Symptoms of rheumatoid arthritis flares sets the stage for this enthralling narrative, offering readers a glimpse into the complexities of this chronic condition. We’ll explore the various symptoms, their progression, and triggers, shedding light on how flares impact daily life. Understanding these nuances is crucial for effective management and improved quality of life.
This comprehensive guide will delve into the specifics of rheumatoid arthritis flares, including their defining characteristics, common symptoms, and the factors that can influence their onset and severity. We’ll also examine how flares differ from the baseline disease activity and how to distinguish them from other conditions.
Rheumatoid Arthritis Flares: Understanding the Ups and Downs: Symptoms Of Rheumatoid Arthritis Flares
Rheumatoid arthritis (RA) is a chronic autoimmune disease characterized by inflammation of the joints. While the underlying disease process is constant, periods of increased inflammation, known as flares, can significantly impact a person’s quality of life. Understanding the triggers and characteristics of these flares is crucial for effective management and symptom control.Flare-ups in rheumatoid arthritis are characterized by a temporary increase in the severity of symptoms, often beyond the baseline level of disease activity.
This increase can manifest in various ways, impacting both physical and emotional well-being. Understanding the mechanisms behind these flare-ups is important for developing tailored strategies to minimize their frequency and intensity.
Defining Rheumatoid Arthritis Flares
A rheumatoid arthritis flare is a temporary exacerbation of symptoms, marked by an increase in inflammation and pain compared to the usual level of disease activity. This increase can affect multiple joints, leading to heightened pain, stiffness, and swelling. The underlying mechanisms driving these episodes are complex and often involve a combination of factors.
Underlying Mechanisms of Flares
Several factors can contribute to the onset of a rheumatoid arthritis flare. These include infections, stress, changes in medication, and environmental triggers. For example, a viral infection can sometimes trigger an increase in inflammatory responses within the body, leading to a flare. Stress hormones can also play a role, increasing the body’s inflammatory response. Even changes in medication, such as a dosage adjustment or a switch to a different medication, can sometimes lead to a temporary flare.
Typical Duration of a Flare
The duration of a rheumatoid arthritis flare can vary significantly. Some flares may last for a few days, while others can persist for several weeks or even months. The length of the flare depends on various factors, including the individual’s overall health, the specific trigger, and the effectiveness of treatment strategies.
Distinguishing Flares from Baseline Disease Activity
Differentiating a flare from the baseline disease activity can be challenging. Baseline activity is the typical level of inflammation and symptoms experienced by an individual with RA. A flare is characterized by a noticeable and significant increase in the severity of symptoms beyond this baseline. For example, a person with a baseline level of moderate morning stiffness might experience severe morning stiffness during a flare.
Key Differences Between a Flare and a Stable Period
| Characteristic | Flare | Stable Period |
|---|---|---|
| Joint pain | Increased intensity and frequency | Moderate or mild, consistent with baseline |
| Joint swelling | Increased size and extent | Minimal or no swelling |
| Stiffness | Marked increase, especially in the morning | Mild to moderate, typically subsides throughout the day |
| Fatigue | Increased severity | Consistent with baseline or reduced |
| Inflammation markers (e.g., ESR, CRP) | Elevated | Within the normal range or slightly elevated |
The table above highlights the key distinctions between a flare and a stable period in rheumatoid arthritis. Monitoring these parameters can assist in recognizing and managing flares effectively.
