All about hypertension diagnosis: Understanding high blood pressure is crucial for maintaining good health. This in-depth guide explores the complexities of diagnosing hypertension, from initial evaluation to specialized testing and considerations for specific populations. We’ll delve into the different methods, from clinical assessments to lab tests, and provide a clear picture of the diagnostic process.
This exploration of hypertension diagnosis will equip you with a solid understanding of the various stages, risk factors, and essential components of a thorough evaluation. We’ll also discuss the critical importance of accurate measurements, the role of lifestyle factors, and the interpretation of laboratory results. Furthermore, the guide will cover the nuances of diagnosing hypertension in diverse populations, highlighting the importance of personalized approaches.
Introduction to Hypertension Diagnosis
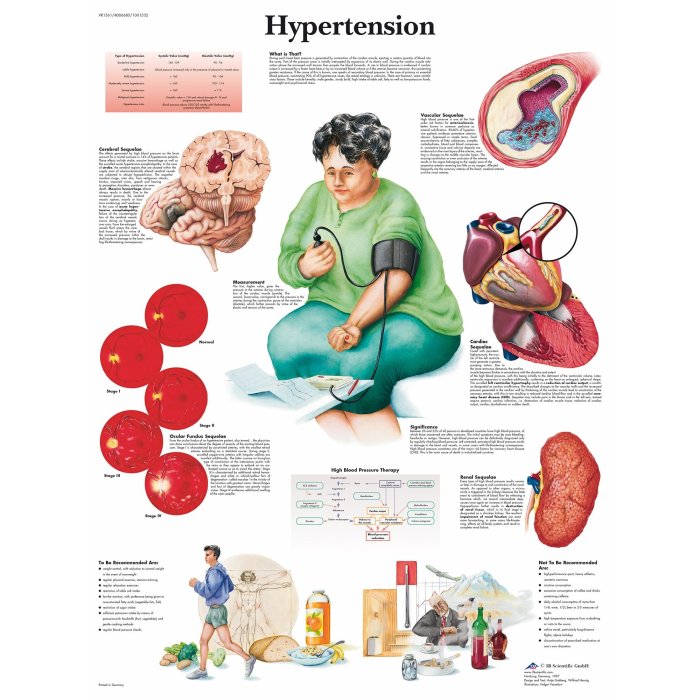
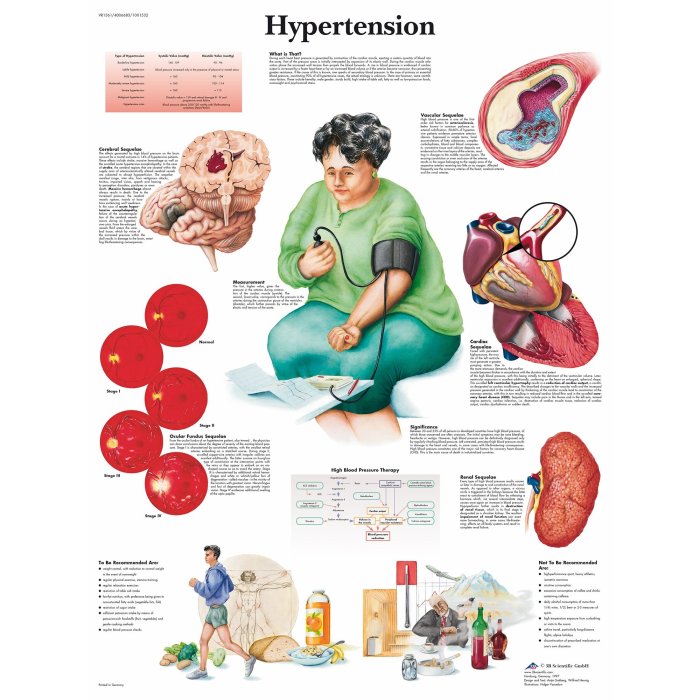
High blood pressure, or hypertension, is a significant public health concern globally. It’s a condition where the sustained force of blood against artery walls is elevated, increasing the risk of serious health problems like heart disease, stroke, and kidney failure. The long-term nature of hypertension and its often silent progression make early detection and management crucial. Understanding the stages of hypertension and the associated risk factors is vital for effective prevention and treatment.Elevated blood pressure can lead to significant health complications, and its management is a crucial component of public health initiatives.
Early diagnosis, along with lifestyle modifications and appropriate medication, can significantly reduce the risk of severe health outcomes.
