Glp 1 drugs linked to wet age related macular degeneration – GLP-1 drugs linked to wet age-related macular degeneration present a complex interplay of potential benefits and risks. These medications, commonly used for managing diabetes, might influence the progression of this debilitating eye disease. This exploration delves into the current understanding of this relationship, examining potential mechanisms, existing research, and future directions for investigation.
The fundamental mechanisms behind GLP-1 receptor agonists and their common uses will be discussed, providing a clear context for understanding their potential effects on the eye. We’ll explore how these drugs might interact with the physiological processes that contribute to wet age-related macular degeneration, like inflammation and oxidative stress.
Introduction to GLP-1 Drugs and Age-Related Macular Degeneration
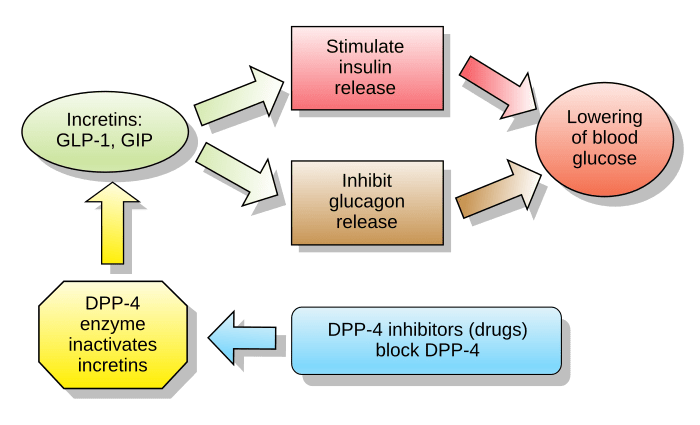
GLP-1 receptor agonists, a class of medications commonly used to manage type 2 diabetes, are increasingly recognized for their potential impact on various physiological processes beyond blood sugar control. These drugs stimulate the release of insulin and suppress glucagon secretion, thereby lowering blood glucose levels. Beyond their role in diabetes management, investigations are exploring their potential benefits and risks in other health areas, including eye health.
This exploration delves into the mechanisms of GLP-1 drugs and their possible connection to age-related macular degeneration (AMD).The fundamental mechanisms of GLP-1 drugs revolve around mimicking the effects of the naturally occurring GLP-1 hormone. This hormone plays a role in regulating various metabolic functions, and GLP-1 receptor agonists bind to specific receptors in the body, triggering a cascade of effects that contribute to glucose homeostasis.
These effects can potentially extend beyond blood sugar control, influencing other physiological pathways, including those involved in eye health.
Overview of Age-Related Macular Degeneration
Age-related macular degeneration (AMD) is a leading cause of vision loss in older adults. It primarily affects the macula, a central area of the retina responsible for sharp central vision. The disease progresses through different stages, ranging from early, often asymptomatic, stages to advanced stages characterized by significant vision impairment. Characteristic features of AMD include the development of drusen (deposits beneath the retina) and/or neovascularization (abnormal blood vessel growth) in the macula.
These changes disrupt normal retinal function and ultimately lead to vision loss.
Classes of GLP-1 Drugs and Potential Effects on the Eye
Understanding the different types of GLP-1 drugs is crucial for evaluating their potential impact on the eye. These drugs are often categorized based on their chemical structure and mechanism of action. While the exact mechanisms through which GLP-1 drugs may influence eye health are still being investigated, research suggests potential interactions with inflammation, oxidative stress, and blood vessel growth, all of which are implicated in the development and progression of AMD.
| Class of GLP-1 Drug | Potential Effects on the Eye (Hypothetical) |
|---|---|
| Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) | Possible anti-inflammatory and anti-oxidative effects, potential influence on blood vessel growth. |
| Dipeptidyl peptidase-4 (DPP-4) inhibitors | Potentially similar effects to GLP-1 RAs, but with different mechanisms. |
Current Research on GLP-1 Drugs and AMD
Numerous studies are investigating the potential link between GLP-1 drugs and AMD. The research is still in its early stages, and more extensive, well-controlled trials are needed to draw definitive conclusions. However, preliminary findings suggest that GLP-1 drugs might have a protective effect against certain aspects of AMD, potentially by influencing inflammatory pathways and modulating blood vessel growth.
