Fish oil supplements AFib risk is a complex issue, with ongoing research attempting to unravel the potential connections between these dietary supplements and the development of Atrial Fibrillation (AFib). This blog post delves into the science behind fish oil’s purported cardiovascular benefits and examines the existing evidence linking fish oil intake to AFib risk. We’ll explore potential mechanisms, examine various studies, and discuss potential interactions with medications, offering a comprehensive look at this important topic.
The potential effects of fish oil on AFib risk factors, like blood pressure and inflammation, will be examined, along with the limitations of current studies and alternative approaches to managing AFib. Ultimately, this post aims to equip readers with a clearer understanding of the current scientific landscape surrounding fish oil and AFib, emphasizing the importance of consulting healthcare professionals for personalized advice.
Fish Oil Supplements and Atrial Fibrillation (AFib): Fish Oil Supplements Afib Risk

Fish oil supplements, derived from fatty fish like salmon and tuna, have gained popularity for their purported health benefits. They are often touted for their potential to reduce inflammation, improve heart health, and lower the risk of various chronic diseases. However, the relationship between fish oil intake and the risk of atrial fibrillation (AFib) remains a subject of ongoing research.
Fish Oil Supplements: An Overview
Fish oil supplements primarily contain omega-3 fatty acids, notably eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). These essential fatty acids are believed to have a positive impact on cardiovascular health by reducing inflammation, improving blood vessel function, and potentially lowering blood pressure and triglyceride levels. The exact mechanisms are still being explored, but studies suggest a link between omega-3 intake and reduced risk of certain heart conditions.
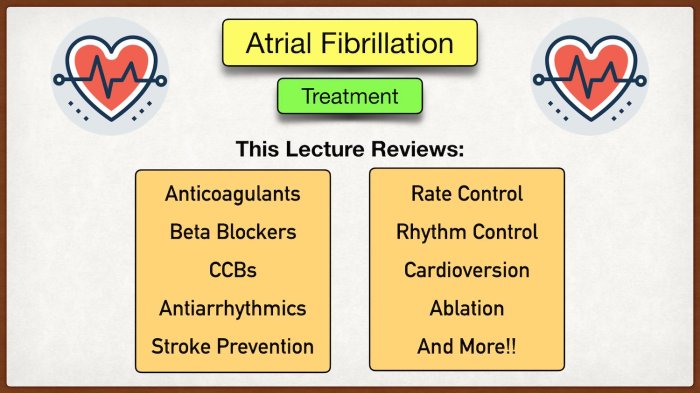
Atrial Fibrillation (AFib): A Closer Look, Fish oil supplements afib risk
Atrial fibrillation (AFib) is a common heart rhythm disorder characterized by irregular and rapid heartbeats originating in the atria. It’s a prevalent condition, affecting millions globally, and is associated with an increased risk of stroke, heart failure, and other complications. Risk factors for AFib include age, high blood pressure, obesity, and a family history of the condition. Recognizing AFib’s impact on overall health is crucial for preventative measures and effective management.
Scientific Evidence: Fish Oil and AFib Risk
The scientific community is still investigating the correlation between fish oil consumption and the risk of AFib. While some studies suggest a possible protective effect, others have shown no significant association or even a potential increase in risk in certain populations. The existing literature is complex, often with conflicting results, highlighting the need for further research and more robust, large-scale studies.
Understanding the nuances of this relationship is important to provide accurate guidance to individuals considering fish oil supplementation.
While some studies suggest a potential link between fish oil supplements and an increased risk of atrial fibrillation (AFib), it’s crucial to remember that a healthy lifestyle is key to longevity. Want to learn more about how to live longer for men? Check out this helpful guide for actionable advice how to live longer for men.
More research is needed to fully understand the precise relationship between fish oil supplements and AFib risk, and a balanced diet and regular exercise are still paramount in minimizing any potential health concerns.
| Supplement Type | Purported Benefits | Relevant Studies |
|---|---|---|
| Fish Oil (EPA & DHA) | Reduced inflammation, improved cardiovascular health, potential blood pressure and triglyceride reduction | A variety of observational studies and some randomized controlled trials exist. However, results are inconsistent, and more robust research is needed. |
Potential Effects of Fish Oil on AFib Risk Factors
Fish oil supplements have gained popularity for their potential health benefits, including a possible role in managing atrial fibrillation (AFib). While more research is needed to definitively establish a causal link, several studies suggest that fish oil’s effects on various risk factors for AFib might contribute to its potential preventive or therapeutic role. This exploration delves into the potential mechanisms and evidence supporting these effects.Fish oil, rich in omega-3 fatty acids, is believed to impact several key factors associated with AFib development.