Stages of Hypertension and Risk Factors
Hypertension is categorized into different stages based on blood pressure readings. Understanding these stages is important for assessing risk and guiding treatment strategies. The stages are generally defined by the systolic and diastolic blood pressure readings.
- Prehypertension: Blood pressure readings fall between 120/80 and 139/89 mmHg. This stage signifies a heightened risk for developing hypertension. Factors like a sedentary lifestyle, excessive sodium intake, and obesity often contribute to prehypertension.
- Stage 1 Hypertension: Blood pressure readings range from 140/90 to 159/99 mmHg. This stage represents a significant risk for developing cardiovascular problems. Risk factors include family history, stress, lack of physical activity, and unhealthy dietary habits.
- Stage 2 Hypertension: Blood pressure readings are 160/100 mmHg or higher. This stage indicates a substantially increased risk of severe health complications. Underlying conditions, such as kidney disease or sleep apnea, may be present, alongside the risk factors mentioned in the previous stages.
History of Hypertension Diagnosis Methods
The history of hypertension diagnosis reflects advancements in medical technology and understanding. Initially, diagnosis relied primarily on clinical assessments, including physical examinations and patient histories. The development of sophisticated blood pressure measurement devices, like the sphygmomanometer, revolutionized the process, allowing for more accurate and consistent readings. More recently, ambulatory blood pressure monitoring and 24-hour blood pressure monitoring have further refined diagnostic capabilities.
Diagnostic Approaches Comparison
The table below summarizes various diagnostic approaches, highlighting their strengths and weaknesses.
| Diagnostic Approach | Description | Strengths | Weaknesses |
|---|---|---|---|
| Clinical Evaluation | Physical examination, patient history, and risk factor assessment. | Cost-effective, readily available, and provides initial risk assessment. | Subjective, prone to inaccuracies without advanced training, and may not identify underlying causes. |
| Laboratory Tests | Blood tests (e.g., cholesterol, creatinine, electrolytes) to assess organ function. | Identifies potential underlying conditions (e.g., kidney disease), and provides objective data. | More expensive and time-consuming compared to clinical evaluation. |
| Ambulatory Blood Pressure Monitoring (ABPM) | Measures blood pressure over 24 hours in a patient’s usual environment. | Provides a more accurate representation of blood pressure variability and identifies white coat hypertension. | Can be inconvenient for the patient, requires specific equipment, and may be more expensive. |
| 24-Hour Blood Pressure Monitoring | Measures blood pressure every hour for 24 hours. | More precise in identifying blood pressure fluctuations and abnormalities. | More expensive and can be uncomfortable for patients, particularly when frequent measurements are required. |
Clinical Evaluation Methods
Uncovering hypertension often hinges on a thorough clinical evaluation. This involves meticulous patient history, a detailed physical examination, and precise blood pressure measurements. Understanding these methods is crucial for accurate diagnosis and effective management of this prevalent condition.A comprehensive approach to hypertension diagnosis necessitates careful consideration of a patient’s history, physical examination, and blood pressure measurements. This process allows healthcare professionals to identify potential risk factors, assess the severity of the condition, and tailor treatment plans accordingly.
It’s vital to remember that these methods should be conducted with precision and attention to detail to ensure an accurate diagnosis.
Learning all about hypertension diagnosis is crucial, but proactive health measures like securing health insurance are equally important. Consider why not wait until you’re sick to buy health insurance – it’s often more affordable and easier to manage in the long run. This crucial step can make a huge difference in managing your health, including conditions like hypertension, so don’t delay.
Understanding your options for diagnosis and treatment of hypertension is essential for overall well-being.
Patient History Components
A thorough patient history is fundamental in identifying potential risk factors and contributing elements to hypertension. It includes inquiries about family history of hypertension, personal medical history, current medications, lifestyle habits, and any other relevant information that may influence blood pressure readings. Detailed inquiries about diet, exercise routines, stress levels, and sleep patterns are vital components of the history.
For instance, a history of excessive salt intake or a sedentary lifestyle could be indicative of an increased risk for hypertension.
Physical Examination Significance
The physical examination plays a critical role in assessing for signs associated with hypertension and other underlying conditions. Blood pressure measurement, along with observations of heart rate, auscultation of heart sounds for murmurs or abnormal rhythms, and assessing for edema, are all crucial aspects of the physical examination. The presence of other conditions, like kidney disease or thyroid issues, might be hinted at through physical examination findings.
