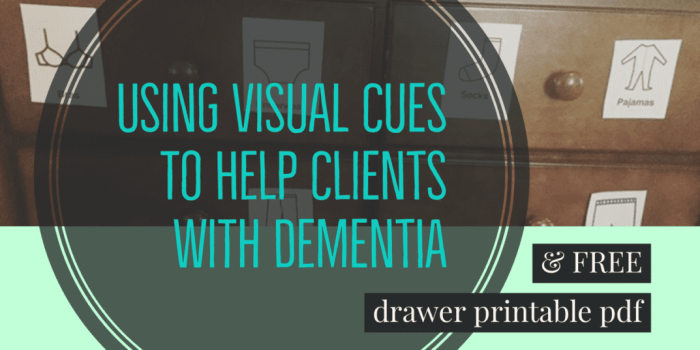
Visual clues to dementia diagnosis are subtle yet significant indicators that can aid in early detection. This blog post explores the various visual cues potentially associated with dementia, ranging from subtle changes in facial expressions to alterations in posture and eye contact. Understanding these visual indicators can be crucial for early intervention and support for…
Author: admin
Ligyrophobia Fear of Loud Noises
Ligyrophobia fear of loud noises – Ligyrophobia, fear of loud noises, can significantly impact a person’s life, from everyday interactions to their overall well-being. This fear isn’t just about a dislike for boisterous sounds; it’s a complex phobia that triggers intense physical and emotional responses. Understanding the causes, symptoms, and coping mechanisms is crucial for…
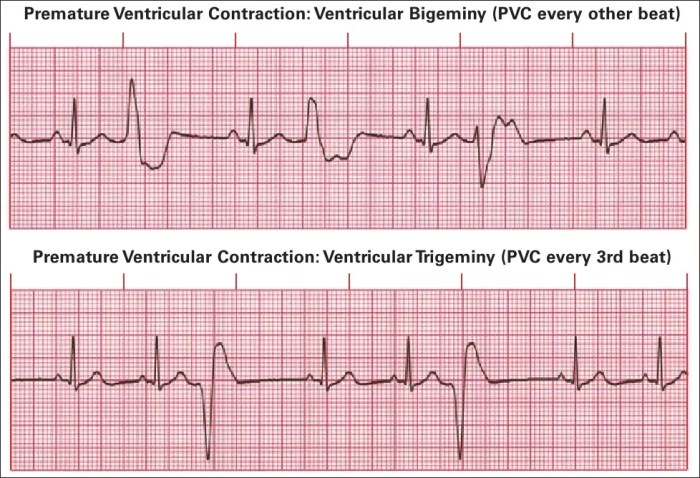
Understanding Premature Ventricular Complexes (PVCs)
Premature ventricular complexes pvcs – Premature ventricular complexes (PVCs) are a common cardiac rhythm disturbance. This in-depth look explores PVCs, from their definition and characteristics to potential causes, symptoms, diagnosis, management, and complications. We’ll delve into the electrical mechanisms behind PVCs, the role of various factors, and the importance of patient education. PVCs, often benign,…
Does Milk Make You Taller? Unveiling the Truth
Does milk make you taller? This age-old question sparks curiosity and debate. We’ll delve into the intricate relationship between milk consumption and height, exploring the science behind growth and development, the nutritional value of various milk types, and the evidence from scientific studies. This exploration promises to shed light on whether that glass of milk…
Magnesium for Muscle Pain A Deep Dive
Magnesium for muscle pain is a crucial topic for understanding the role of this vital mineral in maintaining healthy muscles. Magnesium plays a significant part in muscle function, and deficiencies can lead to a range of issues, including persistent muscle aches and discomfort. This article explores the intricate connection between magnesium and muscle pain, examining…
Papilledema Symptoms Causes, Diagnosis, and Treatment
Papilledema symptoms causes diagnosis treatment – Papilledema symptoms, causes, diagnosis, and treatment are crucial for understanding this potentially serious condition. This comprehensive guide delves into the various visual and non-visual symptoms, exploring the underlying causes from intracranial pressure to tumors. We’ll examine diagnostic methods, from ophthalmoscopy to imaging, and discuss the diverse treatment approaches, from…
Secondary Headache Overview and More Understanding the Causes
Secondary headache overview and more delves into the complexities of headaches beyond the familiar. This exploration examines the crucial distinction between primary headaches, often idiopathic, and secondary headaches, where an underlying medical condition triggers the pain. Understanding the causes, symptoms, and diagnostic processes is key to effective management and treatment. Knowing how to differentiate these…
Hypoactive Sexual Desire Disorder A Comprehensive Guide
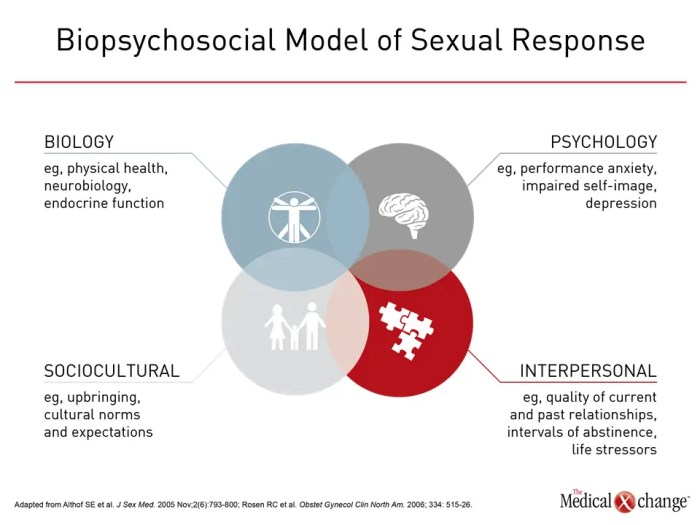
Hypoactive sexual desire disorder symptoms causes diagnosis treatment and coping is a multifaceted issue affecting many individuals. This in-depth exploration delves into the complexities of this condition, examining its symptoms, potential causes, diagnostic processes, available treatments, and effective coping strategies. We’ll cover the nuances of low libido versus HSDD, exploring the biological, psychological, and relational…
Cardiac Effects of Obesity Medications A Deep Dive
Cardiac effects of obesity medications are a crucial area of study, as these drugs can potentially impact the cardiovascular system. This blog post explores the different classes of obesity medications currently available, examining their mechanisms of action and potential physiological pathways through which they might affect the heart. We’ll delve into the potential cardiac risks…
Julie Scott ANP BC A Deep Dive
Julie Scott ANP BC, an Advanced Nurse Practitioner in British Columbia, brings a wealth of experience and expertise to the field. This profile delves into her professional journey, highlighting her education, specializations, and extensive experience. We’ll explore her scope of practice in BC, community involvement, patient care approach, current activities, and the public perception of…