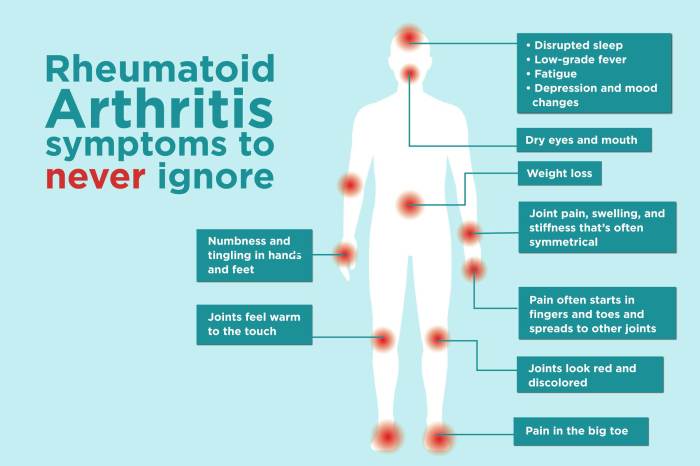
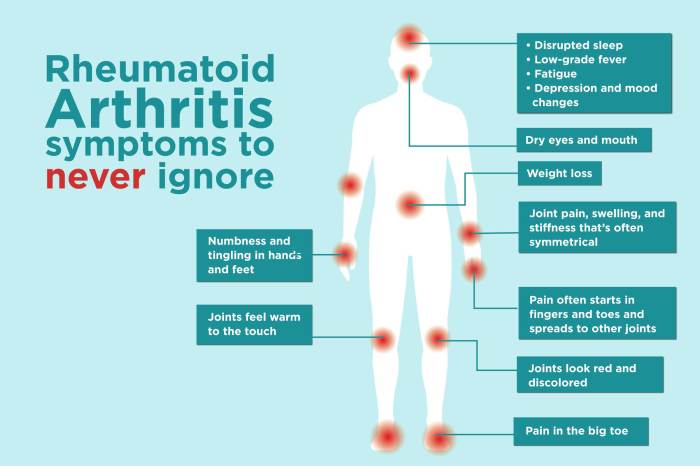
Identifying Flare Symptoms
Rheumatoid arthritis (RA) flares can manifest in a variety of ways, making it crucial to understand the range of symptoms. Recognizing these patterns allows for early intervention and better management of the condition. Identifying flare symptoms is key to getting prompt treatment and avoiding more severe complications.Recognizing the specific symptoms associated with a flare is a critical step in managing rheumatoid arthritis.
While the experience varies greatly from person to person, certain commonalities exist, allowing for a greater understanding of the disease process. The severity and duration of these symptoms can vary significantly, and this variability is a critical aspect of the disease to consider.
Common Flare Symptoms
Understanding the common symptoms associated with RA flares is essential for early recognition and prompt management. These symptoms can range in severity and frequency, and their presentation can vary significantly among individuals.
- Joint pain and stiffness: This is often one of the most prominent symptoms, with affected joints feeling swollen, warm, and tender. Pain can range from mild discomfort to intense throbbing, and stiffness is often most noticeable in the morning or after periods of inactivity.
- Swelling: Swollen joints are a hallmark of RA flares. Swelling can be accompanied by warmth and tenderness, and the degree of swelling can vary depending on the severity of the flare.
- Fatigue: Extreme tiredness, often beyond the typical fatigue associated with daily life, is a frequent symptom during RA flares. This fatigue can significantly impact daily activities and quality of life.
- Morning stiffness: Stiffness in the affected joints, particularly noticeable upon waking, is a common indicator of an RA flare. This stiffness can persist for extended periods.
- Loss of function: As joints become inflamed and painful, the ability to perform daily tasks may be compromised. This can include difficulty with simple movements like getting dressed or walking.
Variability in Symptom Presentation, Symptoms of rheumatoid arthritis flares
The experience of RA flares differs greatly between individuals. Factors like the specific location of inflammation, the duration of the flare, and the overall health status of the patient influence the presentation of symptoms.
- Individual differences: Some individuals might experience primarily joint pain, while others might have more pronounced fatigue or stiffness. The severity and duration of each symptom can vary considerably between individuals.
- Severity of flare: A mild flare might involve only a few joints and mild discomfort, whereas a severe flare could affect numerous joints, causing significant pain and disability.
- Previous flares: Individuals with a history of RA flares might develop a greater sensitivity to symptoms, experiencing them sooner or with greater intensity.
Potential Symptoms During a Flare (Table)
The table below summarizes potential symptoms, their severity, and frequency during an RA flare. This information is for general knowledge and is not a substitute for professional medical advice.
| Symptom | Severity (Mild/Moderate/Severe) | Frequency (Occasional/Frequent/Constant) |
|---|---|---|
| Joint pain | Moderate | Frequent |
| Swelling | Moderate | Frequent |
| Fatigue | Moderate to Severe | Frequent |
| Morning stiffness | Moderate | Frequent |
| Loss of function | Moderate to Severe | Occasional to Frequent |
| Fever | Mild | Occasional |
| Muscle aches | Mild to Moderate | Occasional |
Less Common but Important Symptoms
While the symptoms above are more common, other less frequent symptoms can also indicate an RA flare.