Blood Pressure Measurement Techniques
Accurate blood pressure measurement is essential for diagnosing hypertension. Proper technique is paramount to ensure reliable results. Several factors can influence blood pressure readings, including the patient’s emotional state, recent physical activity, and the environment where the measurement is taken. The technique used should be consistent and standardized.
Blood Pressure Monitor Types
Various blood pressure monitors are available, each with its own advantages and disadvantages. Sphygmomanometers, utilizing an inflatable cuff and a mercury or aneroid manometer, have been traditional methods for blood pressure measurement. Electronic devices, increasingly prevalent, offer automated measurements, reduced operator variability, and digital display of results. The choice of monitor depends on factors such as the setting where the measurement is performed (e.g., clinic vs.
home), the resources available, and the patient’s specific needs.
Blood Pressure Measurement Procedure
| Step | Description |
|---|---|
| 1 | Prepare the patient: Have the patient rest quietly for 5 minutes in a relaxed posture, and ensure a comfortable environment. |
| 2 | Select appropriate cuff size: The cuff should be appropriate for the patient’s arm size. |
| 3 | Position the cuff: Place the cuff around the upper arm, centered over the brachial artery. |
| 4 | Zero the device: Ensure the device is calibrated and properly zeroed. |
| 5 | Inflate and deflate the cuff: Inflate the cuff to a pressure above the estimated systolic pressure, then slowly deflate the cuff, and listen for Korotkoff sounds or observe the pressure readings. |
| 6 | Record the readings: Document both systolic and diastolic blood pressure readings. |
| 7 | Repeat the measurements: Take multiple readings to account for variability and obtain an average reading. |
Common Measurement Errors
Several factors can lead to inaccurate blood pressure readings. Incorrect cuff size, improper cuff placement, inadequate rest periods, or patient anxiety can all influence the accuracy of the measurements. Failure to follow a standardized procedure can result in misdiagnosis. Understanding these potential errors is essential for interpreting the results correctly.
Lifestyle Factors in Patient History, All about hypertension diagnosis
Lifestyle factors, such as diet and exercise habits, significantly influence blood pressure. A diet high in sodium and saturated fats, combined with a sedentary lifestyle, can contribute to hypertension. Conversely, a balanced diet rich in fruits, vegetables, and whole grains, combined with regular physical activity, can lower blood pressure and reduce the risk of developing hypertension. A comprehensive patient history must include inquiries about lifestyle habits to gain a complete understanding of the individual’s risk factors.
Laboratory Tests for Hypertension Diagnosis

Beyond clinical evaluations, laboratory tests play a crucial role in diagnosing and managing hypertension. These tests help identify underlying causes, assess organ damage, and monitor treatment effectiveness. A thorough understanding of the tests, their purpose, and interpretation is vital for accurate diagnosis and personalized care.Laboratory tests provide valuable supplementary information to clinical assessments. They can detect subtle abnormalities not readily apparent through physical examination.
This information is especially important for evaluating potential complications and tailoring treatment plans. For instance, kidney function tests can reveal early signs of damage that may be asymptomatic.
Key Laboratory Tests
A comprehensive approach to hypertension diagnosis often involves several blood and urine tests. These tests are essential for identifying potential contributing factors and assessing the overall health status of the patient.
Blood Tests
Blood tests provide crucial information about various aspects of the patient’s health, including overall blood composition, electrolyte balance, and kidney function.
Understanding hypertension diagnosis involves a lot more than just high blood pressure readings. It’s crucial to look at the whole picture, including lifestyle factors. Meanwhile, noticeable signs that your cold is getting better, like a lessening cough or a clearer head, can be a good sign of recovery. However, hypertension often requires ongoing monitoring and lifestyle adjustments to manage blood pressure effectively.
A good understanding of the various factors involved, like diet and exercise, is crucial for effective long-term management. Learning about these factors will help you understand hypertension better. signs your cold is getting better can be a helpful reference point for similar types of recovery. Ultimately, a complete understanding of hypertension diagnosis is key to managing this condition.
- Complete Blood Count (CBC): This test evaluates the cellular components of the blood, including red blood cells, white blood cells, and platelets. A CBC is valuable in assessing potential underlying conditions that might contribute to or be influenced by hypertension. For example, certain blood disorders or infections can impact blood pressure regulation.
- Electrolytes (Sodium, Potassium, Calcium, Magnesium): Electrolyte imbalances can affect blood pressure regulation. Sodium is particularly relevant as excessive sodium intake is a known risk factor. Variations in these levels can indicate underlying conditions or complications of hypertension.