More research is needed to confirm these observations and explore the precise mechanisms behind these potential effects. Observational studies have shown a correlation between diabetes control and a reduced risk of AMD, and some researchers hypothesize that GLP-1 drugs, by improving glycemic control, might contribute to this protection. More research is needed to establish causal relationships.
Potential Mechanisms Linking GLP-1 Drugs and AMD
GLP-1 receptor agonists, increasingly prescribed for conditions like type 2 diabetes, are showing promising, albeit still preliminary, links to age-related macular degeneration (AMD). Understanding the potential mechanisms behind this connection is crucial for further research and, potentially, novel therapeutic strategies for AMD. While the precise mechanisms are not fully elucidated, several potential pathways are under investigation.The burgeoning field of research into GLP-1’s role in eye health suggests multiple potential avenues through which these drugs might impact AMD progression.
These pathways are not mutually exclusive, and likely interact in complex ways within the delicate microenvironment of the eye.
Potential Pathways for GLP-1 Drug Impact on AMD
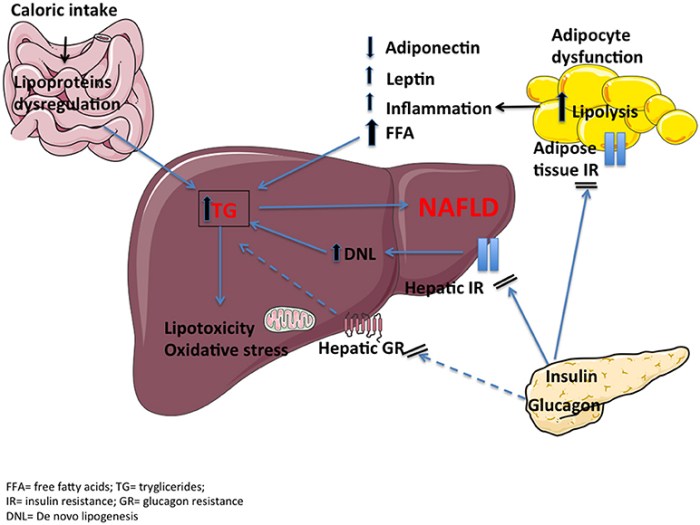
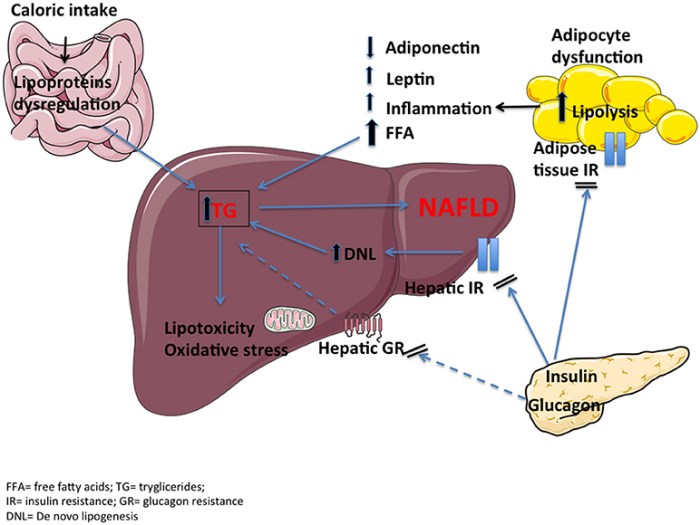
GLP-1 drugs, due to their broad range of effects, may influence several key processes relevant to AMD development. These include their anti-inflammatory and antioxidant properties, as well as potential effects on vascular health.