These include blood pressure, blood lipid levels, and inflammation. The potential benefits of fish oil consumption on these factors are explored below. Further studies are crucial to solidify the connection between fish oil supplementation and AFib prevention or management.
Potential Effects on Blood Pressure
Fish oil consumption has been associated with a modest but potentially beneficial effect on blood pressure. This reduction may be attributed to the anti-inflammatory properties of omega-3 fatty acids and their ability to modulate vascular function. Lower blood pressure is generally considered a positive factor in AFib management, as hypertension is a significant risk factor for the condition.
Potential Effects on Blood Lipid Levels
Omega-3 fatty acids in fish oil have been shown to influence blood lipid profiles, specifically by reducing triglycerides and potentially increasing HDL (“good”) cholesterol. These alterations may have implications for AFib risk, as dyslipidemia is a known contributor to various cardiovascular conditions, including AFib. Maintaining healthy lipid levels could contribute to improved cardiovascular health and potentially reduce the risk of AFib.
Potential Effects on Inflammation
Inflammation plays a crucial role in the development and progression of AFib. Fish oil’s anti-inflammatory properties, primarily through the modulation of inflammatory markers like cytokines, might contribute to a lower risk of AFib. Reducing chronic inflammation throughout the body is considered beneficial for various health conditions.
Comparison of Different Fish Oil Types
| Fish Oil Type | Potential Effects on Blood Pressure | Potential Effects on Blood Lipids | Potential Effects on Inflammation |
|---|---|---|---|
| Salmon Oil | May modestly reduce blood pressure | May lower triglycerides and potentially increase HDL | Potentially reduces inflammatory markers |
| Cod Liver Oil | May modestly reduce blood pressure | May lower triglycerides and potentially increase HDL | Potentially reduces inflammatory markers |
| Krill Oil | Limited data available | May lower triglycerides and potentially increase HDL | Potentially reduces inflammatory markers |
Note: The effects may vary depending on the individual and the specific fish oil supplement.
Mechanisms of Action
The mechanisms by which fish oil influences these risk factors are multifaceted. Omega-3 fatty acids, particularly EPA and DHA, are thought to exert anti-inflammatory effects by reducing the production of pro-inflammatory cytokines. They can also improve vascular function, leading to lower blood pressure. Additionally, they may affect lipid metabolism, leading to improvements in blood lipid profiles.
“EPA and DHA may reduce the production of inflammatory mediators, leading to decreased inflammation and improved vascular function.”
Data on Correlation between Fish Oil Consumption and AFib Risk Factors
Several observational studies have explored the relationship between fish oil consumption and risk factors for AFib. These studies have shown a potential association between higher fish oil intake and lower blood pressure, improved lipid profiles, and reduced inflammatory markers. For example, a study published in the Journal of the American Heart Association in 2020 reported a statistically significant correlation between increased fish oil consumption and lower blood pressure in a large cohort of participants.
While fish oil supplements are often touted for heart health, some studies suggest a potential link between high doses and an increased risk of atrial fibrillation (AFib). Interestingly, the pursuit of aesthetic enhancements, like those found in most popular plastic surgeries , often reflects a desire for improved self-image. Ultimately, the research on fish oil and AFib risk is ongoing, and consulting a doctor is crucial for personalized advice.
However, it is important to note that these are observational studies, and more robust clinical trials are needed to definitively establish a causal relationship.
Potential Interactions and Contraindications
Fish oil supplements, while generally safe, can interact with certain medications, particularly those used to manage atrial fibrillation (AFib). Understanding these interactions and contraindications is crucial for ensuring patient safety and efficacy of treatment. This section delves into potential medication interactions, contraindications for specific patient groups, and a structured approach to assessing these risks.