- Fever: A low-grade fever might accompany a flare, although it’s not always present.
- Muscle aches: Generalized muscle pain can sometimes be a symptom of an RA flare.
- Skin rashes: Certain skin rashes can be associated with some RA flares.
- Eye inflammation: Uveitis, an inflammation of the eye, can sometimes be a symptom of RA flares.
Symptom Progression and Duration
Living with rheumatoid arthritis (RA) flares can feel like a rollercoaster. One day you might feel relatively well, and the next, a barrage of symptoms hits you hard. Understanding how these symptoms progress and how long they typically last is crucial for managing the condition and maintaining your quality of life. This knowledge empowers you to better communicate with your healthcare team and develop effective strategies for coping with flare-ups.The progression of symptoms during an RA flare isn’t always linear.
They can build gradually, peaking at a certain point, and then gradually subside. Alternatively, they might strike suddenly, reaching their worst within hours or days. The duration of a flare varies significantly, from a few days to several weeks or even months. Severity also fluctuates; some days might be excruciatingly painful, while others are relatively manageable. This unpredictable nature underscores the importance of monitoring your symptoms diligently and keeping detailed records.
Typical Symptom Progression
The progression of RA flare symptoms is highly variable, but some common patterns emerge. Symptoms often begin with subtle, intermittent discomfort, such as fatigue, joint pain, or stiffness. These initial symptoms can increase in intensity and frequency over a period of days or weeks. The peak of the flare, characterized by maximum pain, inflammation, and functional limitations, typically lasts for several days to a few weeks.
As the flare subsides, the symptoms gradually decrease in intensity and frequency, returning to a baseline state.
Range of Symptom Durations
The duration of RA flares can vary considerably. Short flares might last for a few days, allowing you to manage the symptoms with over-the-counter pain relievers and rest. Prolonged flares, however, can persist for weeks or even months, requiring more intensive medical interventions and potentially impacting your daily life significantly. For example, a patient experiencing a prolonged flare might find it difficult to work or perform household chores.
Symptom Severity Fluctuations
Throughout a flare, symptom severity can fluctuate dramatically. One day you might experience intense pain and stiffness, while the next day, you might feel relatively better. These fluctuations make it challenging to predict the exact course of the flare and can lead to frustration and uncertainty. However, recognizing these patterns can help you adapt your treatment and coping strategies.
Relationship Between Symptom Duration and Disease Activity
The relationship between symptom duration and disease activity in RA flares is complex. While a shorter flare might indicate a lower level of underlying disease activity, a prolonged flare could signify more active inflammation. This is why it’s crucial to discuss your symptoms with your rheumatologist, who can evaluate your individual situation and determine the appropriate course of action.
Example Symptom Progression Table
| Day | Fatigue | Joint Pain (Wrist) | Morning Stiffness | Overall Function |
|---|---|---|---|---|
| 1 | Mild | Mild, intermittent | Moderate | Mostly normal |
| 3 | Moderate | Moderate, frequent | Severe | Slightly reduced |
| 5 | Severe | Severe, constant | Severe | Significantly reduced |
| 7 | Moderate | Moderate, intermittent | Moderate | Improved |
| 10 | Mild | Mild, infrequent | Mild | Normal |
This table illustrates a possible progression of symptoms over time. Note that individual experiences may differ significantly.
Associated Symptoms and Complications
Rheumatoid arthritis flares aren’t just about the painful joint symptoms. A wide range of associated symptoms can significantly impact a person’s overall well-being and the severity of the flare itself. Understanding these accompanying issues is crucial for effective management and improving quality of life.
Rheumatoid arthritis flares can bring on a whole host of symptoms, from aching joints to fatigue. Finding ways to manage these symptoms is key, and that includes looking at your diet. A good protein bar, for example, can be a convenient and nutritious snack. Learning how to choose a protein bar that meets your needs can be a real game-changer, especially during a flare.