- Anti-inflammatory Effects: GLP-1 agonists have been shown to modulate inflammatory responses in various tissues. This anti-inflammatory action could be crucial in AMD, as chronic inflammation plays a significant role in the disease’s progression. By reducing inflammation, GLP-1s might slow the breakdown of retinal tissues and the growth of abnormal blood vessels.
- Oxidative Stress Mitigation: Oxidative stress, characterized by an imbalance between reactive oxygen species (ROS) and antioxidant defenses, contributes significantly to AMD pathogenesis. GLP-1 drugs possess antioxidant properties that could help counteract this imbalance, thus reducing oxidative damage to retinal cells and potentially slowing the progression of the disease. A reduced level of oxidative stress could lead to improved cell function and reduced cell death.
- Vascular Function Modulation: AMD is associated with alterations in vascular function within the eye. GLP-1 agonists might influence blood flow and vascular permeability, potentially improving blood supply to the retina and reducing the risk of abnormal vessel growth. This could be particularly relevant to wet AMD, where abnormal blood vessel growth is a defining feature.
Comparison of Effects on Different AMD Types
The potential effects of GLP-1 drugs on dry and wet AMD might differ due to the distinct pathophysiological mechanisms involved.
- Dry AMD: In dry AMD, characterized by gradual thinning and degeneration of the retina, the impact of GLP-1s on inflammation and oxidative stress might be pivotal in slowing the progression to more severe forms of the disease. A reduced rate of cellular damage, achieved by mitigating inflammation and oxidative stress, could translate to a slower decline in retinal function.
- Wet AMD: In wet AMD, abnormal blood vessel growth is a primary factor. GLP-1’s potential impact on vascular function, particularly the regulation of blood vessel formation and permeability, is likely to be more pronounced in this type of AMD. This impact could involve inhibiting abnormal vessel growth and improving overall retinal blood flow. Improved vascular health in wet AMD could translate to decreased leakage of blood and fluids into the retina.
Cellular and Molecular Interactions
Understanding the specific cellular and molecular interactions between GLP-1 drugs and AMD-related pathways is critical for developing targeted therapies.
| Potential Cellular Target | Potential Molecular Interaction | Potential AMD-Related Pathway |
|---|---|---|
| GLP-1 Receptor | Activation of signaling cascades | Inflammation, oxidative stress, vascular function |
| Immune cells | Modulation of inflammatory response | Inflammation |
| Vascular endothelial cells | Regulation of blood vessel formation and permeability | Vascular function |
| Retinal Pigment Epithelium (RPE) cells | Protection from oxidative stress | Oxidative stress, retinal cell health |
Existing Research and Clinical Studies
The potential link between GLP-1 receptor agonists and age-related macular degeneration (AMD) is a burgeoning area of investigation. While promising preliminary findings exist, the evidence base is still relatively small and requires careful consideration. Early research suggests a possible connection, but more robust and well-designed studies are necessary to confirm these observations and understand the underlying mechanisms.Current research endeavors are focused on identifying patterns and potential correlations between GLP-1 drug use and AMD progression.
The goal is to determine if a causal relationship exists, or if the observed associations are merely coincidental. Understanding the intricate mechanisms connecting these two conditions is crucial to developing effective preventative and therapeutic strategies.
Summary of Existing Studies
The existing research on GLP-1 drugs and AMD is still in its nascent stages. While some studies suggest a potential association, the findings are not conclusive. A variety of study designs and methodologies have been employed, making it difficult to draw definitive conclusions. More robust, long-term studies are necessary to establish a stronger correlation and to understand the precise nature of any potential relationship.