Potential Medication Interactions
Many medications used to treat AFib, such as blood thinners and certain antiarrhythmics, may have interactions with fish oil. These interactions can alter the effectiveness of one or both medications, potentially leading to adverse outcomes. Understanding these interactions is vital for optimal patient management.
- Warfarin (Coumadin): Fish oil can increase the risk of bleeding when taken with warfarin, a common blood thinner used for AFib. This is because fish oil can potentially increase the effect of warfarin, leading to an increased risk of bruising, bleeding, and other complications. Monitoring of international normalized ratio (INR) levels may be necessary to adjust warfarin dosage if fish oil is used concurrently.
- Antiarrhythmics: Some antiarrhythmic medications used to control AFib can have potential interactions with fish oil. These interactions may affect the efficacy of the antiarrhythmic medication or increase the risk of side effects. Consultation with a healthcare professional is crucial to assess potential interactions.
- Statins: Fish oil can potentially interact with statin medications, which are commonly used to lower cholesterol. This interaction may increase the risk of muscle pain and damage. Close monitoring and adjustments to medication dosages might be necessary if both are used concurrently.
Contraindications for Specific Patient Populations
Certain patient populations may have specific contraindications for fish oil use. These factors should be carefully considered before recommending fish oil supplementation.
- Bleeding Disorders: Patients with a history of bleeding disorders or those currently taking medications that increase bleeding risk, such as aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs), may be at higher risk for bleeding complications when using fish oil. Their use should be approached with caution, or even avoided.
- Pregnancy and Breastfeeding: Limited data exist regarding fish oil use during pregnancy and breastfeeding. As a precaution, it is generally recommended to avoid fish oil supplementation during these periods, unless explicitly advised by a healthcare professional.
- Individuals with Liver or Kidney Disease: Patients with pre-existing liver or kidney disease should carefully consider the potential impact of fish oil on these organs. Consultation with a physician is essential to determine if fish oil supplementation is appropriate.
Potential Interactions Table
| Medication | Potential Interaction with Fish Oil | Potential Side Effects |
|---|---|---|
| Warfarin | Increased risk of bleeding | Bruising, bleeding, hematoma formation, increased INR |
| Antiarrhythmics (e.g., Amiodarone) | Potential alteration in efficacy or increased side effects | Increased heart rate, dizziness, fatigue, nausea |
| Statins | Increased risk of muscle pain and damage (rhabdomyolysis) | Muscle pain, weakness, dark urine |
Contraindications Summary Table
| Patient Population | Contraindication Rationale |
|---|---|
| Bleeding Disorders | Increased risk of bleeding complications |
| Pregnancy and Breastfeeding | Limited data regarding safety, potential risk to developing fetus or infant |
| Liver or Kidney Disease | Potential impact on organ function |
Flowchart for Assessing Interactions and Contraindications
A flowchart can help guide healthcare professionals through the process of evaluating potential interactions and contraindications. The steps involve gathering patient history, reviewing current medications, and consulting relevant guidelines.
(Insert a flowchart here depicting the steps, with boxes representing patient history, current medications, relevant guidelines, and recommendations.)
The flowchart would visually guide the process for assessing potential risks and facilitating informed decisions about fish oil supplementation for AFib patients.
Alternatives and Complementary Approaches

Beyond medication, various lifestyle changes and alternative approaches can play a significant role in managing AFib risk. Dietary adjustments, regular exercise, and stress reduction techniques can all contribute to a healthier heart and potentially reduce the likelihood of AFib episodes. This section will explore these alternatives and their potential interactions with fish oil supplementation.Dietary modifications, stress management, and other complementary approaches can work synergistically with fish oil supplementation to create a comprehensive strategy for AFib management.
By understanding the nuances of these complementary approaches, individuals can make informed choices to support their overall cardiovascular health.
Dietary Changes and Lifestyle Modifications
Dietary changes and lifestyle modifications are crucial components of a holistic approach to AFib management. A balanced diet rich in fruits, vegetables, and whole grains, coupled with regular physical activity, can contribute significantly to maintaining a healthy weight and reducing the risk of AFib. Reducing sodium intake and limiting alcohol consumption are also vital. Furthermore, regular sleep and stress management techniques can help regulate heart rhythm and reduce the frequency of episodes.