- Kidney Function Tests (Creatinine, Blood Urea Nitrogen): These tests assess the efficiency of kidney function. Impaired kidney function can contribute to or worsen hypertension, or be a consequence of it. Elevated creatinine or blood urea nitrogen levels may signal kidney damage, a critical aspect to evaluate in hypertension management.
Urine Tests
Urine tests offer valuable insights into kidney function and other aspects of the patient’s health.
- Urinalysis: A urinalysis assesses the physical and chemical properties of urine, including the presence of protein, blood, glucose, and other substances. Proteinuria, for instance, can indicate kidney damage, a frequent complication of long-standing hypertension.
Summary Table of Expected Results
| Test | Normal Range | Abnormal (Hypertension) | Interpretation |
|---|---|---|---|
| Creatinine (mg/dL) | 0.6-1.2 | >1.2 | Possible kidney damage |
| Blood Urea Nitrogen (mg/dL) | 8-20 | >20 | Possible kidney dysfunction |
| Sodium (mEq/L) | 135-145 | High or Low | May contribute to or worsen hypertension |
| Potassium (mEq/L) | 3.5-5.0 | High or Low | May contribute to or worsen hypertension |
| Urine Protein | Negative | Positive | Possible kidney damage |
Step-by-Step Procedures
Detailed procedures for each test are beyond the scope of this overview. Consult medical laboratory manuals for specific instructions.
Accuracy and Limitations
Laboratory tests provide valuable information but are not definitive diagnostic tools in isolation. The accuracy of these tests depends on proper sample collection, handling, and laboratory procedures. False positives or negatives can occur. For instance, temporary dehydration can affect electrolyte levels.
Importance of Clinical Correlation
Interpreting laboratory results requires careful consideration of the patient’s clinical presentation. A complete evaluation that includes medical history, physical examination, and laboratory findings is essential for accurate diagnosis and management of hypertension. The presence of elevated blood pressure combined with abnormal lab results strengthens the suspicion of hypertension and associated complications.
Diagnostic Criteria and Guidelines
Defining hypertension, the persistent elevation of blood pressure, requires precise diagnostic criteria and guidelines. These standards ensure consistent and accurate diagnoses across various healthcare settings and populations, enabling appropriate management and treatment strategies. Different guidelines exist, tailored to specific age groups and risk factors, reflecting the nuanced approach necessary for effective patient care.
Current Diagnostic Criteria for Hypertension
The current diagnostic criteria for hypertension generally rely on repeated measurements of blood pressure. Multiple readings are crucial because blood pressure can fluctuate throughout the day. A diagnosis is not made based on a single elevated reading. Instead, the average of several readings taken over time is considered.
Diagnostic Guidelines for Different Populations
Different guidelines provide specific recommendations for diagnosing hypertension in various populations, recognizing that factors like age and overall health can impact blood pressure readings and diagnostic thresholds. This approach ensures that the diagnostic process is adapted to the unique characteristics of each group.
- Children: Diagnostic criteria for hypertension in children are distinct from those used in adults. Factors such as growth and development play a significant role. Moreover, the specific criteria are often tailored to the child’s age and percentile ranking for blood pressure, to account for the normal variations in blood pressure across different developmental stages. These variations ensure that diagnoses in children are appropriate for their individual growth patterns.
- Adults: Guidelines for adults usually recommend multiple blood pressure measurements on at least two separate visits. These repeated readings help in confirming the diagnosis and ensure accuracy. Further, lifestyle factors and co-morbidities are considered to aid in a comprehensive assessment. The diagnostic criteria are often linked to the individual’s risk factors, including family history, smoking habits, and dietary patterns.
Factors Influencing the Diagnosis of Hypertension
Several factors influence the diagnosis of hypertension, including the measurement method, the time of day, and the patient’s overall health status. The measurement method should be consistent to ensure accurate readings. The time of day is important because blood pressure tends to fluctuate throughout the day. Furthermore, a patient’s emotional state and physical activity levels can impact the blood pressure reading.
In addition, pre-existing conditions like kidney disease or diabetes can influence blood pressure levels and require careful consideration in the diagnostic process.