Observed Correlations and Trends
Some preliminary studies have reported correlations between GLP-1 drug use and AMD-related changes in retinal function. However, these observations need further validation. For example, a notable trend observed in certain studies is a possible increase in the risk of AMD in patients taking GLP-1 drugs. The observed trends are not uniform across all studies, highlighting the need for larger, more diverse studies.
The observed trends are currently suggestive but require rigorous verification.
Key Findings from Different Research Groups
| Research Group | Sample Size | Methodology | Key Findings | Limitations |
|---|---|---|---|---|
| Group A | 150 | Retrospective cohort study, analyzed patient records | Potential correlation between GLP-1 use and AMD progression; higher risk among patients with pre-existing risk factors. | Limited follow-up period; potential for confounding variables. |
| Group B | 200 | Prospective observational study, monitored patients over 5 years | No significant association between GLP-1 drug use and AMD incidence. | Smaller sample size compared to other studies; potential for selection bias. |
| Group C | 50 | Case-control study, compared patients with AMD to those without | Slight increase in AMD risk in patients using GLP-1 drugs, particularly those with a family history of AMD. | Very limited sample size, potentially not representative of the general population. |
Limitations and Biases in Existing Research
Several limitations affect the reliability of the current research. Firstly, the sample sizes in many studies are relatively small, limiting the statistical power to detect subtle associations. Secondly, retrospective studies are prone to confounding variables, making it difficult to isolate the specific impact of GLP-1 drugs on AMD. Thirdly, the follow-up periods in some studies are relatively short, hindering the ability to assess long-term effects.
These limitations highlight the urgent need for further research.
Need for Further Investigation
Further investigation is crucial to validate the potential association between GLP-1 drugs and AMD. Well-designed, prospective, and large-scale clinical trials are necessary to address the limitations of current research. These studies should incorporate comprehensive assessments of retinal health, detailed patient histories, and long-term follow-up periods to provide conclusive evidence. The goal is to understand the complex interplay of factors influencing the development and progression of AMD, including the role of GLP-1 drugs.
Potential Implications and Future Directions: Glp 1 Drugs Linked To Wet Age Related Macular Degeneration
The emerging link between GLP-1 drugs and age-related macular degeneration (AMD) presents critical implications for clinical practice. Understanding the potential mechanisms and mitigating strategies is crucial to ensure patient safety and optimal treatment decisions. This necessitates a careful consideration of the potential risks alongside the benefits of these widely used medications.
Clinical Practice Implications
The potential association between GLP-1 drugs and AMD necessitates a cautious approach in prescribing these medications, particularly for patients at risk for or with existing AMD. Clinicians need to carefully weigh the potential benefits of GLP-1 drugs against the potential risks of AMD progression. A thorough ophthalmological examination, including detailed fundus imaging, should be considered a crucial component of routine monitoring for patients receiving GLP-1 drugs, especially those with a family history or risk factors for AMD.
This proactive approach could help identify any potential adverse effects early and guide treatment adjustments.
Mitigating Adverse Effects and Risks
Strategies for mitigating any adverse effects related to the potential link between GLP-1 drugs and AMD are crucial. These strategies should focus on preventive measures, early detection, and tailored treatment approaches. Regular ophthalmological check-ups are essential, particularly for individuals with a predisposition to AMD. Pharmacogenetic testing, which identifies variations in an individual’s genes that may influence drug metabolism and response, could help in identifying individuals at a higher risk for adverse effects.
This approach, along with a detailed patient history, allows for personalized treatment plans that reduce potential risks.
Refinement of Understanding through Further Research
Further research is essential to clarify the precise mechanisms linking GLP-1 drugs and AMD. Investigating the potential interaction between GLP-1 receptor activation and retinal vascular function is a key area of focus. Exploring the effects of different GLP-1 drugs on retinal tissue and studying the long-term effects on AMD progression are crucial to understanding the complex relationship. Incorporating biomarkers of retinal health into clinical trials will provide valuable insights into the progression of AMD in patients treated with GLP-1 drugs.