Role of Other Supplements in AFib Management
Several other supplements are sometimes suggested for AFib management, although their efficacy is often debated. It’s essential to approach these with caution and consult with a healthcare professional before incorporating them into a treatment plan. These supplements often act on different mechanisms than fish oil, and their interactions with existing medications need careful consideration. For example, some supplements may affect blood clotting, potentially increasing the risk of bleeding or interfering with anticoagulants.
Comparison of Supplements to Fish Oil
| Supplement | Potential Benefits | Potential Drawbacks | Comparison to Fish Oil |
|---|---|---|---|
| Coenzyme Q10 | May improve heart function and reduce oxidative stress. | May interact with certain medications. | May complement fish oil’s effects on heart health, but mechanisms are different. |
| Magnesium | May help regulate heart rhythm. | Can cause diarrhea or other digestive issues in high doses. | May be beneficial for overall cardiovascular health, but not as directly linked to AFib as fish oil. |
| Vitamin D | May improve heart health and reduce inflammation. | High doses can be harmful. | Potentially synergistic in reducing inflammation, but mechanisms are different. |
| Omega-3 Fatty Acids (other sources than fish oil) | May reduce inflammation and improve heart health. | May interact with certain medications. | Similar benefits to fish oil, but source and dosage differences may impact effectiveness. |
Combining Fish Oil with Other Treatments
Combining fish oil with other treatments requires careful consideration of potential interactions. While fish oil is generally considered safe, combining it with anticoagulants, certain medications, or other supplements can sometimes increase the risk of bleeding or other adverse effects. Always consult with a healthcare professional to determine the safety and efficacy of any combined treatment plan.
Importance of Professional Consultation
It is crucial to remember that any changes to a treatment plan, including the addition or removal of supplements, must be discussed with a healthcare professional. They can assess individual needs, evaluate potential interactions, and provide personalized recommendations. Self-treating or altering a prescribed regimen without medical guidance can be harmful and potentially exacerbate underlying conditions. This is particularly true when considering the potential interactions between fish oil and other supplements or medications.
A healthcare provider can provide tailored guidance and ensure that any interventions align with the patient’s overall health status and other treatments.
Public Health Implications
Fish oil supplementation, while promising in some studies, presents complex public health implications regarding atrial fibrillation (AFib) prevention. Understanding these implications is crucial for informed recommendations and potential policy decisions. A thorough analysis considers the potential benefits, associated costs, and the need for further research before widespread adoption.The potential for cost-effectiveness in preventing AFib through fish oil supplementation is a significant consideration for public health initiatives.
Identifying the optimal dosage, duration of supplementation, and specific populations most likely to benefit is essential for maximizing the return on investment. This requires rigorous scientific investigation.
While researching fish oil supplements and their potential impact on atrial fibrillation (AFib) risk, I stumbled upon some interesting insights about dietary changes. It got me thinking about how changing your diet to cure psoriasis might have a similar effect on heart health. Changing your diet to cure psoriasis often involves focusing on anti-inflammatory foods, which could potentially reduce AFib risk factors.
Ultimately, more research is needed to definitively link these dietary changes to AFib risk, but it’s certainly a fascinating area to explore further.
Potential Cost-Effectiveness Analysis
The cost-effectiveness of fish oil supplementation in reducing AFib risk hinges on several factors. These include the cost of the supplements, the frequency of supplementation, the long-term health implications of AFib, and the projected reduction in AFib incidence. A critical evaluation needs to compare the cost of fish oil supplements with the potential healthcare costs avoided through reduced AFib cases.
This analysis should consider various factors like the potential for reducing hospitalizations, medication costs, and the overall quality of life improvement.
Limitations of Fish Oil Supplementation
While fish oil supplementation shows promise in some studies, several limitations must be considered. These include the potential for side effects such as gastrointestinal distress, allergic reactions, and interactions with other medications. Not all individuals respond equally to fish oil, and the effectiveness may vary depending on pre-existing health conditions. The variability in fish oil quality and composition can also impact efficacy.
Further research is crucial to fully understand these factors and their impact on the overall effectiveness of fish oil supplementation.
Need for Further Research
More robust, large-scale clinical trials are needed to establish the efficacy and safety of fish oil supplementation for AFib prevention in diverse populations. These trials should carefully evaluate the long-term effects, assess various dosages and durations, and compare fish oil supplementation to other preventative strategies. Specific populations, like individuals with pre-existing cardiovascular conditions, require dedicated study.
