for a fascinating exploration into a lifestyle that prioritizes whole, unprocessed plant foods. This approach isn’t just about what you eat; it’s about understanding the core principles, nutritional benefits, potential risks, and practical applications of this dietary philosophy. We’ll delve into…
LASIK Side Effects What to Expect
What side effects can I expect after LASIK? This comprehensive guide dives into the potential short-term and long-term effects of laser eye surgery. From the initial recovery period to possible complications, we’ll explore the factors influencing outcomes and strategies for managing any issues that may arise. Understanding the risks and benefits of LASIK is crucial…
Coughing Up Mucus COVID Understanding the Symptoms
Coughing up mucus COVID is a significant concern for those affected. This detailed exploration delves into the characteristics of this symptom, examining the various consistencies, colors, and volumes of mucus produced throughout the illness. We’ll compare it to other respiratory ailments, offering a clear picture of what to expect. Understanding the different stages and how…
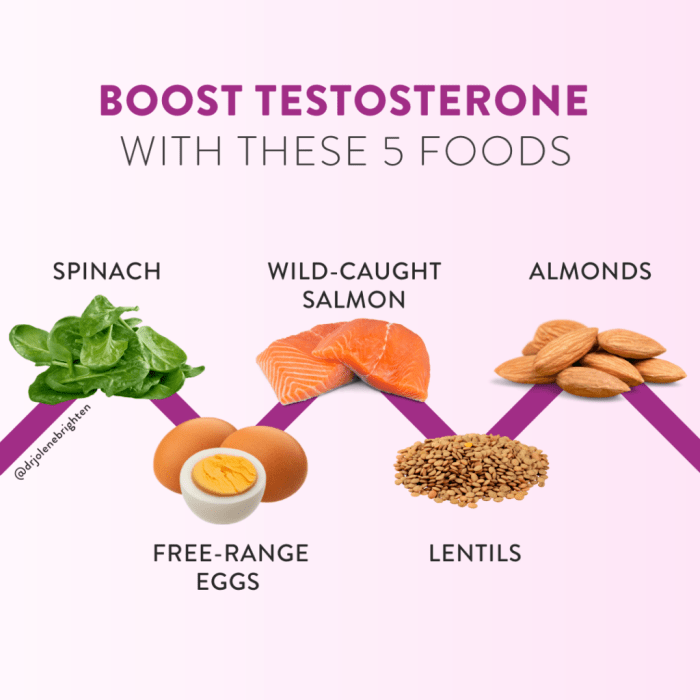
Low Testosterone in Women A Deep Dive
Low testosterone in women sets the stage for this enthralling narrative, offering readers a glimpse into a complex hormonal landscape. We’ll explore the intricacies of low testosterone levels in women, delving into its various definitions, measurement methods, and the diverse factors that influence them. From understanding the typical ranges to identifying potential symptoms and underlying…
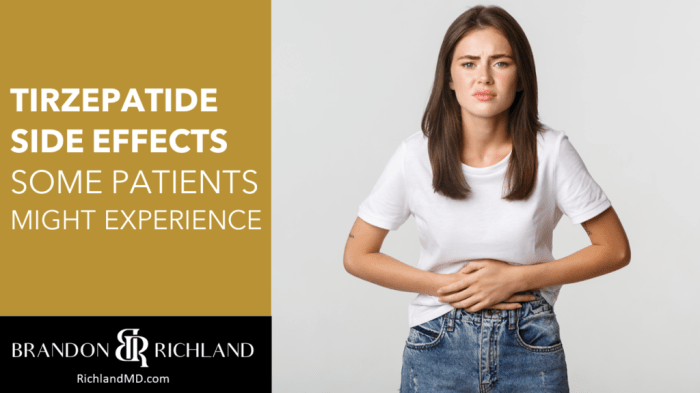
Zepbound Tirzepatide Diabetes Risk A Deep Dive
Zepbound tirzepatide diabetes risk is a critical area of concern for those managing diabetes. This in-depth look examines the potential risks associated with tirzepatide, a medication increasingly used to control blood sugar. We’ll explore its mechanism of action, potential side effects, risk factors, and the latest research. Understanding these risks is crucial for informed decision-making…
Risks of Sitting Too Long A Health Hazard
Risks of sitting too long can lead to a multitude of health problems, impacting both physical and mental well-being. From musculoskeletal issues to cardiovascular risks, and even mental health concerns, understanding the dangers of prolonged sitting is crucial for maintaining a healthy lifestyle. This exploration delves into the various facets of this sedentary habit, highlighting…
Hot Toddy for Cough A Cozy Remedy
Hot toddy for cough, a comforting beverage steeped in history, offers a potential solution for soothing coughs. This traditional drink, often associated with winter evenings, combines warming spices, comforting ingredients, and sometimes a touch of alcohol to provide relief. We’ll explore the history, variations, potential benefits, and risks of this age-old remedy. From understanding the…
Triple Negative Breast Cancer Recurrence After Mastectomy
Triple negative breast cancer recurrence after mastectomy is a complex and challenging medical issue, demanding careful consideration of the biological mechanisms driving recurrence, clinical manifestations, treatment strategies, patient outcomes, and the essential support systems for affected individuals. This detailed exploration delves into the intricacies of this specific form of breast cancer recurrence, highlighting the unique…
Post-Surgery Urinary Retention What to Do
What to do if you cant urinate after surgery – What to do if you can’t urinate after surgery? This comprehensive guide delves into the causes, immediate actions, medical interventions, prevention strategies, and recovery process. Understanding the potential complications and knowing what steps to take is crucial for a smooth post-operative recovery. From recognizing the…