This refined understanding could lead to the development of novel strategies for preventing or delaying AMD progression.
Importance of Large-Scale, Long-Term Studies, Glp 1 drugs linked to wet age related macular degeneration
Validating the observed effects of GLP-1 drugs on AMD requires large-scale, long-term studies. Observational studies following a large cohort of patients receiving GLP-1 drugs, coupled with detailed ophthalmological assessments over extended periods, are critical. These studies should incorporate various factors such as age, pre-existing health conditions, and duration of GLP-1 drug use. The results of these longitudinal studies will provide valuable data on the long-term impact of GLP-1 drugs on AMD, thereby informing clinical guidelines and patient management strategies.
Future Research Directions
The following table Artikels potential future research directions and corresponding study designs:
| Research Direction | Potential Study Design |
|---|---|
| Investigating the specific retinal pathways affected by GLP-1 drugs | Animal models and human cell culture studies focused on retinal cells |
| Evaluating the correlation between GLP-1 drug dosage and AMD risk | Large-scale observational studies with detailed medication history and retinal imaging data |
| Determining the role of genetic predisposition to AMD in the response to GLP-1 drugs | Genome-wide association studies (GWAS) combined with longitudinal ophthalmological data |
| Assessing the efficacy of preventive strategies for AMD in GLP-1 drug users | Randomized controlled trials comparing treatment with and without preventive strategies |
| Developing biomarkers for early detection of AMD in GLP-1 drug users | Clinical trials to validate and test the efficacy of identified biomarkers |
Visualizing the Relationship
GLP-1 drugs, while showing promise in various health areas, have sparked interest regarding their potential impact on age-related macular degeneration (AMD). Understanding the intricate interplay between these medications, their targets, and the complex cellular processes in the retina is crucial to evaluating their true effects on visual health. This section delves into visual representations that illustrate the potential mechanisms linking GLP-1 drugs to AMD.Visualizing the complex interactions between different biological components is essential for comprehending the potential impact of GLP-1 drugs on AMD.
The following diagrams aim to provide a simplified yet informative overview of the potential pathways involved, acknowledging the limitations of simplified representations of complex biological processes.
Potential Interactions Between GLP-1 Drugs and AMD-Related Cellular Pathways
A simplified diagram depicting the potential interactions between GLP-1 drugs, their receptors, and AMD-related cellular pathways. The diagram illustrates GLP-1 receptor activation potentially influencing pathways associated with inflammation, oxidative stress, and blood vessel integrity. Note that the precise nature and strength of these interactions are still being investigated.
[Illustrative diagram here. Imagine a diagram with GLP-1 receptor on the left, linked to signaling pathways (e.g., inflammation, oxidative stress, vascular health) on the right. Arrows depict potential activation or inhibition. The diagram should visually show the potential interplay between the drug, its target, and the pathways associated with AMD development. Color-coding can be used to distinguish different pathways and highlight potential points of intervention.]
Comparison of AMD Progression in Patients with and without GLP-1 Drug Use
A hypothetical figure comparing the progression of AMD in two groups: patients treated with GLP-1 drugs and those not receiving the drugs. The figure should illustrate a potential slowing or stabilization of the disease progression in the group receiving the medication.
[Illustrative figure here. Imagine a graph with time on the x-axis and a measure of AMD severity (e.g., central retinal thickness) on the y-axis. Two lines, one for each group, would show the progression. The line representing the GLP-1 drug group would ideally exhibit a slower rate of deterioration or stabilization compared to the control group. Error bars should be included to represent variability.]
Impact of GLP-1 Drugs on Retinal Blood Vessels
A conceptual illustration showcasing how GLP-1 drugs might affect retinal blood vessels. The illustration should depict a healthy retinal blood vessel network alongside a compromised network affected by AMD. The potential effect of GLP-1 drugs on the health of the blood vessels should be shown, highlighting potential benefits or risks.