Consider factors like ingredients, portion size, and overall nutritional value. For a comprehensive guide on this, check out how to choose a protein bar. Ultimately, understanding these symptoms and managing your diet are crucial for navigating these challenging periods.
Common Associated Symptoms
Beyond the hallmark joint pain, fatigue, fever, and weight loss are frequently reported during flares. These symptoms often accompany the inflammation and immune system activity characteristic of rheumatoid arthritis. These additional symptoms can dramatically increase the overall impact of the flare, making daily tasks more challenging and contributing to a decreased quality of life.
Impact on Flare Severity
The presence of associated symptoms can significantly influence the severity of a rheumatoid arthritis flare. For example, intense fatigue can make even simple activities feel overwhelming, compounding the discomfort of joint pain. Fever can exacerbate inflammation and pain, while weight loss can signal a more severe or prolonged inflammatory response within the body. The combination of multiple associated symptoms often results in a more debilitating experience than joint pain alone.
Potential Complications of Severe or Prolonged Flares
Prolonged or severe flares of rheumatoid arthritis can lead to a range of complications. These complications can arise from the sustained inflammation and immune system activation. Potential complications include damage to organs like the heart, lungs, and kidneys. Additionally, there is an increased risk of cardiovascular issues due to chronic inflammation. It’s crucial to address both the joint symptoms and associated symptoms to mitigate these potential complications.
Rheumatoid arthritis flares can bring a whole host of unpleasant symptoms, from the usual aches and stiffness to something far more unsettling – a feeling of impending doom. This feeling, often described as a sense of dread or anxiety, can be a significant part of the experience for many people with RA. It’s a difficult symptom to shake, often preceding or accompanying other physical symptoms like intense joint pain and fatigue.
Understanding this emotional component alongside the physical symptoms is crucial for managing RA flares effectively. Learning more about this “feeling of impending doom” can be helpful in managing the experience here.
Impact on Daily Activities and Quality of Life
Rheumatoid arthritis flares have a substantial impact on daily activities and quality of life. The pain, fatigue, and other associated symptoms can make simple tasks like bathing, dressing, or even walking feel insurmountable. This can lead to social isolation, reduced productivity, and a general decrease in overall well-being. Managing these flares effectively is essential to maintain a fulfilling and productive life.
Summary of Associated Symptoms and Impact
| Associated Symptom | Potential Impact on Flare Severity | Impact on Daily Life |
|---|---|---|
| Fatigue | Increases the perceived severity of joint pain, makes daily activities more difficult. | Reduces productivity, increases social isolation, affects ability to perform daily tasks. |
| Fever | Exacerbates inflammation and pain, potentially increasing the severity of the flare. | Can lead to discomfort, fever-related symptoms like chills, sweats, and headaches. |
| Weight Loss | May indicate a more severe or prolonged inflammatory response. | Can lead to nutritional deficiencies, further impacting overall well-being. |
| Other Associated Symptoms (e.g., Anemia, Muscle Pain, Sleep Disturbances) | Contribute to overall fatigue and discomfort, compounding the effects of joint pain. | Can affect mood, cognitive function, and the ability to participate in daily activities. |
Trigger Factors for Flares

Rheumatoid arthritis (RA) flares can be unpredictable, making it challenging to manage the condition. Understanding the factors that trigger these episodes can help individuals proactively manage their symptoms and maintain a better quality of life. Knowing what might set off a flare can empower you to make necessary lifestyle adjustments.Understanding the triggers behind rheumatoid arthritis flares is crucial for managing the condition effectively.
This knowledge allows individuals to anticipate potential flare-ups and proactively implement strategies to mitigate their impact.
Environmental Factors
Environmental factors can play a significant role in triggering RA flares. Exposure to certain environmental triggers can initiate or worsen inflammation in the affected joints.
- Cold temperatures can sometimes exacerbate RA symptoms. Prolonged exposure to cold environments can constrict blood vessels, reducing blood flow to the joints, which can increase pain and stiffness. This is often seen in individuals with RA.