Public Awareness Campaigns
Public awareness campaigns are vital to educate the public about the potential benefits and risks of fish oil supplementation for AFib prevention. These campaigns should highlight the importance of consulting with healthcare professionals before starting any new supplement regimen. Information should emphasize the need for balanced diets and lifestyle modifications, in addition to potential supplements. Clear, accurate information is crucial to avoid misinterpretations and potentially harmful self-treatments.
Summary Table: Cost-Effectiveness of Fish Oil in AFib Prevention
| Factor | Potential Benefit | Limitations |
|---|---|---|
| Cost of Supplements | Relatively low compared to long-term AFib treatment | Variability in supplement quality and price |
| Reduction in AFib Risk | Potential for decreased incidence of AFib | Variability in individual response and effectiveness |
| Healthcare Cost Savings | Potential for decreased hospitalizations and medication costs | Long-term effects not fully understood |
| Side Effects | Potential for gastrointestinal issues or allergic reactions | Individual sensitivities vary |
| Overall Cost-Effectiveness | Promising, but further research needed for conclusive results | Requires large-scale clinical trials for definitive analysis |
Expert Opinions and Recommendations
Navigating the complex relationship between fish oil supplements and atrial fibrillation (AFib) requires expert insights. While preliminary research suggests a potential link, conclusive evidence is still emerging. This section summarizes expert opinions, highlights key recommendations from leading medical organizations, and emphasizes the crucial role of individual patient considerations.
Expert Consensus on Fish Oil and AFib Risk
Experts generally agree that more research is needed to definitively establish a causal link between fish oil consumption and AFib risk. Current evidence, while promising in some studies, is not consistent enough to recommend widespread use of fish oil supplements for AFib prevention or treatment.
Recommendations from Leading Medical Organizations
Leading medical organizations, such as the American Heart Association (AHA) and the American College of Cardiology (ACC), typically advise against relying on fish oil supplements alone for managing or preventing AFib. These organizations often recommend a holistic approach that includes lifestyle modifications, such as a balanced diet, regular exercise, and stress management, as cornerstone strategies for AFib prevention and management.
They emphasize that dietary supplements should not replace established medical recommendations.
“Dietary supplements, including fish oil, should not be used as a substitute for prescribed medications or lifestyle changes in the management of AFib.”
Hypothetical Statement from a Leading Medical Organization.
Individual Patient Considerations
Individual patient considerations are paramount. Factors such as pre-existing health conditions, medication use, and family history should be carefully evaluated by healthcare professionals before recommending any dietary supplement, including fish oil. For example, individuals with bleeding disorders might require specific caution when considering fish oil supplementation due to its potential blood-thinning effects. A personalized approach, tailored to each patient’s specific needs and medical history, is essential.
- Underlying health conditions: Patients with conditions like high blood pressure, diabetes, or kidney disease should consult their doctors before using fish oil supplements. These conditions can interact with fish oil’s effects on blood pressure or blood clotting.
- Medications: Individuals taking blood thinners or other medications should discuss the potential interactions with their doctor before using fish oil supplements. The interaction between fish oil and certain medications could be potentially dangerous.
- Family history: A family history of AFib might warrant a more cautious approach to fish oil supplementation, but this is not a contraindication in itself. Further discussion with a cardiologist is necessary to develop a comprehensive plan.
FDA Recommendations (if available)
The FDA’s stance on fish oil supplements and AFib risk is not currently available in a specific statement. The FDA primarily regulates the safety and labeling of dietary supplements. They do not typically issue specific recommendations for the use of supplements for specific health conditions.
Final Wrap-Up
In conclusion, while promising, the link between fish oil supplements and AFib risk remains somewhat inconclusive. Existing research presents some potential correlations, but more robust and conclusive studies are needed. This blog post has highlighted the complexities involved and the importance of considering various factors. Remember, individual responses to dietary supplements can vary, and consulting with a healthcare professional is crucial before making any changes to your treatment plan.
Ultimately, a balanced approach incorporating dietary changes, lifestyle modifications, and professional guidance is key to managing AFib risk.