Comparison of Diagnostic Criteria Across Organizations
Different organizations, such as the World Health Organization (WHO) and the American Heart Association (AHA), have developed their own guidelines for diagnosing hypertension. While generally aligned, there are subtle differences in the specific thresholds for classifying blood pressure levels.
| Organization | Systolic BP (mmHg) | Diastolic BP (mmHg) |
|---|---|---|
| WHO | 140 or greater | 90 or greater |
| AHA | 130 or greater | 80 or greater |
Importance of Following Established Guidelines
Adhering to established diagnostic guidelines is crucial for ensuring consistency, accuracy, and appropriate management of hypertension. These guidelines help clinicians make informed decisions, leading to more effective patient care. The use of standardized criteria ensures that diagnoses are made in a consistent manner across different healthcare settings, regardless of the clinician or location. This consistency is vital in tracking disease progression, assessing treatment efficacy, and promoting public health initiatives.
Learning about hypertension diagnosis is crucial for overall health, but sometimes, skin concerns can distract us. For example, dealing with pesky bacne can be a real mood killer. Fortunately, there are effective ways to tackle this issue. Checking out how to get rid of bacne here can help you feel more confident. Ultimately, understanding hypertension diagnosis is vital for preventative care and a healthier lifestyle.
Secondary Hypertension Evaluation: All About Hypertension Diagnosis
Unmasking the hidden causes of high blood pressure is crucial for effective management. Secondary hypertension, unlike the more common primary (essential) hypertension, stems from an underlying condition. Identifying this underlying cause is vital, as treatment often focuses on addressing the root issue rather than simply controlling blood pressure. This targeted approach can lead to better long-term outcomes and potentially resolve the hypertension entirely.
Significance of Identifying Secondary Hypertension
Pinpointing secondary hypertension is important for several reasons. Firstly, treating the underlying cause can often lead to a complete resolution of high blood pressure, avoiding the need for lifelong medication. Secondly, certain secondary causes, like renal artery stenosis or Cushing’s syndrome, require specific interventions that address the underlying condition. Finally, prompt diagnosis can prevent potential complications associated with the primary condition, such as kidney damage or stroke.
Early detection can significantly improve patient outcomes and quality of life.
Causes of Secondary Hypertension
Secondary hypertension arises from a wide array of medical conditions. These conditions disrupt the delicate balance of the body’s regulatory mechanisms, leading to elevated blood pressure. Examples include kidney diseases, endocrine disorders, and vascular abnormalities.
Evaluation Methods for Secondary Hypertension
Evaluating secondary hypertension involves a combination of clinical assessments and laboratory tests. A thorough history, including lifestyle factors, family history, and current medications, is essential. Physical examination, focusing on signs of possible underlying conditions, complements the history.
Diagnostic Tests for Secondary Hypertension
A comprehensive evaluation often includes specific diagnostic tests, such as imaging studies and hormone tests. Imaging techniques, such as renal ultrasound or CT angiography, can reveal structural abnormalities in the kidneys or blood vessels. Hormone tests, like aldosterone and renin levels, can detect endocrine imbalances.
Importance of Differentiating Primary from Secondary Hypertension
Differentiating primary from secondary hypertension is critical for appropriate treatment. Primary hypertension, often referred to as essential hypertension, has no identifiable cause. In contrast, secondary hypertension is a consequence of a specific medical condition, necessitating a different approach to management. Failure to identify the secondary cause can result in ineffective treatment of the high blood pressure and potentially lead to complications from the underlying condition.
Comprehensive History in Identifying Secondary Causes
A thorough medical history is fundamental in identifying potential secondary causes. A detailed inquiry about symptoms, lifestyle, medications, and family history can provide crucial clues. For example, a history of persistent headaches, unexplained weight gain, or polyuria can suggest underlying endocrine disorders. A family history of kidney disease can raise suspicion for genetic or inherited conditions.
Table: Common Causes of Secondary Hypertension and Associated Diagnostic Tests
| Cause | Diagnostic Tests |
|---|---|
| Renal Artery Stenosis | Renal ultrasound, CT angiography, Doppler ultrasound |
| Primary Aldosteronism | Plasma aldosterone/renin ratio, CT scan of adrenal glands |
| Cushing’s Syndrome | 24-hour urinary free cortisol, dexamethasone suppression test |
| Pheochromocytoma | Plasma and urine catecholamine measurements |
| Obstructive Sleep Apnea | Overnight polysomnography |
Special Considerations in Hypertension Diagnosis
Hypertension, or high blood pressure, requires careful consideration of various factors beyond standard diagnostic procedures. Different populations, settings, and individual characteristics can significantly impact the accuracy and effectiveness of hypertension diagnosis. Understanding these nuances is crucial for providing appropriate care and preventing potential complications.