- Changes in barometric pressure are another potential environmental factor linked to RA flares. These changes can influence the body’s inflammatory response, potentially leading to increased pain and discomfort in the affected joints. The precise mechanism is not fully understood but is believed to be related to changes in the body’s internal pressure and fluid balance.
- Exposure to certain allergens and pollutants can trigger an inflammatory response, contributing to RA flares. Common allergens like pollen, dust mites, and pet dander can irritate the respiratory system and potentially influence systemic inflammation in those with RA. Pollutants like certain chemicals and industrial fumes may also play a role.
Lifestyle Factors
Certain lifestyle choices can influence the risk of RA flares. Making conscious adjustments can help individuals manage their symptoms effectively.
- Lack of adequate sleep can negatively impact the body’s ability to regulate inflammation. Insufficient sleep can increase stress hormones, which in turn can worsen inflammation and contribute to RA flares. Maintaining a consistent sleep schedule and creating a relaxing bedtime routine can help minimize this risk.
- Poor nutrition can affect the body’s overall health and potentially exacerbate RA symptoms. A diet rich in processed foods, sugary drinks, and unhealthy fats can contribute to inflammation. Conversely, a balanced diet rich in fruits, vegetables, and lean proteins can support the body’s natural anti-inflammatory processes and may help minimize flare-ups.
- Physical stress can also play a role in triggering RA flares. Excessive physical exertion, especially when not adequately rested, can increase the body’s inflammatory response, leading to pain and swelling in the affected joints. It is important to listen to the body and adjust activity levels as needed to prevent overexertion.
Infections
Infections can sometimes trigger or worsen RA flares. The body’s response to infection can activate the immune system, potentially leading to increased inflammation in the joints.
- Viral or bacterial infections are potential triggers for RA flares. The body’s immune response to these infections can inadvertently affect the joints, exacerbating existing RA symptoms or triggering new ones. A common example is the flu, which can be a significant trigger in some individuals.
- Dental infections, in particular, have been linked to RA flares. The inflammatory response to these infections can be systemic, potentially affecting other parts of the body, including the joints.
Stress and Psychological Factors
Stress and other psychological factors can significantly influence RA flares. The body’s response to stress can activate the inflammatory response, potentially leading to increased pain and discomfort in the affected joints.
- Stressful life events, such as job loss, relationship problems, or financial difficulties, can contribute to RA flares. The physiological response to stress can trigger an increase in inflammation, which may worsen existing RA symptoms.
- Chronic stress, a prolonged period of emotional strain, can also play a role in RA flare-ups. This type of stress can negatively impact the body’s ability to regulate inflammation and contribute to more frequent and severe RA symptoms. For example, a period of high-pressure work demands could exacerbate symptoms.
Monitoring and Managing Flares
Navigating rheumatoid arthritis flares can feel like a rollercoaster. Understanding how to monitor your symptoms and implement effective management strategies is crucial for maintaining a good quality of life. This involves a proactive approach, not just reacting to flare-ups, but anticipating them and minimizing their impact.
Monitoring Symptom Severity and Frequency
Regularly tracking symptoms is essential for recognizing patterns and communicating effectively with your rheumatologist. This involves meticulous documentation of pain levels, stiffness duration, swelling extent, and fatigue intensity. Using a symptom diary, a dedicated app, or a notebook can help you systematically record these observations. Note the time of onset, duration, and any associated factors like weather changes or stress levels.
This data allows you to identify triggers and predict potential flare-ups.
Strategies for Managing Flare Symptoms
Various strategies can help alleviate the discomfort and challenges of a flare. Rest is crucial, but it’s important to avoid prolonged inactivity. Gentle movement and light exercise can help maintain joint mobility and reduce stiffness. Heat therapy, such as warm compresses or baths, can soothe aching joints. Cold therapy, like ice packs, can help reduce inflammation.
Mindfulness and relaxation techniques, such as deep breathing exercises or meditation, can help manage stress, which is often a contributing factor to flares.
Rheumatoid arthritis flares can be tricky, bringing on a whole host of symptoms like fatigue and joint pain. Sometimes, these flare-ups might be linked to surprising things, like certain foods. For instance, if you’re looking to identify potential triggers, checking out a migraine trigger food list could be insightful, as some foods that cause migraines might also affect your rheumatoid arthritis.