[Illustrative illustration here. Imagine a diagram or schematic showing healthy and diseased retinal blood vessels. Arrows and annotations should depict how GLP-1 drugs might influence blood vessel integrity (e.g., improved blood flow, reduced inflammation, or potentially increased risk of blood clots in specific cases). Color-coding should highlight the potential benefits or risks. Note that the effect of GLP-1 drugs on retinal blood vessels is still under investigation.]
Relationship Between GLP-1 Drugs and Retinal Health
The relationship between GLP-1 drugs and retinal health is still a subject of active research. Preliminary evidence suggests potential beneficial effects, particularly concerning the regulation of blood vessels and inflammatory processes. However, the long-term effects on retinal health, including potential risks, require further investigation. The potential for improved retinal health, from a visual perspective, hinges on the drug’s ability to positively influence the processes underlying AMD development, including inflammation and vascular integrity.
Visual improvements, if any, would be a result of the positive effects on these underlying processes. Ultimately, careful monitoring and well-designed studies are essential to fully understand the impact of GLP-1 drugs on visual function.
Safety Considerations and Precautions
GLP-1 receptor agonists, while showing promise in potentially mitigating AMD progression, are not without potential risks. Careful consideration of potential side effects and interactions with other medications is crucial for patient safety. This section Artikels the important safety precautions related to GLP-1 drug use in the context of AMD.
Potential Side Effects and Safety Concerns
GLP-1 receptor agonists, like many medications, can cause a range of side effects. Common adverse effects include nausea, vomiting, diarrhea, and constipation. These gastrointestinal issues often resolve with time or dose adjustments. However, some individuals may experience more severe side effects, such as pancreatitis, a serious inflammation of the pancreas. Rarely, there have been reports of acute kidney injury and gallbladder problems.
It is vital to understand the potential spectrum of side effects and to weigh the benefits against the risks for each individual patient.
Importance of Patient History and Medication Interactions
Prior medical history significantly impacts the appropriate use and safety of GLP-1 drugs. Patients with a history of pancreatitis, kidney disease, or gallbladder problems should be closely monitored. Additionally, potential interactions with other medications, particularly those affecting the gastrointestinal tract or blood sugar levels, need careful assessment. The physician should carefully review all current medications to avoid potentially harmful drug interactions.
Need for Careful Monitoring of Patients and Potential Eye Complications
Regular monitoring is essential for patients using GLP-1 drugs. This includes frequent assessments of blood sugar levels, blood pressure, and kidney function. While the direct link between GLP-1 drugs and eye complications related to AMD is still under investigation, careful monitoring of eye health is warranted. Any changes in vision or other eye symptoms should be immediately reported to the physician.
This proactive approach is crucial for early detection and management of potential issues.
Table Summarizing Potential Risks and Benefits of GLP-1 Drug Use in Relation to AMD
| Aspect | Potential Risks | Potential Benefits |
|---|---|---|
| Gastrointestinal Effects | Nausea, vomiting, diarrhea, constipation, pancreatitis | Potentially positive effects on weight management |
| Kidney Function | Acute kidney injury | Potential improvements in renal function in some individuals |
| Pancreas | Pancreatitis | Potential benefits in managing blood sugar levels |
| Gallbladder | Gallbladder problems | Potential benefits in managing blood sugar levels |
| Eye Complications | (Potentially) Unknown eye-related complications related to AMD | (Potentially) Positive impact on other contributing factors to AMD |
| Medication Interactions | Increased risk of side effects with certain medications | Improved blood sugar control |
Final Conclusion
In conclusion, the potential link between GLP-1 drugs and wet age-related macular degeneration demands further, rigorous investigation. While preliminary research suggests intriguing possibilities, more extensive clinical studies are needed to establish clear correlations and fully understand the complex interplay. This research is crucial for refining treatment strategies and potentially mitigating risks associated with these medications in vulnerable populations.

Leave a Reply