Diagnosis in Specific Populations
Different groups, such as pregnant women and children, present unique challenges in hypertension diagnosis. These challenges often stem from the variations in normal blood pressure ranges and the potential for underlying conditions. Accurate diagnosis necessitates a nuanced approach that considers developmental stages and potential comorbidities.
- Pregnant Women: Pre-eclampsia and gestational hypertension are conditions that can mimic or coexist with chronic hypertension. Recognizing these conditions requires careful monitoring of blood pressure throughout pregnancy, along with evaluation of other symptoms. Blood pressure readings must be interpreted in the context of the gestational stage, with careful attention paid to both systolic and diastolic values. For example, a blood pressure reading that might be considered normal in a non-pregnant individual could indicate a serious condition in a pregnant woman.
- Children: Normal blood pressure ranges vary significantly by age and sex in children. Diagnosis in this population relies heavily on repeated measurements, using appropriate-sized cuffs, and considering growth parameters. Factors such as obesity, kidney disease, and genetic predisposition also play a crucial role in hypertension development in children. For example, a child with a family history of hypertension might require more frequent monitoring compared to a child with no such history.
It is essential to consult pediatric specialists for appropriate diagnostic strategies and treatment plans.
Role of Patient Factors
Patient characteristics like ethnicity, age, and lifestyle choices can influence blood pressure readings and the overall risk of developing hypertension.
- Ethnicity: Certain ethnic groups exhibit a higher prevalence of hypertension. For instance, African Americans are known to have a higher incidence of hypertension compared to other ethnic groups. Understanding these disparities is crucial for targeted preventative measures and early interventions. This recognition necessitates adjustments in screening strategies and blood pressure monitoring frequencies.
- Age: Blood pressure typically increases with age. Therefore, interpreting blood pressure readings in older adults requires consideration of age-related changes in vascular function. A higher blood pressure reading in an elderly patient might be a normal physiological variation rather than an indicator of a severe condition. For example, a 70-year-old individual might exhibit higher blood pressure compared to a 20-year-old, which does not necessarily imply hypertension.
Challenges in Specific Settings
Diagnosing hypertension in remote areas can present considerable logistical and resource limitations. These limitations may affect the frequency of blood pressure monitoring, the availability of specialized personnel, and access to diagnostic tests.
- Remote Areas: Limited access to healthcare facilities, healthcare professionals, and diagnostic equipment pose challenges in remote areas. Implementing mobile health clinics and telemedicine initiatives can play a crucial role in addressing these challenges. For example, a remote community lacking access to a hospital may rely on mobile clinics equipped with blood pressure monitors for early detection of hypertension.
Culturally Sensitive Approaches
Cultural factors significantly influence patient behaviour and adherence to treatment. Therefore, cultural sensitivity is essential in hypertension diagnosis and management. Consideration of cultural beliefs, practices, and preferences will contribute to improved patient outcomes.
- Cultural Sensitivity: Understanding cultural norms and beliefs related to health, illness, and treatment is critical. Tailoring communication styles and treatment strategies to individual cultural needs can enhance patient engagement and improve adherence to treatment plans. For instance, a patient from a culture that emphasizes family support might benefit from involving family members in the hypertension management plan.
Table of Specific Considerations
| Patient Population | Specific Considerations |
|---|---|
| Pregnant Women | Gestational hypertension, pre-eclampsia, age-specific norms |
| Children | Age- and sex-specific norms, growth parameters, underlying conditions |
| Ethnic Minorities | Higher prevalence in some groups, targeted screening |
| Elderly | Age-related physiological changes, medication interactions |
| Remote Areas | Limited access to healthcare, telemedicine initiatives |
Continuous Monitoring and Follow-up
Hypertension management necessitates ongoing monitoring and follow-up to ensure effective control and prevent complications. This involves regular blood pressure checks, lifestyle modifications, and medication adjustments as needed.
- Continuous Monitoring: Regular follow-up appointments are crucial for monitoring blood pressure trends and adjusting treatment plans. This continuous monitoring is essential for maintaining optimal blood pressure levels and preventing potential complications.
Last Word
In conclusion, navigating the world of hypertension diagnosis requires a multifaceted approach, combining clinical expertise with laboratory precision. By understanding the various stages, diagnostic methods, and guidelines, you can actively participate in your own health management. This guide provides a comprehensive overview of the process, from initial assessments to secondary hypertension evaluations, emphasizing the importance of continuous monitoring and follow-up.
Remember, early detection and proper management are key to effectively controlling hypertension and mitigating associated risks.