Ultimately, understanding your body’s unique reactions is key to managing these flare-ups effectively.
Self-Care Techniques for Alleviating Symptoms
Implementing self-care techniques is an integral part of managing flare symptoms. Prioritizing sleep is vital, as fatigue often exacerbates RA symptoms. A balanced diet rich in anti-inflammatory foods like fruits, vegetables, and omega-3 fatty acids can help reduce inflammation. Staying hydrated by drinking plenty of water supports overall well-being. Avoiding triggers, like specific foods or environmental factors, can also help prevent or lessen the severity of a flare.
A regular exercise routine, even if modified during a flare, helps maintain overall health and well-being.
- Prioritize sleep: Aim for 7-9 hours of quality sleep each night. Adequate rest helps the body repair and combat inflammation.
- Maintain a balanced diet: Focus on anti-inflammatory foods like fruits, vegetables, and omega-3 rich foods. Limit processed foods, sugary drinks, and excessive alcohol.
- Stay hydrated: Drink plenty of water throughout the day to support overall health and potentially reduce inflammation.
- Manage stress: Incorporate stress-reducing techniques like meditation, yoga, or deep breathing exercises into your routine.
- Avoid triggers: Identify and avoid specific foods, environmental factors, or activities that worsen your symptoms.
The Role of Medication in Managing Flares
Medications play a significant role in managing RA flares. Disease-modifying antirheumatic drugs (DMARDs) are crucial for long-term management, reducing inflammation and preventing joint damage. Symptomatic medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroids, can provide rapid relief from pain and inflammation during flares. Your rheumatologist will tailor a medication regimen based on your individual needs and response to treatment.
Lifestyle Modifications for Flare Management
Lifestyle modifications are vital for managing RA flares effectively. Maintaining a consistent sleep schedule, a balanced diet, and stress-reducing activities can significantly impact symptom severity. Regular exercise, even modified during flares, helps maintain joint mobility and overall health. Avoiding smoking and excessive alcohol consumption further contributes to better overall health and symptom management. It is essential to establish a supportive environment, including social connections and emotional support, to help navigate the challenges of living with RA.
Differentiating Flares from Other Conditions
Navigating the world of autoimmune diseases can be tricky, especially when symptoms overlap. Distinguishing rheumatoid arthritis (RA) flares from other inflammatory conditions requires careful consideration of various factors. Accurate diagnosis is paramount to receiving appropriate treatment and managing the condition effectively. Misdiagnosis can lead to delayed interventions and potentially worsen the disease progression.
Identifying Overlapping Symptoms
Numerous conditions can mimic the symptoms of RA flares. These include other forms of arthritis, infections, and even some non-articular inflammatory conditions. Understanding the commonalities and differences is key to precise diagnosis. Symptoms like joint pain, stiffness, and swelling can be present in several inflammatory diseases. This underscores the critical role of a comprehensive medical evaluation.
Comparing RA Flares with Other Potential Diagnoses
| Characteristic | Rheumatoid Arthritis Flare | Osteoarthritis | Psoriatic Arthritis | Lupus |
|---|---|---|---|---|
| Joint Involvement | Symmetrical, often affecting multiple joints | Asymmetrical, typically affecting weight-bearing joints | Asymmetrical, often associated with skin psoriasis | Polyarticular, can affect various joints, with possible skin manifestations |
| Morning Stiffness | Often lasting for at least 30 minutes | May or may not be present, usually less than 30 minutes | May be present, often less than 30 minutes | May be present, duration variable |
| Systemic Symptoms | Possible, including fatigue, fever, and malaise | Generally absent | Possible, including fatigue and fever | Common, including fatigue, fever, and other constitutional symptoms |
| Rheumatoid Factor/Anti-CCP Antibodies | Often positive | Usually negative | May be positive, but not always | May be positive, but not always diagnostic |
This table provides a simplified comparison. Individual experiences can vary, and a thorough examination is essential.
Role of Medical History and Physical Examination
A detailed medical history plays a crucial role in differentiating RA flares. The doctor will inquire about the duration and pattern of symptoms, any prior diagnoses, and any potential triggers. The physical examination is equally important. The doctor will assess the affected joints for tenderness, swelling, and range of motion. They will also evaluate for any systemic symptoms like fever, rash, or fatigue.
A thorough assessment of the patient’s overall health status provides crucial information.
“A comprehensive approach involving detailed medical history, physical examination, and appropriate laboratory tests are crucial for accurate diagnosis and treatment of rheumatoid arthritis flares.”
The doctor will consider all the factors to provide the most suitable course of treatment.
Illustrative Case Studies
Understanding rheumatoid arthritis (RA) flares requires more than just knowing the symptoms. Real-life examples provide crucial insight into the complexities of this chronic autoimmune disease. These cases demonstrate the variability in flare presentations, the impact on daily life, and the diverse management strategies employed. By examining these scenarios, we gain a deeper appreciation for the challenges faced by individuals living with RA.The following case studies illustrate the unpredictable nature of RA flares, highlighting the variety of symptoms, triggers, and management approaches.
Each case underscores the individual experiences and emphasizes the importance of personalized care plans tailored to each patient’s needs.
Case Study 1: The Impact of Stress
This patient, a 45-year-old woman, experienced frequent RA flares linked to high-stress periods. During these times, she reported increased joint pain, stiffness, and fatigue, impacting her ability to work and participate in social activities. Her management strategy included stress-reduction techniques, such as yoga and meditation, alongside medication adjustments with her rheumatologist. This case demonstrates how psychological factors can exacerbate RA symptoms and the importance of incorporating holistic approaches into management.
Case Study 2: The Role of Infection
A 62-year-old man with a history of RA experienced a severe flare following a urinary tract infection. He presented with intense joint pain, fever, and malaise. His treatment involved addressing the infection with antibiotics and adjusting his RA medication regimen. This case illustrates how infections can trigger RA flares, emphasizing the need for prompt medical attention when infections occur.
Case Study 3: The Effect of Environmental Factors
A 30-year-old woman with RA noticed a pattern of flares coinciding with changes in weather, particularly during periods of extreme humidity. Her symptoms included increased joint pain and swelling, along with a sense of overall discomfort. Her rheumatologist advised her on lifestyle modifications, such as staying hydrated and using humidifiers. This case highlights the potential role of environmental factors in triggering RA flares, emphasizing the importance of identifying potential triggers.
Case Study 4: Medication Side Effects
A 58-year-old man with RA experienced a flare after starting a new medication for high blood pressure. The new medication seemed to worsen his RA symptoms, including joint pain, swelling, and stiffness. His rheumatologist adjusted his RA medication regimen and discontinued the blood pressure medication, which resolved the issue. This case emphasizes the importance of monitoring for potential side effects from medications and the possibility of interactions with RA medications.
Summary Table of Case Studies
| Case Study | Patient Profile | Flare Symptoms | Triggers | Management Approaches | Impact on Patient Life |
|---|---|---|---|---|---|
| 1 | 45-year-old woman; high stress | Increased joint pain, stiffness, fatigue | High-stress periods | Stress-reduction techniques, medication adjustments | Limited ability to work and participate socially |
| 2 | 62-year-old man; history of RA | Intense joint pain, fever, malaise | Urinary tract infection | Antibiotics, RA medication adjustments | Severe disruption to daily life |
| 3 | 30-year-old woman; history of RA | Increased joint pain, swelling, discomfort | Extreme humidity | Lifestyle modifications, humidifiers | Discomfort and reduced mobility |
| 4 | 58-year-old man; history of RA | Joint pain, swelling, stiffness | New blood pressure medication | RA medication adjustments, discontinued blood pressure medication | Significant impact on daily activities |
End of Discussion
In conclusion, understanding rheumatoid arthritis flares is essential for effective self-management. By recognizing the diverse symptoms, triggers, and potential complications, individuals can better prepare for and navigate these episodes. This knowledge empowers them to work collaboratively with healthcare professionals to develop personalized strategies for managing flares and maintaining a fulfilling life.

Leave a Reply